Abstract
Aims: The aim of this study was to compare the 5-year outcomes of patients with multivessel disease (MVD) involving the proximal left anterior descending (LAD) artery who were treated with sirolimus drug-eluting stents (SES), bare metal stents (BMS) and coronary artery bypass surgery (CABG).
Methods and results: Clinical outcomes were compared between the 682 patients enrolled in the ARTS-I and ARTS-II study who had MVD involving the proximal LAD, and were treated with BMS (27.4%), CABG (30.2%), and SES (42.4%). At 5-year follow-up the primary endpoint of major adverse cardiovascular and cerebrovascular events (MACCE) occurred in 33.7%, 18.0% and 24.9% of patients treated with BMS, CABG and SES, respectively (BMS vs. SES p=0.04, CABG vs. SES p=0.07). Unadjusted and adjusted rates of mortality and death/stroke/myocardial infarction (safety) were comparable between all three treatments. Repeat revascularisation was significantly lower following CABG irrespective of adjustment. The absolute difference in MACCE between patients with a logistic EuroSCORE above and below the mean (i.e., 2.09%) was 18.8% (p=0.001), and 1.9% (p=0.28) for CABG and SES, respectively. In patients with a high EuroSCORE, SES was a significantly safer treatment (p=0.04) whilst repeat revascularisation remained lower with CABG irrespective of the EuroSCORE.
Conclusions: At 5-year follow-up CABG has comparable safety, and superior efficacy in terms of reducing repeat revascularisation compared to BMS and SES in the treatment of patients with MVD involving the proximal LAD however, appropriate patient selection remains imperative.
Introduction
The proximal segment of the left anterior descending (LAD) artery is the most important segment of the coronary tree after the left main stem (LMS). Its importance is highlighted by the poor prognosis if left untreated,1 and the recent appropriateness guidelines for revascularisation from the American Heart Association/American College of Cardiology (AHA/ACC), which do not deem revascularisation of the proximal LAD inappropriate, even if it is present in isolation, or associated with no symptoms in patients on little, or no therapy.2
The optimal method of revascularisation in patients with multivessel disease (MVD) (with or without involvement of the proximal LAD) continues to remain a contentious issue.3 Although patients with MVD have preferentially been treated with coronary artery bypass grafting (CABG), no survival advantage has ever been demonstrated in randomised trials comparing CABG to percutaneous coronary intervention (PCI) with either bare metal stents (BMS) or drug-eluting stents (DES).4-6 Moreover, recent evidence suggests that PCI with DES offer a safe and suitable alternative to CABG in specific groups of patients with MVD.6-7
In patients with MVD with proximal LAD involvement previous observational studies have demonstrated a prognostic advantage following revascularisation with CABG compared to balloon angioplasty, or PCI with BMS.8-10 This benefit however, has not been reproduced in the sub-group analyses of patients with proximal LAD lesions enrolled in randomised studies of MVD comparing BMS to CABG.11,12 Moreover, in this group of patients the data on the use of DES, which offer the advantage of reduced rates of restenosis compared to BMS,13 is limited by the availability of only medium term outcomes.14-16
The Arterial Revascularisation Therapies Part I (ARTS-I) and Part II (ARTS-II) studies both recruited patients with MVD using the same inclusion criteria.17-18 In the ARTS-I study patients were randomised to treatment with a BMS or CABG, whilst in the single arm ARTS-II study all patients received a sirolimus eluting stent (SES). The 3-year outcomes of 682 patients with proximal LAD disease from the ARTS-I and ARTS-II study have been published previously.14 The aim of this report was to describe the 5-year outcomes (i.e., major adverse cardiovascular and cerebrovascular events – [MACCE]) of this important pre-specified sub-group of patients, which consequently represents the longest reported follow-up of proximal LAD disease treated with DES.
Methods
Study population
The ARTS-I and ARTS-II studies have been published previously.17,18 In brief, the multicentre ARTS-I study randomised 1,205 patients between April 1997 and June 1998 to treatment with PCI with a BMS or CABG. The ARTS-II study was a multicentre, non-randomised, open label trial which recruited 607 patients between February and November 2003 who were all treated with PCI using a SES.
