Abstract
Aims: We sought to evaluate the prognostic impact of age on the procedural results and subsequent clinical outcomes in patients with multivessel disease (MVD) treated either by coronary artery bypass surgery (CABG) or by percutaneous coronary intervention (PCI) with or without drug eluting stents, based on data of the Arterial Revascularisation Therapies Study (ARTS) part I and part II. The potential influence of age in determining the most appropriate revascularisation strategy for patients with MVD is largely unknown.
Methods and results: Three year clinical outcome of ARTS I patients randomised to PCI with bare metal stent (BMS) (n= 600) or CABG (n= 605), and matched patients treated by PCI with sirolimus-eluting stents (SES) in ARTS II (n= 607) were reviewed according to four age quartiles. Endpoints were measured in terms of major adverse cardiac and cerebrovascular events MACCE) during hospital stay and up to three years. The frequency of female, diabetes, hypertension, peripheral vascular disease, pulmonary disease, as well as lesion complexity increased with age. At three years, MACCE free survival was comparable between patients treated by CABG or SES PCI, regardless of age quartile. The incidence of MACCE was higher among ARTS I BMS treated patients in all but the second age quartile. This was primarily related to a higher need for repeat revascularisation among BMS treated patients. However, age, which emerged as a strong independent predictor of MACCE following CABG (p<0.005), was not predictive of adverse events following PCI. Conversely, diabetes was the strongest independent predictor of MACCE among PCI treated patients (p<0.02), but didn’t affect three-year outcomes following CABG.
Conclusions: Age seems to influence the CABG outcome in-hospital but not PCI. PCI-SES could offer lower immediate risk in patients with MVD and comparable long-term outcome as CABG especially in older patients. The worst outcome of PCI-BMS group is primarily related to the need for repeat revascularisation. Diabetes is the most important predictor of MACCE following PCI.
Introduction
Coronary artery disease (CAD) is the leading cause of mortality worldwide. The prevalence of CAD increases with age, and this coupled with increasing life expectancy has led to a sharp rise in the number of elderly patients undergoing percutaneous coronary intervention (PCI) and coronary artery bypass grafting surgery (CABG).1 In comparison to their younger counterparts, older patients with CAD usually present with more diffuse atherosclerosis and a higher plaque burden.2 In addition non-cardiac co-morbidities such as renal insufficiency and impaired pulmonary function are also more prevalent with increasing age. This high risk profile of elderly CAD patients contributes to their increased complication rates, both after PCI3 and CABG.4 Consequently, numerous clinical studies have confirmed that a correlation exists between clinical outcomes from either method of revascularisation, and the patient’s age.5-9 On the other hand elderly patients have been shown to derive more benefit from invasive coronary revascularisation than from optimal medical therapy,9-11 and one study9 even concluded that elderly patients have a greater absolute risk reduction associated with revascularisation in comparison with younger patients. The most appropriate revascularisation procedure for older or younger patients remains controversial, primarily through the lack of clinical studies investigating a direct comparison of both treatment strategies.
The objective of the current investigation was to examine the prognostic impact of age on the procedural results, and subsequent early and late clinical outcomes in a contemporary cohort of patients with MVD treated by either CABG or PCI with or without drug eluting stents (DES).
Methods
Study population and protocol
The present study is a retrospective analysis of the ARTS I and II trials; the detailed protocols of both have been previously reported.12,13
Briefly, the study population includes the 1,205 patients from the ARTS-I study who were randomised to either bare metal stent (BMS) implantation (n=600) or CABG (n=605), and the 607 patients from the ARTS-II registry who were treated by sirolimus-eluting stent (SES) implantation. In order to obtain a population comparable to ARTS-I, patients in ARTS-II were stratified per clinical site in order to ensure that at least one third of the included patients had triple vessel disease. All inclusion and exclusion criteria were the same for both trials, including the upper age limit, which was 80 years old. Patients were enrolled irrespective of whether they had stable or unstable angina or silent ischaemia. They were required to have MVD and at least one other significant lesion (>50% diameter stenosis) in a different major epicardial artery suitable for stent implantation. Specific exclusion criteria included: patients with any prior coronary intervention, left main stem coronary disease, left ventricular ejection fraction of less than 30%, overt heart failure, history of a cerebrovascular accident, transmural myocardial infarction in the preceding week, severe hepatic or renal disease and the need for concomitant major surgery. All patients gave written informed consent.
