Abstract
Aims: Incidence, associated risk factors and impact on mortality of infections after bypass surgery (CABG) and stenting (PCI) for multivessel coronary disease (MVD) have never been reported in a large randomised trial. The aim of the present study was to evaluate, in patients with MVD, the prevalence of major infections after PCI and CABG and to assess their impact on mortality.
Methods and results: The SYNTAX trial randomised 1,800 MVD patients to either CABG or PCI. Patients were followed up to five years. The primary endpoint of this post hoc analysis was the occurrence of major infection. At five years of follow-up, the primary endpoint had occurred in 142 (15.8%) patients in the CABG arm and 44 (4.9%) patients in the PCI arm (≤60 days HR – 7.9, 95% CI: 4.7 to 13.1; p<0.001) (>60 days – HR 0.79, 95% CI: 0.44 to 1.44; p=0.45). Major infections were independently associated with a higher risk of all-cause mortality at five years (adjusted HR 2.6, 95% CI: 1.8 to 3.8, p<0.001).
Conclusions: CABG is associated with a higher incidence of post-procedure major infections compared to PCI. Major infections are independently associated with all-cause mortality.
Introduction
In patients with multivessel coronary artery disease (CAD) requiring revascularisation, the choice between percutaneous coronary intervention (PCI) and coronary artery bypass graft surgery (CABG) involves a complex multidisciplinary decision-making process1. This process is usually based on ischaemic outcomes, which are always the main endpoints assessed in major randomised trials2,3.
These trials have shown that, while PCI can be used for less anatomically complex disease, CABG is associated with better long-term ischaemic outcomes in patients with higher anatomic complexity, i.e., higher SYNTAX scores1,2,3. Of note is the fact that the bulk of the difference in these outcomes is related to a more frequent need for repeat revascularisation procedures after PCI, with mortality being similar between the two strategies4.
One clear difference between CABG and PCI is the obviously greater invasiveness of cardiac surgery compared to the percutaneous vascular access of PCI. This leads to a perceived risk of infection that is much higher for CABG5,6. Interestingly, this risk of infection after surgery is related to a high clinical risk profile, which might also be related to the occurrence of multivessel CAD of higher complexity, where CABG performs better than PCI in terms of ischaemic outcomes7. Furthermore, it has been shown that patients suffering from post-CABG major infections are at increased risk of death5,6,7,8.
Reports on post-CABG infection events come from surgery trials or registries; post-PCI infections are rarely described. Furthermore, since PCI is associated with a more frequent need for repeat revascularisation procedures due to stent failure, and some of these repeat revascularisations are performed with CABG, it is possible to speculate that in an intention-to-treat analysis the PCI arm would also be subject to a high risk of infection. To the best of our knowledge, no large randomised trial comparing PCI and CABG in multivessel CAD has provided a detailed report on the occurrence and clinical impact of infection events. Therefore, the aim of the present study was to assess the prevalence of infections after PCI and CABG, identify their risk factors, and assess their effect on intermediate-term mortality in the context of a landmark randomised trial of patients with multivessel CAD.
Methods
STUDY POPULATION
The design and methods used in the SYNTAX trial were previously published elsewhere9,10. In brief, it was a multicentre, multinational, open-label, randomised controlled trial that enrolled 1,800 patients with multivessel and/or left main (LM) coronary artery disease in 85 sites in Europe and the USA. Patients were randomised to undergo either CABG or PCI and were followed for five years2. All patients provided written informed consent before enrolment.
ASSESSMENT AND DEFINITIONS OF INFECTION EVENTS
All infection events were recorded on a specific section of the electronic report forms as study adverse events by each site investigator. For the present analysis, the complete closed five years SYNTAX trial database was retrospectively reviewed. All 7,082 adverse events reported in the trial were scrutinised and all infection events were independently assessed by a clinical events committee composed of one clinical cardiologist (E. Spitzer), one cardiac surgeon (U. Benedetto) and one infectologist (M. Falcone), all of whom were blinded for study arm and outcomes.