Patient selection
The inclusion and exclusion criteria for both studies were the same. Patients with stable angina, unstable angina or silent ischaemia, who had ≥2 coronary lesions, located in different major epicardial vessels and/or their side-branches (not including the LMS) that were potentially amenable to stent implantation were eligible for inclusion. All patients were required to have a lesion with a diameter stenosis >50% in the LAD, and ≥1 other major epicardial coronary artery.
The goal was to achieve complete anatomic revascularisation. There was no restriction on the total implanted stent length. Decisions to place stents in lesions with bifurcations, fresh thrombus, calcification, diffuse disease, complex anatomy or stenting of side branches were left to the discretion of the operators. By protocol surgical revascularisation was performed “on-pump”, and where possible the left internal mammary artery graft was used for LAD revascularisation.
The major exclusion criteria were: patients with previous PCI, LMS disease, overt congestive heart failure, left ventricular ejection fraction <30 percent, history of a cerebrovascular accident (CVA), transmural myocardial infarction (MI) in the preceding week, severe hepatic or renal disease, neutropenia or thrombocytopenia, an intolerance or contraindication to acetylsalicylic acid or thienopyridines, the need for concomitant major surgery and life-limiting major concomitant non-cardiac diseases. Written informed consent was obtained from each patient prior to enrolment, and the study was approved by the ethics committee of each participating site.
The five year outcomes of the ARTS-I and ARTS-II patient cohorts have already been published elsewhere.19,20 This pre-specified sub-group analysis included only those patients with a >50% diameter stenosis lesion in the proximal LAD, defined as the coronary segment between the branching point of the LMS and the first major septal branch (segment 6 in the AHA classification).21
Endpoints
The primary endpoint of this study was MACCE, defined as a composite of death, stroke, MI and repeat revascularisation (percutaneous or surgical) at 5-year follow-up. Secondary endpoints included death, stroke, MI, safety (a composite of death, stroke and MI) and repeat revascularisation at 5-year follow-up.
Definitions
Deaths included mortality from any cause. Cerebrovascular accidents included transient ischaemic attacks, reversible neurological deficits, intracranial haemorrhage, and ischaemic stroke.17 MI was defined in the first seven days after the intervention, if there was documentation of new abnormal Q-waves and either a ratio of serum creatinine kinase MB (CK-MB) isoenzyme to total creatinine kinase (CK) that was ≥0.1, or a CK-MB value that was five times the upper limit of normal. Serum CK and CK-MB isoenzyme concentrations were measured 6, 12, and 18 hours after the intervention. Commencing eight days after the intervention (the length of the hospital stay after surgery), either abnormal Q-waves or enzymatic changes were sufficient for a diagnosis of MI. An MI was only confirmed after the relevant electrocardiograms had been analysed by the core laboratory and adjudicated by the clinical-events committee. This two-part method of defining MI was developed for ARTS-I to address the difficulty in diagnosing an MI after cardiac surgery.17 The incidence of stent thrombosis according to the Academic Research Consortium definitions was only available for patients in ARTS-II.22
Statistical methods
Continuous variables are expressed as mean±standard deviation (SD) and were compared using the unpaired Student’s t-test. Categorical data are presented as percentages, and were compared using the χ2 test or Fischer’s exact test. Survival curves were constructed for time-to-event variables using Kaplan-Meier estimates, and compared by the log-rank test. Patients lost to follow-up were considered at risk until the date of last contact, at which point they were censored. The overall association between treatment type and MACCE was further examined using univariate and multivariate Cox proportional hazard models. In the multivariate model, to compensate for difference in baseline and procedural characteristics between patients enrolled in ARTS-I and ARTS-II adjustments were made for the potential confounders of gender, logistic EuroSCORE (EUROLOG), smoking status, diabetes, hypercholesterolaemia, hypertension, and previous myocardial infarction. Finally patient outcomes were also stratified into two groups according to the mean value of the EUROLOG. A p value of <0.05 was considered significant, and all tests were two-tailed. Data were analysed with SPSS version 17.0 software (SPSS Inc., Chicago, IL, USA).
Results
The ARTS-I study recruited 1,205 patients, of whom a total of 393 (32.6%) had involvement of the proximal LAD. The ARTS-II study enrolled 607 patients, of whom 289 (47.6%) had proximal LAD disease. In total there were 682 patients in this sub-group analysis of whom 187 (27.4%), 206 (30.2%), and 289 (42.4%) received treatment with BMS, CABG and SES, respectively.