The pooled population of ARTS-I and ARTS-II was divided into four equal quartiles of 453 subjects based on age at trial inclusion. The first, second, third and fourth quartiles (mean±SD) consisted of patients <54 years (48.8±4.8 years), 54-62 years (58.5±2.1 years), 62-68 years (65.6±1.9 years), and 68-83 years old (73.3±3.1 years) respectively. Five patients (3 in ARTS I and 2 in ARTS II) older than 80 years were included.
Data analysis and endpoints
Clinical outcomes in each subgroup were compared according to the assigned treatment, (CABG, PCI with BMS or PCI with SES) and analysis was performed on the outcome of each revascularisation procedure according to age quartiles. The primary endpoint was defined as the absence of any of the following major adverse cardiac and cerebral events (MACCE) within three years of inclusion in the trial: death (all-cause mortality), cerebrovascular accident, non-fatal myocardial infarction (MI), or any repeat revascularisation (either PCI or CABG).12,14,15 MACCE rate during hospital stay and at three years is assessed according to hierarchical classification. In hierarchical classification, only the worst event was counted as an event. Single adverse events are reported in a non-hierarchical way. Events for the present report were counted from the time of procedure for all the three arms. Complete three-year follow-up was available for all of the 1,812 study patients.
Statistical analysis
Statistical analysis was performed with SAS 6.12 software (SAS Institute Inc., Chicago, IL, USA). Continuous variables are expressed as mean±standard deviation (SD) and compared with use of Student’s unpaired t-test. Categorical variables were reported as counts and percentages and compared using the Fisher’s exact test for pair wise variables or the Chi-square for trend to examine the impact of age. Longitudinal event rates were evaluated using Kaplan-Meier estimates and compared with the log-rank test. To examine the impact of age in each treatment strategy, Cox Proportional Hazard models in SAS V8.2 was used. Both the age and the treatment subgroups were tested for interaction with predictor variables. This analysis was restricted to the MACCE. For the interaction tests between predictor variables and age group or treatment group, a likelihood ratio test was used by subtracting the summed -2log(L) of the “by group” analysis from the -2log(L) of the stratified (by age and by treatment) analysis, and comparing the outcome with a Chi-square distribution with the correct number of degrees of freedom. In case of a p-value <0.05 for the interaction, the “by group” analysis regression parameters were used.
Results
Baseline characteristics
Three patients died while waiting for surgery, and were subsequently excluded from the clinical outcome evaluation. Six patients initially assigned to BMS implantation were instead treated by surgery, and 19 patients initially assigned to surgery were instead treated with BMS. One patient assigned to stenting, and four patients assigned to surgery received only medical treatment. All patients assigned to SES implantation were treated according to protocol.
The patient population between both trials was not matched, and consequently the mean age of patients in the ARTS-II trial which was 63±10 years is slightly higher than that of the patients in the ARTS-I trial, whose mean ages were 61±9 years and 61±10 years for CABG and PCI, respectively. The patients included in the ARTS-II registry had more complex lesions and anatomy as has been previously reported.16
Table 1 shows the baseline demographic and clinical characteristics of the enrolled patients.
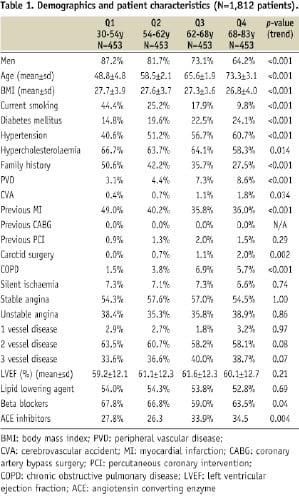
Increasing age is associated with an increased prevalence of diabetes mellitus, hypertension, peripheral artery disease, previous carotid artery surgery or cerebrovascular events, and chronic obstructive pulmonary disease. Conversely, the incidence of hypercholesterolaemia, obesity, family history of MI or sudden death, previous MI and current smoking, as well as the percentage of males in the population were found to decrease with advanced age. In all quartiles, the majority of patients presented with stable angina.
Procedural characteristics are depicted in Table 2.
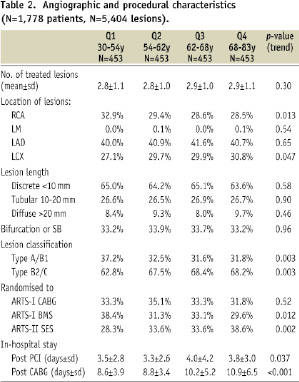
As patients included in ARTS had to be amenable for PCI or CABG, it is not surprising that the number of lesions treated was not influenced by age and was similar in patients assigned to CABG or stent implantation. The left anterior descending artery was equally revascularised within each age subgroups and more complex lesions were noted in older patients.