Infection events were described in agreement with previous reports of post-CABG infections and defined according to standard CDC/NHSN criteria11,12. The primary objective of the present analysis was to assess the occurrence of major infections in the CABG and PCI arms. Major infection was defined as the occurrence of deep incisional surgical site infection occurring at the primary chest incision or at a secondary incision site (e.g., saphenous harvest and groin cannulation sites), mediastinitis, infectious myocarditis or pericarditis, endocarditis, cardiac device infection, pneumonia, empyema, clostridium difficile colitis, and bloodstream infection at any time point during the five-year follow-up period as reported by the investigators11,12,13.
Secondary objectives were to assess the relationship between the occurrence of major infection and mortality and to describe the risk factors for major infections in both study arms.
STATISTICAL ANALYSIS
Categorical variables are presented as counts and percentages and compared with chi-square tests. Continuous variables are presented as mean±standard deviation and compared with the Student’s t-test. Major infections during the follow-up period were assessed with time-to-first-event analysis by the Kaplan-Meier method using the day of the procedure as day zero. The PCI and CABG arms were compared using a Cox proportional hazards model. The proportional hazards assumption was assessed using a time-dependent Cox model. Since this assumption was violated, the follow-up was divided into two time points, ≤60 days post procedure and >60 days up to five years post procedure. Hazard ratios, confidence intervals and p-values were described for both time points.
To assess the effect of major infection on mortality, univariable and multivariable Cox models were created with major infection treated as a time-dependent variable. In the multivariable model, the following variables were forced into the model to adjust for possible confounders – age, gender, creatinine clearance <60 ml/min, SYNTAX