The field of cardiovascular medicine has witnessed an important paradigm shift in the approach to revascularisation in patients with coronary artery disease (CAD). While coronary artery bypass grafting (CABG) was historically the favoured approach for revascularisation, advances in the percutaneous management of CAD have made this option an attractive alternative to CABG. There has been great interest in understanding how these two strategies compare and, to this end, multiple randomised clinical trials have been conducted. Most of these studies comparing CABG and percutaneous coronary intervention (PCI) have focused on relevant clinical endpoints, including myocardial infarction (MI), repeat revascularisation, stroke and mortality. However, major infections as an outcome measure have generally been excluded from the analysis in these studies, thereby potentially limiting our understanding of the comparative safety and efficacy of CABG and PCI.
The SYNTAX trial randomised 1,800 patients with multivessel and/or left main coronary artery disease to CABG or PCI with first-generation drug-eluting stents (TAXUS Express; Boston Scientific, Marlborough, MA, USA). The primary endpoint, a composite of death, stroke, MI and need for repeat revascularisation at one year, was observed in 17.8% in the PCI arm versus 12.4% in the CABG arm (RR 1.44, 95% CI: 1.15-1.81, p=0.002)1, driven by a higher rate of repeat revascularisation in the PCI group (13.5% vs 5.9%, RR 2.29, 95% CI: 1.67-3.14, p<0.001). Notably, CABG was associated with a significantly higher risk of stroke, whereas all-cause mortality and MI were comparable in both treatment groups. Results from the 10-year follow-up showed no significant difference in all-cause mortality between CABG and PCI, including high-risk subgroups such as diabetes or left main disease2. Other contemporaneous studies have shown similar findings: over the long term, PCI is associated with a greater risk of repeat revascularisation and MIs, whereas CABG has a higher risk of periprocedural events, including death, MI and stroke3,4,5,6.
In this issue of EuroIntervention, Mancone et al7 present an analysis of the SYNTAX trial, focusing on major infections in patients undergoing CABG or PCI.
Over a five-year follow-up period, 186 (10.3%) patients had one or more major infections, and major infections were independently associated with a higher risk of death (HR 2.6, 95% CI: 1.8-3.8; p<0.001). In the CABG group, major infections occurred in 15.8% of patients, the majority of which were procedure-related (within hospitalisation or within 60 days of the index procedure). The most common infections were deep surgical site (10.7%), pneumonia (3.9%) and bloodstream infections (2.5%). An astute surgeon may note that this rate of deep surgical site infection is much higher than contemporary reports (deep sternal wound infection rate 0.8 to 5.0%). This is probably in part due to the inclusion of infection at the saphenous vein harvesting site in addition to infection at the primary sternotomy incision in the definition. Contrary to findings from other studies, bilateral internal thoracic artery use and diabetes were not associated with higher risk of infection8,9. An association between major infections and mortality has been reported previously and is affirmed by the findings of the present analysis10. One of the most feared complications of CABG, deep sternal wound infection, carries a 14% perioperative mortality rate and is associated with adverse five-year survival11,12,13.
The observed rate of major infections in the PCI arm was 4.9%. An astute interventional cardiologist may note that this rate is disproportionately higher than the <1% expected rate of infection. The most common infections in the PCI arm were pneumonia (3.2%), deep surgical site infection (1.2%) and blood stream infection (1.2%). The major driver of infection in the PCI arm was the need for CABG, either during index hospitalisation or during follow-up (for repeat revascularisation). Excluding patients who underwent CABG in the PCI group, the rate of deep surgical site infection (presumably access site-related) was low (0.8%). The use of the radial access site for cardiac catheterisation was low in the trial and, as such, the rates of access-site infection associated will be lower with the continued adoption of the radial approach. Of note, the most common infection related to PCI, even after excluding patients who underwent CABG, was pneumonia (3.0%). It is unlikely that cardiac catheterisation is causally linked to pneumonia and is more likely due to patient comorbidities. The risk factors for PCI-associated infection were need for CABG, peripheral vascular disease and older age.