Based on the clinical and demographic data the calculated logistic EuroSCORE for each subgroup was 1.27±0.58, 1.33±0.58, 2.07±1.10 and 3.58±1.95, respectively. Finally, the average hospital stay increased with age and was longer among patients treated surgically.
In-hospital clinical outcome
In-hospital death and MACCE for each assigned treatment are presented in Table 3 according to age quartile.
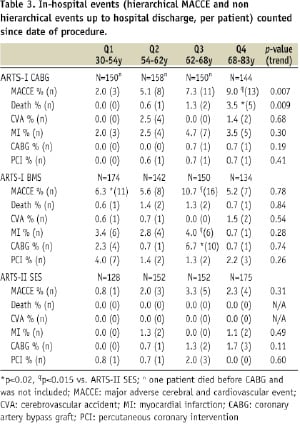
There was an age related increase in mortality and MACCE in patients treated surgically. The in-hospital mortality observed in these patients was comparable to the predicted mortality estimated by the EuroSCORE. Conversely, age had no significant influence on the in-hospital outcomes of patients assigned to percutaneous treatment, either with BMS or DES. In the youngest quartile (Q1) of patients assigned to BMS there was an excess MACCE as compared to SES PCI, which was primarily due to the increased repeat revascularisations, and myocardial infarctions in the BMS subgroup (p=0.016). However, we may speculate that this observation is related to improvements in ARTS-II PCI techniques and medical management. In the oldest quartile (Q4) patients treated by SES PCI had less MACCE as compared to surgically treated patients (2.3% vs. 9.0%, p=0.011); which was predominantly driven by a reduction in mortality (0.0% vs. 3.5%, p=0.018).
Three-year clinical outcome
Patient mortality increased with age and this trend was significant for patients assigned to CABG and SES PCI (Table 4).

A trend noted only in those patients having PCI was the increasing incidence of cerebrovascular accidents with increasing age. Not surprisingly, the need for repeat revascularisation was higher among PCI treated patients in all age quartiles when compared to surgery. However, the need for repeat PCI and CABG was dramatically reduced in ARTS-II SES treated patients by 60.8%, 26.9%, 59.6% and 45.4% in Q1, Q2, Q3 and Q4, respectively, as compared to ARTS-I BMS treated patients. The need for repeat revascularisation was not age-dependent.
The 3-year event free survival in each treatment arm is depicted in Figure 1 according to age quartile. In brief, there was no significant difference in MACCE rate between patients allocated to CABG or SES PCI with similar outcomes noted for each age group.
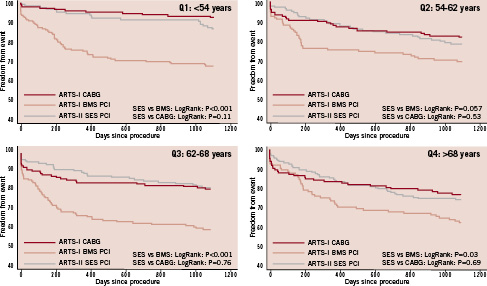
Figure 1. Kaplan-Meier curve to three years showing freedom from major adverse cardiac and cerebrovascular event (MACCE) according to age quartile in patients assigned to coronary artery bypass surgery (CABG), percutaneous coronary angioplasty with bare metal stent (BMS) and percutaneous coronary angioplasty with sirolimus-eluting stent (SES).
Conversely, the increased need for repeat revascularisation, specifically during the first year, resulted in a worse event free survival for ARTS-I BMS treated patients.
Impact of age on event free survival
A multi-variable analysis was conducted to determine the influence of age on outcome at three-years follow-up. Age together with hypertension and multiple long diffuse lesions were independent predictors of MACCE amongst surgically treated patients. In patients treated with SES PCI the presence of diabetes was the strongest independent predictor of MACCE, together with the absence of hypertension, a small number of lesions treated, and procedural duration (Table 5).
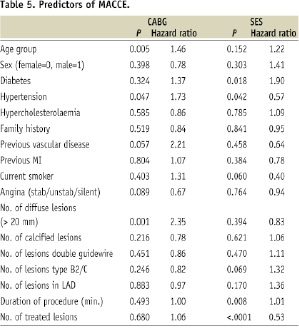
Age was not found to be an independent predictor of three-year outcomes amongst patients treated by PCI either with SES or BMS.