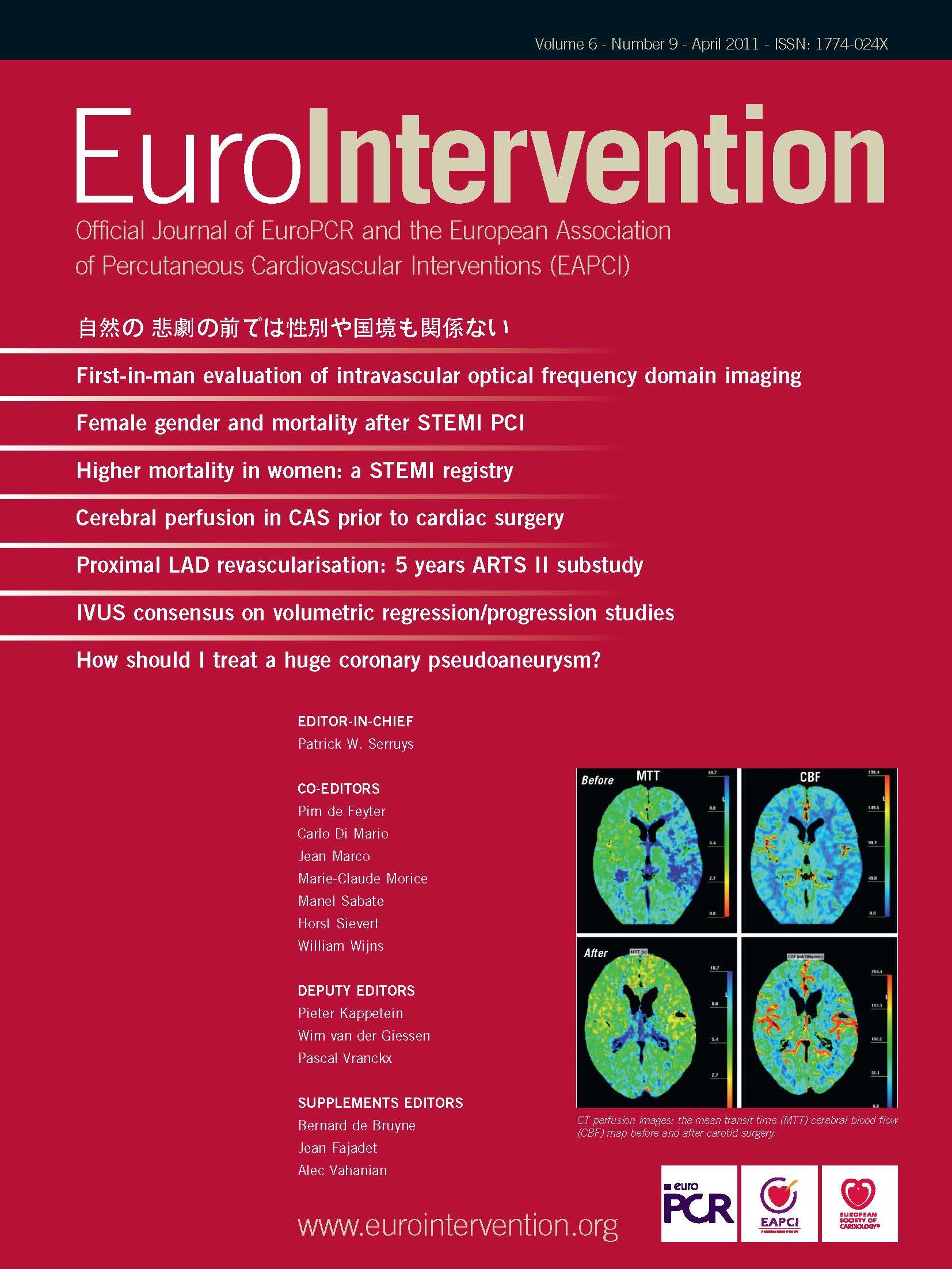
Baseline angiographic characteristics (Table 1)
Baseline angiographic characteristics of the study population, stratified according to method of revascularisation, have been published previously, and are summarised in Table 1.11,14 As expected considering the time lag between the two studies the incidence of risk factors was significantly higher in the cohort treated with SES. Despite this however, the overall risk as assessed using the EuroSCORE (additive or logistic) was similar for each treatment group.