The analysis by Mancone et al presents two key findings: 1) the risk of major infections was eight times higher with CABG than with PCI within 60 days of the procedure, and 2) major infections, whether with CABG or with PCI, are not benign and are associated with increased length of stay and increased mortality. What then is the current risk/benefit equation for CABG versus PCI for multivessel disease (Figure 1)? Most trials show that the upfront risk of procedure-related complications (including infections) is higher with CABG when compared with PCI and that the recovery time is longer with CABG than with PCI. Most trials also consistently show that PCI is associated with increased long-term risk of repeat revascularisation. The impact on outcomes of MI and death is more controversial. Few trials have shown a higher risk of MI with PCI than with CABG4, but in a few of the analyses the gap is narrowed if there is complete revascularisation with PCI3. Very few trials have shown a difference in long-term death favouring CABG6 but other trials/analyses including longer-term follow-up have failed to show this benefit2,14. Finally, given that PCI only targets significant lesions, the long-term outcome with PCI is dependent on the patients’ ability to comply with guideline-directed medical therapy which targets both significant and less significant lesions. There are challenges in the application of clinical trial results to day-to-day practice: 1) there is no simple way to apply trial-level results to patient-specific risks versus benefits, and 2) oversimplification of results ignores the patient-specific values of a particular endpoint (for example, death versus stroke). In recent years, the scientific community has aimed its efforts at understanding the merits and shortcomings of CABG and PCI. In doing so, the focus was placed on adverse cardiovascular events after each respective approach to revascularisation. It is clear that non-cardiovascular events that are not routinely captured in randomised clinical trials have a profound impact on patient outcomes, including mortality, after revascularisation. It is imperative that future studies include clinically relevant non-cardiovascular events in their analysis so that physicians and patients can make the most informed decision with regard to the optimal revascularisation strategy (Figure 1).
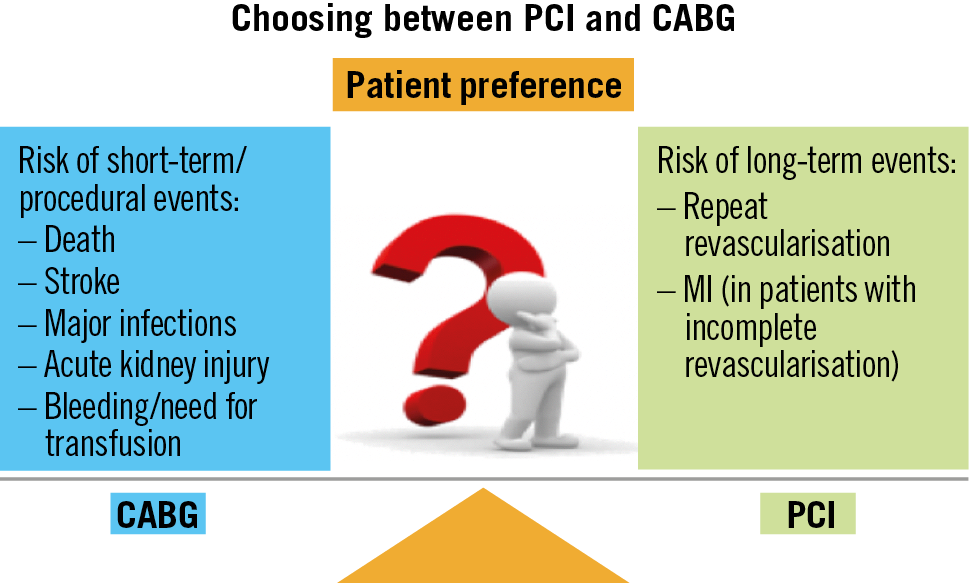
Figure 1. Weighing risks and benefits of CABG versus PCI for multivessel coronary disease.
Conflict of interest statement
S. Bangalore reports being an ad hoc consultant/speaker for Abbott Vascular, Biotronik, Meril, Pfizer, Reata, and Amgen, and has received research grants from Abbott Vascular and NHLBI. The other author has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.