Discussion
The current investigation is the first to evaluate long-term outcomes of similar patients with MVD studied according to their age. Specifically, we assessed whether PCI with BMS, PCI with SES, or CABG is safer and/or more effective in particular age groups. In contrast to clinical registries, patients enrolled in the ARTS trials had less comorbidity, and a higher proportion of complete revascularisation.
At present the influence of age on long-term survival after PCI and CABG has not been adequately studied. Most of the data are derived from observational registries which doesn’t allow for a direct comparison between PCI and CABG, as elderly patients referred to one or the other revascularisation technique have different baseline characteristics. However a recent registry, which corrected for baseline differences, has shown a trend towards a better survival following surgery, despite the less invasive nature of PCI, and the lower initial morbidity.17,18
There is a limited amount of data available from randomised trials on the influence of age on patient outcome after revascularisation. The BARI and SoS trial showed that survival was better with CABG compared with PCI irrespective of age.19,20 Conversely, a systematic review has shown that long term survival after PCI or CABG is similar among patients over the age of 65 when compared to those younger than 65.21
Increasing age is associated with a lower three years survival among patients enrolled in CABG or SES arms of ARTS trials. However, neither PCI vs. CABG nor DES vs. BMS have a significant impact on survival up to three years, within each age quartiles.
This study has reiterated that important clinical and angiographic characteristics are age related. Older patients are more likely to be female, and when compared to their younger counterparts they are more likely to have comorbidities such as diabetes and hypertension.1-4 Furthermore, the elderly have more diffuse and complex coronary lesions on angiography.22,23 Therefore, in real-world clinical practice, when myocardial revascularisation is required, these important clinical characteristics are used on a case-by-case basis to make a clinical decision, without any well-established criteria for identifying those elderly patients more likely to benefit from PCI or CABG. Currently elderly patients with significant comorbidities tend to be treated by PCI, not only because it is less invasive, but also based on the results from the AWESOME randomised trial which demonstrated similar survival outcomes in patients >70 years of age following either PCI or CABG.24
The data from the ARTS-I trial confirms a gradual increase of both mortality (p=0.003) and morbidity (p=0.001) with age amongst patients referred for CABG. Although the death rate also increased with increasing age among ARTS-II patients (p=0.01), age (as assessed per quartile) was not an independent predictor of MACCE following PCI (p=0.15), whilst it did emerge as an important independent predictor of MACCE following surgery (p=0.005). The selection of patients without severe comorbidities, with preserved left ventricular function and amenable to (near) complete revascularisation by PCI is the most likely explanation of the excellent results observed after stenting, particularly amongst those treated with SES. Those patients having surgery also had similar baseline characteristics, and were low surgical risk based on their calculated EuroSCORE. Therefore this study demonstrates that the impact of age on the outcomes after coronary revascularisation for MVD is significantly more important after surgery than after PCI.
Our data show that the risk from surgery is highest during the in-hospital phase. Notably, the eldest patients (>68 years) undergoing surgery had a higher mortality rate than their counterparts treated by SES PCI. The in-hospital mortality observed in ARTS-I among surgically treated patients is in line with their predicted mortality based on the EuroSCORE. For patients included in the fourth quartile, the EuroSCORE predicted in-hospital mortality was of 3.58%, which is almost identical to that actually observed in this study (3.5%). For the younger age groups, the observed in-hospital mortality was slightly lower than that predicted by the EuroSCORE (0.0% vs. 1.27%, 0.6% vs. 1.33% and 1.3% vs. 2.07% for Q1, Q2 and Q3). These results are in keeping with recent evidence which suggests that the logistic EuroSCORE over estimates mortality, and requires recalibration.25 The SYNTAX trial has also shown that early outcomes after PCI are related to initial lesion characteristics, however new evidence also suggests that these early outcomes after PCI can be influenced by adverse patient characteristics as assessed by the EuroSCORE.26,27
Clearly, the late outcomes after PCI are determined by the need for repeat revascularisation. At three-year follow-up, 173, 39 and 89 repeat revascularisations with PCI and/or surgery were performed in the ARTS-I PCI, ARTS-I CABG and ARTS-II PCI patients, respectively. Consistent with other trials of DES the use of SES lead to a dramatic improvement in the results of PCI in MVD as compared to BMS PCI.28 This improvement has now been shown in our study to be independent of age. Despite the significantly lower repeat intervention rates with SES, CABG still remains associated with the lowest re-intervention rates in any age group quartile.