score, EuroSCORE, diabetes, peripheral vascular disease (PVD), chronic obstructive pulmonary disease (COPD), left ventricular ejection fraction (LVEF in %), body mass index (BMI in kg/m2), and study arm. This relationship was further assessed using the Mantel-Byar test and graphically represented with the Simon-Makuch survival plot.
For the description of the risk factors for major infection, variables associated with major infection in both arms with a p-value <0.10 on univariable analysis were included in a multivariable Cox proportional hazards model. In the CABG multivariable model, age and diabetes were included despite the non-significant p-values on univariable analysis. Similarly, in the PCI arm, diabetes was also included in the multivariable model despite the lack of association on univariable analysis.
All analyses were performed according to the intention-to-treat principle. Two-sided values less than 0.05 were considered statistically significant. SPSS, Version 21 (IBM Corp., Armonk, NY, USA) and R v3.3.2 (R Foundation for Statistical Computing, Vienna, Austria) were used for all analyses.
Results
STUDY POPULATION
In the SYNTAX trial, 903 and 897 patients were randomised to PCI and CABG, respectively. Complete five-year follow-up data were available for 805 (89.7%) patients in the CABG arm and 871 (96.5%) in the PCI arm. Baseline characteristics according to study arm have been described previously elsewhere10.
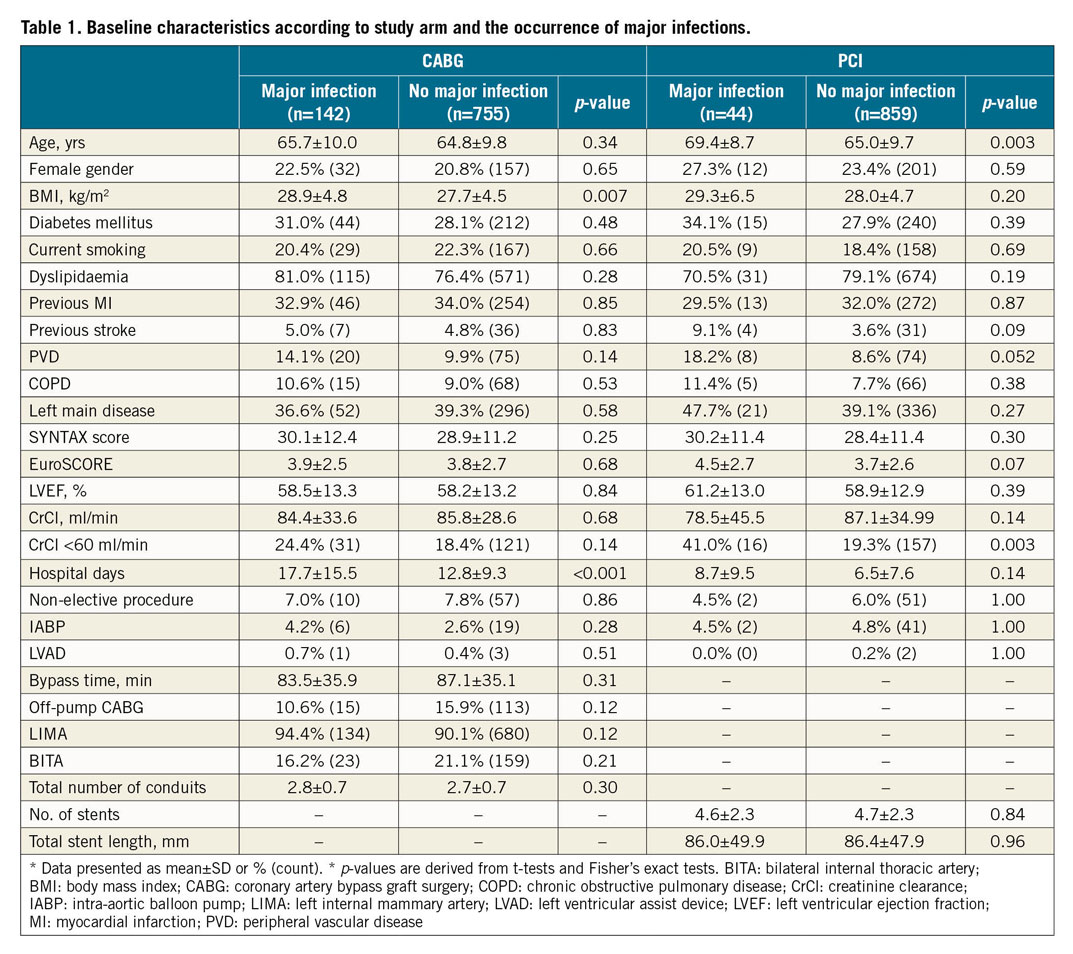
In the CABG group, patients with major infection had higher body mass indices (BMI) and had longer hospital stays than patients without major infections (Table 1). In the PCI group, patients who had major infections were older, and had a higher prevalence of peripheral vascular disease and renal failure than patients without infections (Table 1).
INCIDENCE OF INFECTIONS