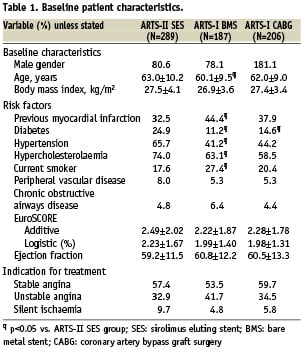
Angiographic and lesion characteristics (Table 2)
The characteristics of the proximal LAD lesions are shown in Table 2. Patients treated with SES had significantly more complex lesions as indicated by the longer lesion length, and greater proportion of Type C lesions, calcified lesions and bifurcations when compared with those treated with BMS or CABG. The characteristics of coronary lesions in segments other than in the proximal LAD are presented elsewhere.14 Overall patients treated with SES had more extensive disease, and significantly lower rates of complete revascularisation compared to those treated with BMS or CABG. Patients receiving CABG had the longest hospital stay.
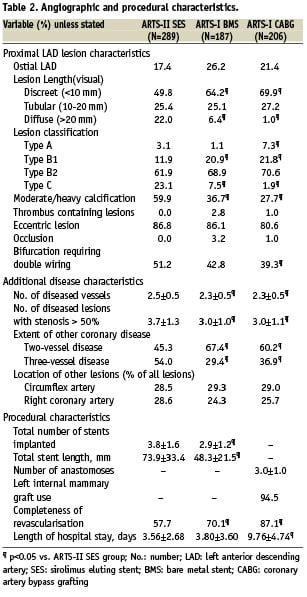
Outcomes at 5-years (Table 3, Figure 1)
The hierarchical and non-hierarchical outcomes at 5-years follow-up are shown in Table 3, whilst unadjusted Kaplan Meier survival curves are shown in Figure 1. Overall there was a significant reduction in the primary endpoint of 5-year MACCE following treatment with SES compared to BMS (Relative risk [RR] 1.35, 95% CI [1.02-1.80], p=0.04), whilst only a trend towards a lower incidence of MACCE was seen amongst those treated with CABG compared to SES (RR 0.72, 95% CI [0.51-1.03], p=0.07). In general, safety was comparable between all three treatments modalities.
The 5-year outcomes between patients treated with CABG and SES stratified according to a EUROLOG above or below the mean of 2.09% is shown in Figure 2. The absolute difference in MACCE for patients treated with CABG, and SES between those with low and high EUROLOG was 18.8% (p=0.001), and 1.9% (p=0.28), respectively, which was primarily driven by the increased incidence of death/CVA/MI in those patients with high EUROLOG. Repeat revascularisation remained lower with CABG irrespective of EUROLOG; in addition, within each treatment group there was no significant difference in rates of repeat revascularisation between patients with high or low EUROLOG.
Figure 3 shows the univariate and multivariate Cox proportional hazard models for outcomes between SES and CABG at 5-year follow-up. After adjusting for confounding factors, rates of mortality, the composite of safety, and the composite of MACCE remained comparable between SES and CABG. Of note, even after adjustment CABG remained the most effective treatment in terms of reducing repeat revascularisations.
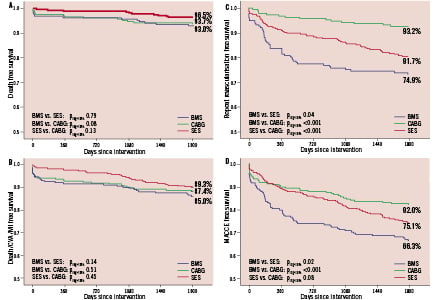
Figure 1. Kaplan Meier survival curves at 5-year follow-up for (A) death (B) death/stroke/myocardial infarction (C) any repeat revascularisation and (D) major adverse cardiovascular and cerebrovascular events (MACCE) for treatment with sirolimus eluting stents (SES), bare metal stents (BMS) and coronary artery bypass surgery (CABG).