Previous studies have shown that diabetes is a strong predictor of adverse outcome among patients treated by PCI, most notably for those with MVD.29,30 Our results confirm that diabetes is the most important clinical risk factor for MACCE in patients treated by SES PCI. In the surgical group diabetes was not associated with MACCE, which is in contrast to previous observational studies which have shown diabetes to be an independent predictor of mortality.31-33 The relative safety and efficacy of CABG decreases with increasing age, and this is independent of a patient’s diabetic status. This data therefore suggests that young patients with diabetes benefit the most from surgery, and conversely, elderly patients without diabetes have a better outcome following SES PCI, compared to CABG.
This implies that in diabetic patients with MVD, amenable to both PCI and CABG, a patient’s age should be considered when deciding the most appropriate method of revascularisation. In view of the paucity of evidence this subject needs to be accurately assessed in a specifically designed clinical trial in diabetic patients. Currently there are no published randomised studies of revascularisation specifically in diabetics; previous data have all been derived from post hoc subgroup analysis. Recently the early results of the CARDia trial, the first dedicated randomised trial of revascularisation in diabetics, showed no difference in outcome between diabetic patients with MVD treated with PCI or CABG,34 although no age distributions have yet been released. The full publication of CARDia is awaited, together with the results of the on-going FREEDOM trial with the specific aim to clarify the role of CABG and PCI in diabetic patients with MVD. In the BARI 2D trial, Frye et al35 reported that for many patients with both diabetes and coronary artery disease, optimal medical therapy rather than any intervention is an excellent first-line strategy, notably for those with less severe disease. When revascularisation by PCI is indicated, five year MACE free survival is not affected by the initial treatment strategy (medical or revascularisation). However, when revascularisation by CABG is deemed the more appropriate revascularisation strategy, MACE free survival is better in patients initially randomised to surgery. This trial also indicates that treatment strategy must be individualised for specific patients, based on the most appropriate evidence-based treatment recommendations.
Study limitations
Firm conclusions regarding the advisability of SES PCI in the oldest patients with multivessel disease cannot be drawn from the comparative evaluation of the ARTS-I and ARTS-II trials. Moreover, these data refer to selected patients with low co-morbidities, who were amenable to complete revascularisation with either PCI or CABG; importantly very old patients (octogenarians) were excluded from this study.
This study combines results of a randomised trial (ARTS I) and a registry (ARTS-II). Population of the registry was comparable (in term of inclusion criteria) but “not matched” besides a similar 2/3 MVD ratio. We sought that age-corrected or propensity analysis would not be appropriate for the pooled ARTS-I and II population analysis. We therefore aimed to compare outcomes according to age quartile. However, using this approach, clinical and anatomical differences between patient’s arms of each quartile are not fully compensated.
An important limitation to consider is the long time lag between the enrolment of patients in ARTS-I and ARTS-II, which may have influenced outcomes. The development of new surgical techniques and increasing use of arterial conduits may of lead to improved surgical outcomes if the CABG patients had been enrolled at the same time as ARTS-II SES patients. Conversely the patients in ARTS-II had a worse baseline and procedural risk profile compared to those included in ARTS-I, however better stent design, improved PCI technique and equipment, as well as the increased use of anti-platelet agents probably account for the improved procedural success in these patients.
Clinical implications
Increasing age has an adverse prognosis in MVD patients treated by CABG which is not observed following percutaneous revascularisation. The use of SES has improved the results of PCI such that they are now as good as those of surgery for any age quartile, furthermore this use of SES is not associated with an excess in post discharge death or MI as compared to BMS. At present multivessel PCI with SES in elderly patients is a valuable alternative to surgery, particular in the absence of diabetes. Whether SES PCI is equivalent to CABG, or even superior in elderly patients without diabetes, needs to be formally demonstrated in a head to head randomised trial, with long-term follow-up to help define the optimal treatment of these patients.
Conclusions
Age seems to influence the CABG outcome in-hospital but not PCI. PCI-SES could offer lower immediate risk in patients with MVD and comparable long-term outcome as CABG especially in older patients. The worst outcome of PCI-BMS group is primarily related to the need for repeat revascularisation. Diabetes is the most important predictor of MACCE following PCI.