Overall, 214 major infections occurred in 186 (10.3%) of the 1,800 patients randomised in the SYNTAX trial during the five years of follow-up – 142 (15.8%) patients in the CABG arm and 44 (4.9%) in the PCI arm (Table 2, Figure 1). CABG was associated with an almost eightfold increase in the rate of major infection as compared to PCI within the first 60 days post procedure (HR 7.87, 95% CI: 4.73 to 13.06; p<0.001) (Figure 1). After 60 days, Kaplan-Meier curves of major infections after CABG and PCI were parallel, with no difference between the two strategies (HR 0.79, 95% CI: 0.44 to 1.44; p=0.45) (Figure 1).
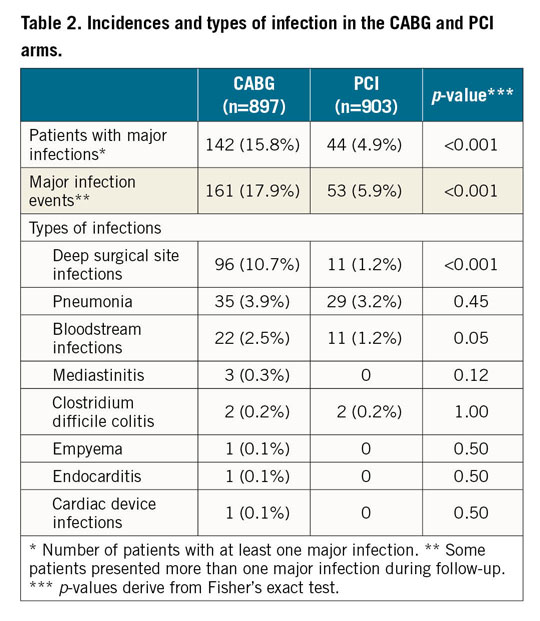
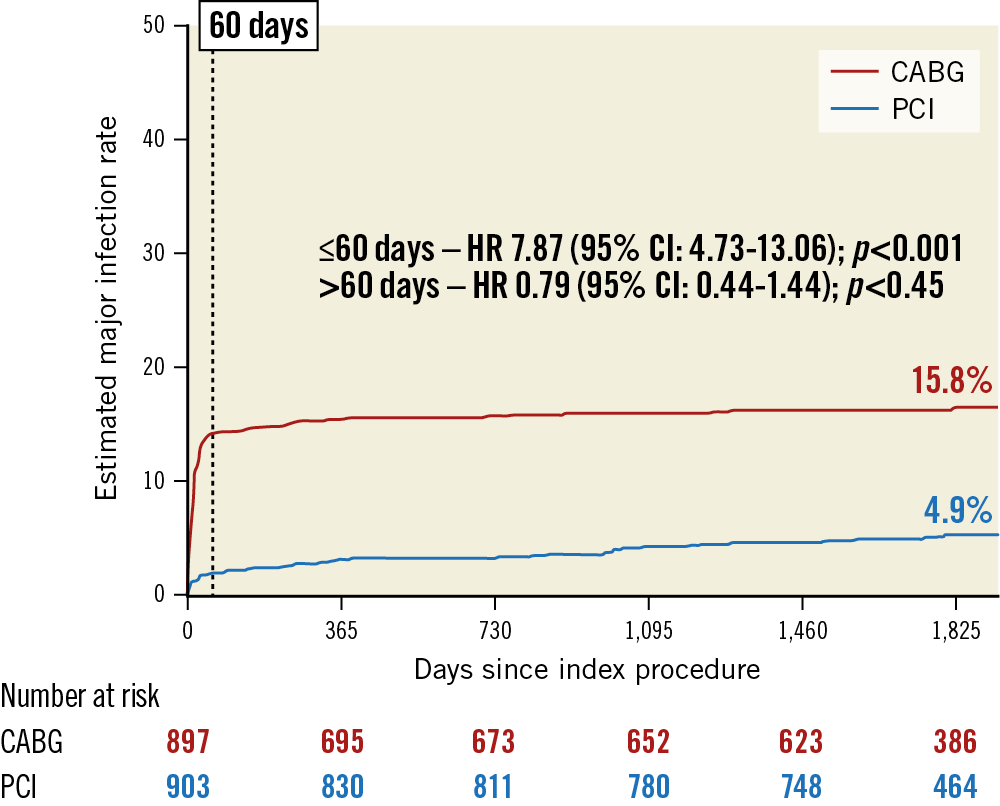
Figure 1. Five-year Kaplan-Meier curves of major infection. Five-year Kaplan-Meier estimates and Cox hazard ratios for the rates of major infection in CABG and PCI arms. Hazard ratios for the first 60 days and after 60 days after the index procedure are provided. CABG: coronary artery bypass graft surgery; HR: hazard ratio; PCI: percutaneous coronary intervention
A total of six patients in the PCI arm had major infections after undergoing CABG. One patient had a deep sternal infection at day 10 post procedure after undergoing CABG despite randomisation for PCI due to crossover, and five patients had major infections after CABG for repeat revascularisation during follow-up (three deep sternal infections, two pneumonias and one bloodstream infection). In the CABG arm, all cases of deep surgical site infection and mediastinitis occurred following the index procedure.
Overall, the most common major infections were deep surgical site infections (10.7%), pneumonia (3.9%) and bloodstream infections (2.5%) in the CABG group, and pneumonia (3.2%), bloodstream infections (1.2%) and deep surgical site infections (1.2%) in the PCI group (Table 2). CABG was associated with a significantly higher occurrence of deep surgical site infections (p<0.001) than PCI (Table 2).
INFECTIONS AND SURVIVAL
The occurrence of major infections was associated with a higher risk of all-cause mortality (unadjusted HR 2.5, 95% CI: 1.8-3.5; p<0.001). The association remained significant even after adjustment for several possible confounders (adjusted HR 2.6, 95% CI: 1.8-3.8; p<0.001) (Figure 2).