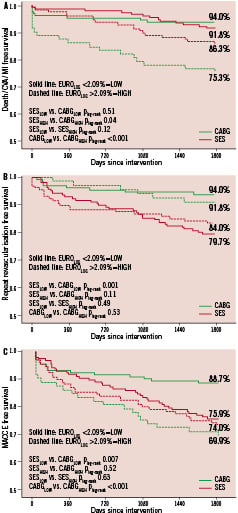
Figure 2. Kaplan Meier survival curves at 5-year follow-up up for (A) death/stroke/myocardial infarction (B) any repeat revascularisation and (C) major adverse cardiovascular and cerebrovascular events (MACCE) for treatment with sirolimus eluting stents (SES), and coronary artery bypass surgery (CABG) stratified according to patients with a logistic EuroSCORE above (dotted line) or below (solid line) 2.09%.
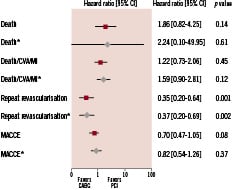
Figure 3. Unadjusted ( ) and adjusted (
) and adjusted ( ) Hazard ratios at 5-years follow-up between treatment with sirolimus eluting stents (SES) and coronary artery bypass surgery (CABG). Hazard ratios were adjusted for gender, logistic EuroSCORE, smoking status, diabetes, hypercholesterolaemia, hypertension, and previous myocardial infarction. *Adjusted for, gender, logistic EuroSCORE, smoking status, diabetes, hypercholesterolaemia, hypertension, and previous myocardial infarction.
) Hazard ratios at 5-years follow-up between treatment with sirolimus eluting stents (SES) and coronary artery bypass surgery (CABG). Hazard ratios were adjusted for gender, logistic EuroSCORE, smoking status, diabetes, hypercholesterolaemia, hypertension, and previous myocardial infarction. *Adjusted for, gender, logistic EuroSCORE, smoking status, diabetes, hypercholesterolaemia, hypertension, and previous myocardial infarction.
Stent thrombosis
Definite stent thrombosis according to ARC definitions occurred in 2.8% of the ARTS-II proximal LAD patients (early 0.7%; late 0.3%; very late 1.7%), while the composite of definite or probable stent thrombosis occurred in 6.6% (early 1.4%; late 0.7%; very late 4.5%).
Discussion
The main findings from this study are that in patients with MVD involving the proximal LAD, overall long-term safety outcomes are comparable following treatment with SES, BMS, or CABG. Moreover, this study also demonstrates that in this complex group of patients CABG remains the most effective treatment in terms of reducing repeat revascularisation out to 5-year follow-up.
The proximal LAD occupies an important location in the coronary arterial tree, and as such it is no surprise that untreated lesions in this location are associated with poor outcomes.1 Its importance is further reflected by recommendations that revascularisation of any significant proximal LAD lesions, even in the absence of symptoms, is not deemed inappropriate.2
Proximal LAD disease can occur in isolation or in association with MVD. The former has been the subject of numerous randomised controlled trials, which have compared PCI using BMS, to surgical revascularisation by standard CABG or minimally invasive direct CABG with a LIMA-to-LAD anatomosis.23-25 Meta-analysis of these studies report similar survival between groups out to 5-year follow-up, and reduced repeat revascularisation with CABG.
In the setting of MVD, data is confined to retrospective studies, and long-term outcome (>3 years) data is limited.9-12,14-16 In general there is little dispute over the superiority of DES over BMS in terms of reducing rates of target lesion revascularisation (TLR).13 For lesions in the proximal LAD however, the issue is complicated by the proximal LAD having a normal mean minimum lumen diameter of approximately 3 mm,26 the cut off above which DES have been shown to offer only limited clinical benefit.27 Consistent with this, Bonello et al recently reported no significant difference in MACE or TLR at 1-year follow-up among 487 patients with MVD and non-ostial proximal LAD lesions, treated with BMS or DES (mean stent diameter 3.2 mm).15 In contrast to these results, the current study demonstrates not only comparable safety, but also a significant reduction in repeat revascularisation (p[log-rank]=0.04) and overall MACCE (p[log-rank]=0.02) out to 5-years with the use of DES compared to BMS.