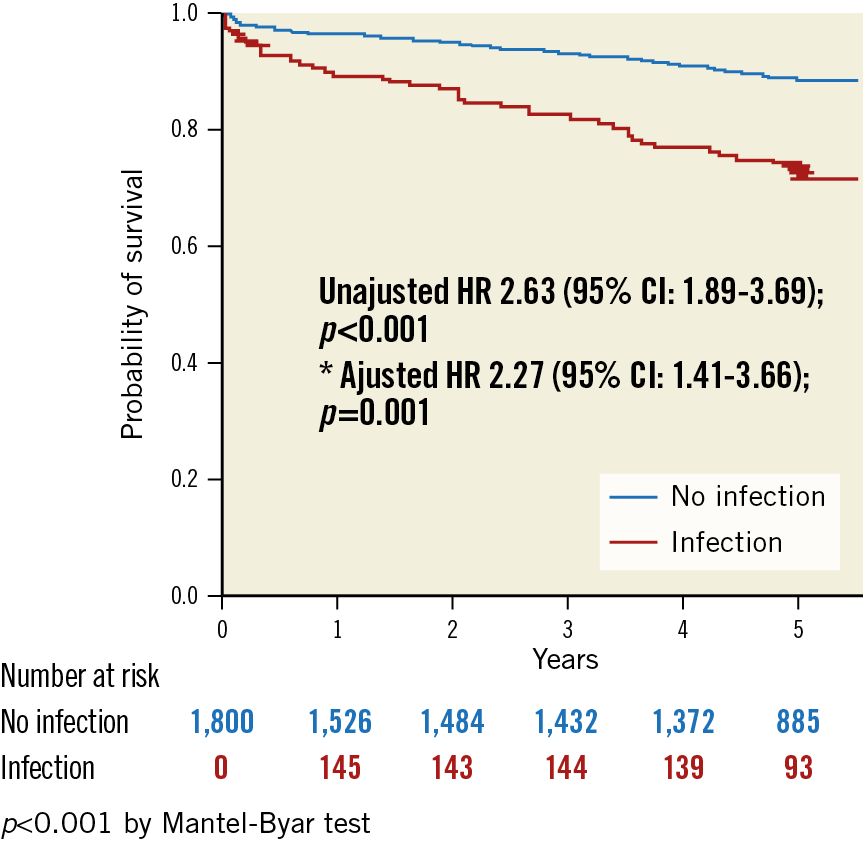
Figure 2. Simon-Makuch survival plot in patients with and without infections. Simon-Makuch survival plot for the association between major infections and the occurrence of all-cause death at five years. Hazard ratios are derived from time-dependent Cox models with infection treated as a time-dependent variable. HR: hazard ratio
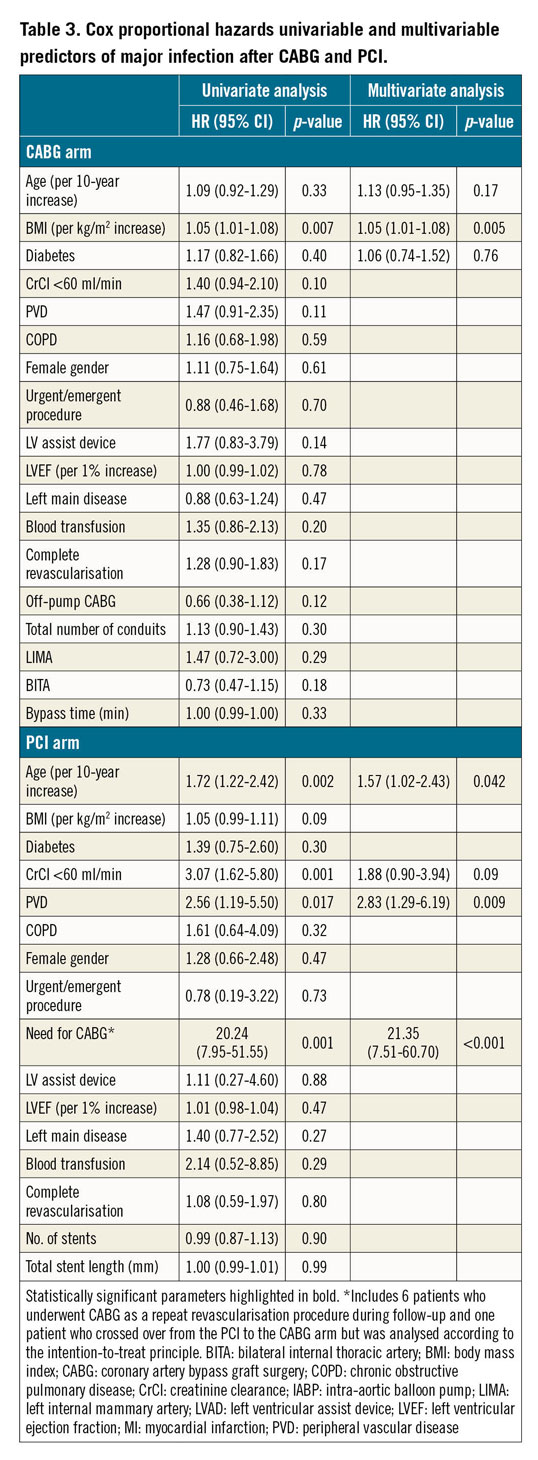
RISK FACTORS FOR INFECTIONS
In the CABG group, high BMI was the only independent predictor of major infections (Table 3). In the PCI arm, advanced age, peripheral vascular disease, and the need for subsequent CABG were independently associated with major infection (Table 3).
Discussion
We report for the first time the incidence, predictors and clinical impact of infection events after PCI and CABG in patients with multivessel CAD, in the context of a large randomised controlled trial. The findings of the present study can be summarised as follows: 1) CABG is associated with a higher incidence of major infections within 60 days post procedure than PCI; 2) major infections are independently associated with long-term all-cause mortality; 3) high BMI is an independent predictor of major infections after CABG; 4) advanced age, PVD, and the need for subsequent CABG are independently associated with major infections after PCI; and 5) patients with infections after revascularisation present higher clinical risk profiles.
Due to its invasive nature, cardiac surgery is more frequently associated with infectious complications than percutaneous procedures14. Several registry studies have reported varying infection rates after CABG6,7,8,11. Patients included in these reports represent heterogeneous populations including patients with single- or two-vessel disease with low overall risk profiles. On the other hand, reports on post-PCI infection events are quite scarce in the literature15. Interestingly, since PCI has received an equal degree of recommendation (class I recommendation) to CABG for single- and two-vessel CAD, it is in the three-vessel and left main disease population that PCI is still compared to CABG in randomised trials. Indeed, these trials currently represent the best opportunity to compare infection rates after both revascularisation modalities1.
INCIDENCE AND PREDICTORS OF INFECTION
In our study, only three-vessel disease (3VD) and/or LM disease patients were included. These patients have an overall high-risk profile. It is therefore not unexpected that we observed relatively high infection rates as compared to data in the literature7. Furthermore, we report all events occurring during index hospitalisation as well as during follow-up, although, as depicted in the Kaplan-Meier curve (Figure 1), most infection events were procedure-related and occurred in the hospitalisation period or within 60 days of the index procedure. Importantly, our data are consistent with those of the recent EXCEL trial that reported similar infection rates, although definitions between the two trials may be somewhat different16.
In agreement with previously published data, we showed that high BMI is related to the occurrence of infection after surgery17. The use of bilateral internal thoracic artery (BITA) grafts and diabetes were not found to be associated with a higher risk of major infection (Table 3). While data in the literature have shown that BITA grafts were safe in terms of infections, the recently published ART trial suggested that this strategy increased the risk of wound infection in patients with diabetes and high BMI18,19,20. In the PCI arm, few data are available regarding the prevalence and predictors of infection. We found that age, PVD and need for subsequent CABG were independently associated with major infections. For MVD patients with any of these characteristics undergoing revascularisation, special attention regarding the risk of infection is warranted.
INFECTION AND MORTALITY
The most important finding of the present analysis is the independent association between major infection and mortality. Interestingly, the risk of dying during long-term follow-up more than doubled for patients who had a major infection event post procedure compared to those who did not have infections. This difference appeared to increase over time, as shown by the diverging cumulative survival curves (Figure 2). Although the reasons for this long-term effect on mortality are still unclear, this finding is consistent with a recent report on infection and mortality after cardiac surgery in which patients discharged after surgery had higher long-term mortality if they had had infection after the procedure7.
It is important to acknowledge that our data do not provide a causal explanation for the relationship between infection and death. Our analysis shows a strong association that remains significant after adjusting for several possible confounders7,8,9,10,11. Furthermore, the fact that survivors of postoperative infections continue to die during long-term follow-up might be related to the intrinsic frailty of these patients. It may also represent some sort of sequelae following the infective disease. This phenomenon was also observed for other conditions in the SYNTAX trial. Patients with COPD, for instance, present a higher risk of death even after surviving the surgical procedure21.