In this the sub-group of patients with MVD and proximal LAD lesions, treatment with CABG has shown a consistent benefit in terms of reduced repeat revascularisation compared to balloon angioplasty, and PCI with either BMS or DES.9-12,14,16,28 With respect to safety, there have been conflicting results. The majority of the data comes from sub-group analyses of the New York State registry, and results demonstrate a consistent and significant improvement in adjusted survival out to 3-years follow-up after treatment with CABG compared to balloon angioplasty or stenting with BMS.9,10 In contrast however, comparable safety was seen in this group of patients in the sub-group analysis of the randomised ARTS-I study.11
Similar inconsistent results have also been seen in the more recent observational studies which have included patients treated with DES. Yan et al recently reported comparable adjusted mortality at 2-year follow-up between DES and CABG,16 whilst Hannan et al demonstrated no difference in unadjusted survival between groups, however following adjustment, outcomes were superior following CABG.28 In addition, Kukreja et al reported the 3-year outcomes from the current cohort and showed significantly improved unadjusted survival following SES implantation. This benefit has not been maintained out to 5-years, and is likely to reflect the larger absolute increase in death (SES ∆2.4%, CABG ∆1.0%) and MI (SES ∆2.8%, CABG ∆1.0%) between 3- and 5-years follow-up observed in patients treated with SES compared to CABG. It is more than likely that these events were driven by definite/probable stent thrombosis which rose by 73% in this cohort between 3- and 5-year follow-up.
One of the limitations of these previous observational studies is the difficulty in effectively adjusting outcomes according to different baseline clinical and angiographic variables.29 In daily practice, this heterogeneity reiterates the importance of appropriate patient selection when deciding individualised revascularisation strategy in patients with MVD.6,7 Historically CABG has been the preferred method of revascularisation in these patients; however it is now apparent that in select patients, PCI is a safe and effective alternative.6 In the current study the EUROLOG identified those patients who were at highest risk of adverse events following treatment with either CABG or PCI. Most importantly, in those patients with a high EUROLOG, PCI offered a significantly safer treatment, and an improved MACCE free survival compared to CABG. This is in keeping with previous published data which have indicated that the EuroSCORE has a role to play in risk stratification amongst patients undergoing revascularisation by either PCI or CABG.30,31
In contrast to this patient based risk assessment, assessment of coronary anatomy, using for example, the SYNTAX score, is also of vital importance.32 Studies indicate that the SYNTAX score can help aid revascularisation decisions; however it also has an increasingly important role in patient risk stratification.6,7,33,34 Importantly the calculation of the SYNTAX score requires a careful and through review of the coronary angiogram. This may identify those patients in whom completely revascularisation with PCI cannot be achieved, which can have significant implications on overall outcome.35 In the current cohort complete revascularisation was accomplished in only 57.7% of patients in the SES group, compared to 87.1% (p<0.05) of those treated with CABG. In additional incomplete revascularisation was a univariate predictor of MACCE in patients treated with SES (HR:1.65, 95% CI:1.02-2.66, p=0.04). These results reiterate the importance of a comprehensive risk assessment to ensure that patients receive the most appropriate tailored revascularisation strategy, which takes into consideration their comorbidities and coronary anatomy.36,37
Limitations
The current study is limited by the long time lag between the enrolment of patients in ARTS-I and ARTS-II, which may have influenced outcomes. The development of new surgical techniques and increasing use of arterial conduits may of lead to improved surgical outcomes if the CABG patients had been enrolled at the same time as ARTS-II patients. Conversely the patients in ARTS-II had a worse baseline and procedural risk profile compared to those included in ARTS-I, however better stent design, improved PCI technique and equipment, as well as the advances in pharmacological therapy probably account for the overall improved outcomes. In addition ARTS-II was a registry, and as such suffers from the inherent limitation of this type of study. Moreover, this cohort represents a sub-group analysis and therefore endpoints were not adequately powered to provide definitive results. Leaving these study design limitations aside, the absence of SYNTAX scores in patients treated with CABG is a limitation which otherwise would have allowed a more effective comparison of anatomical complexity. Unfortunately the angiographic films for ARTS-I are unavailable.
Conclusion
At 5-years follow-up surgical revascularisation remains the most effective treatment in terms of reducing repeat revascularisation in patients with MVD involving the proximal LAD. Safety at 5-year follow-up is comparable overall; however in those patients with a high EUROLOG, SES appears to provide a safer alternative to CABG. These results reiterate that appropriate patient selection, taking into account both anatomical and clinical variables is imperative when determining the optimal revascularisation strategy in these complex patients.