Overall, five-year all-cause mortality rates in the CABG and PCI arms of the SYNTAX trial were similar, even though CABG patients had more infections and infections were related to mortality. This can be partially explained by the fact that, in the PCI arm, patients had more myocardial infarctions; this was also shown to be related to mortality22. In SYNTAX, PCI was associated with a higher rate of fatal myocardial infarctions as compared to CABG (2.7% vs 0.6%, p<0.001). Indeed, cardiovascular mortality represented 67.5% of all deaths in the PCI arm and 49.5% in the CABG arm, while non-cardiovascular mortality represented 32.5% in the PCI arm and 50.5% in the CABG arm2,22.
Limitations
The main limitation of the present study is that it is a post hoc analysis of the SYNTAX trial, and hence merely hypothesis-generating. Nevertheless, we set up a new independent clinical events committee which carefully reviewed all events reported by the investigators and finally adjudicated the major infections. Additionally, the magnitude of difference in infections encountered between the two treatment strategies and the analysis of major infection rather than any infection support the robustness of the findings.
Conclusions
Even though a higher infection rate after CABG compared to PCI is an expected finding, to the best of our knowledge this is the first large randomised trial to report it. Furthermore, the long-term follow-up and the assessment of infections in a time-to-event fashion provide important new insight on the topic. CABG is associated with a higher risk of overall and major infections compared to PCI. Major infections are independently associated with long-term all-cause mortality. High BMI is an independent predictor of major infections after CABG. Advanced age, PVD, and need for subsequent CABG are independent predictors of major infections after PCI.
|
Impact on daily practice The present study describes for the first time the size of the difference in major infection rates between CABG and PCI for the treatment of multivessel coronary disease in a randomised fashion. It demonstrates the impact of major infections on mortality and describes its risk factors separately for both revascularisation strategies. The results will impact significantly on the decision-making process of the Heart Team regarding the choice of revascularisation modality for each individual patient. |
Guest Editor
This paper was guest edited by Alec Vahanian, MD, PhD; Department of Cardiology, Hôpital Bichat-Claude Bernard, and University Paris VII, Paris, France.
Funding
The SYNTAX trial was funded by Boston Scientific.
Appendix. Study collaborators
Marie-Claude Morice, MD; Institut Hospitalier Jacques Cartier, Generale de Sante, Massy, France; David R. Holmes Jr, MD; Mayo Clinic Rochester, Rochester, MN, USA; Pedro A. Lemos, MD, PhD; Hospital Israelita Albert Einstein, Sao Paulo, Brazil; Gennaro Sardella, MD; Department of Cardiovascular, Respiratory, Nephrology, Anesthesiology and Geriatric Sciences, Sapienza University of Rome, Rome, Italy; Francesco Fedele, MD; Department of Cardiovascular, Respiratory, Nephrology, Anesthesiology and Geriatric Sciences, Sapienza University of Rome, Rome, Italy; Marie-Angèle Morel, BSc; Cardialysis B.V., Rotterdam, the Netherlands; Carlos Collet, MD; Department of Cardiology, Amsterdam University Medical Center, Amsterdam, the Netherlands; Ewout W. Steyerberg, PhD; Erasmus University Medical Center, Rotterdam, the Netherlands.
Conflict of interest statement
R. Modolo has received a research grant from the Sao Paulo Research Foundation (FAPESP – grant number 2017/22013-8). R. Cavalcante is an employee of Boston Scientific. G. Biondi-Zoccai has consulted for Abbott and Bayer. Y. Onuma has served as an advisory board member for Abbott Vascular. P.W. Serruys reports personal fees from Abbott Laboratories, AstraZeneca, Biosensors, Biotronik, Cardialysis, HeartFlow, GLG Research, Medtronic, Sino Medical Sciences Technology, Société Europa Digital & Publishing, Stentys France, Svelte Medical Systems, Philips/Volcano, St. Jude Medical, Qualimed and Xeltis, outside the submitted work. E. Blackstone reports grants from Medstar, and grants from NIH, outside the submitted work. The other authors have no conflicts of interest to declare. The Guest Editor is a consultant for Edwards Lifesciences.
Supplementary data
To read the full content of this article, please download the PDF.