Abstract
Aims: As the global population ages, elderly patients will form an increasing proportion of those undergoing percutaneous coronary intervention (PCI). We investigated the safety and efficacy of bare metal stents (BMS) and DES in all patients undergoing PCI at our institution, stratified by age.
Methods and results: We investigated three sequential groups of consecutive patients treated exclusively with BMS (n=2,194; January 2000 to April 2002), sirolimus-eluting stents (SES, n=834; April 2002 to February 2003) and paclitaxel-eluting stents (PES, n=2,841; February 2003 to December 2005). The primary endpoint was all-cause mortality. Secondary endpoints included target vessel revascularisation (TVR) and composite major adverse cardiac events (MACE, defined as all-cause death, any nonfatal myocardial infarction or TVR). Patients were followed up for a median of 1,366 days. Patients were stratified into equal quintiles based on age (<51.8, 51.8-58.4, 58.4-65.4, 65.4-73.0 and >73.0 years). All-cause mortality was significantly higher in the eldest two groups, while TVR rates were similar across all age groups. DES were associated with reductions in TVR and MACE and a trend towards reduced mortality in all age groups.
Conclusions: DES are safe and effective when compared to BMS, irrespective of age.
Introduction
The benefit of percutaneous coronary intervention (PCI) with bare metal stents (BMS) in elderly patients is clearly established, with improvements in quality of life and clinical outcome when compared to medical therapy1-8. However, although global life expectancy is rising (projected increase from 77 years to 82 years by 2045-2050 in developed countries)9 and drug-eluting stents (DES) have been shown to be effective in reducing restenosis in a wide array of patients10-12, the relative safety and efficacy of DES in the elderly remains less clearly established, with existing data limited to either small cohorts or relatively short-term follow-up13,14. The majority of randomised controlled trials of drug-eluting stents had an mean age of 60-65 years12, and therefore, provide little information for the ever-growing elderly population. As a result, recently the American Heart Association has called for an increase in the recruitment of elderly patients in clinical trials15,16. We therefore stratified all patients undergoing PCI in our institution between 2000-2005 for de novo coronary stenoses by age, to investigate the long-term safety and efficacy of contemporary PCI with BMS and DES in different age groups.
Methods
Between January 2000 and December 2005, we examined all patients undergoing PCI with a single stent type for de novo coronary stenoses in our institution. The only exclusion criteria were the implantation of more than one different stent type during the index procedure or PCI for in-stent restenosis (Figure 1). Initially, all patients were treated with BMS, but on the 16th April 2002, our institution adopted the use of sirolimus-eluting stents (SES: Cypher; Cordis, Warren, NJ, USA) as the default strategy for all coronary interventions as part of the RESEARCH registry17. On the 16th of February 2003, SES were replaced by paclitaxel-eluting stents (PES: TAXUS; Boston Scientific, Natick, MA, USA) as the default stent as part of the T-SEARCH registry18. This single centre registry therefore consists of three sequential groups of consecutive patients: BMS (n=2,194; January 2000 to April 2002), SES (n=834; April 2000 to February 2003) and PES (n=2,841; February 2003 to December 2005). Patients initially enrolled in one of the sequential cohorts (BMS, SES or PES) were maintained for analytical purposes throughout the follow-up period in their original cohort, even if a subsequent intervention of another lesion was performed using a different type of stent. We subsequently stratified the patients into quintiles based on age. The primary endpoint was all-cause mortality. Secondary endpoints included target vessel revascularisation (TVR) and composite major adverse cardiac events (MACE, defined as all-cause death, nonfatal myocardial infarction in any vascular territory or TVR).
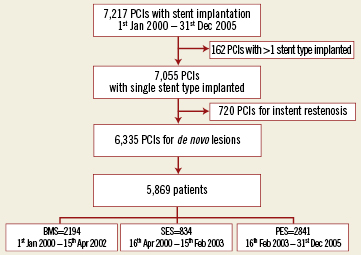
Figure 1. Flowchart of patient recruitment.
All procedures were performed following standard procedural guidelines at the time19. The use of glycoprotein IIb/IIIa inhibitors or adjunctive devices was left up to the operator’s discretion. Angiographic success was defined as residual stenosis <30% by visual estimation in the presence of Thrombolysis in Myocardial Infarction (TIMI) grade 3 flow. All patients were advised to maintain lifelong aspirin. Hypercholesterolaemia was defined as fasting total cholesterol >5mmol/l (193 mg/dl) or the use of lipid-lowering therapy. Hypertension was defined as blood pressure greater than 140/90 mmHg or the use of antihypertensive medications. Renal impairment was defined as a serum creatinine >150 µmol/l (1.7 mg/dl).
Annual follow-up survival data were obtained from municipal civil registries for all patients. The causes of death were classified according to the International Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). A questionnaire was subsequently sent to all living patients with specific enquiries about repeat hospital admission and adverse events. As the principal regional cardiac referral centre, repeat procedures (percutaneous and surgical) are normally performed at our institution and recorded prospectively in our database. For patients who suffered an adverse event at another centre, medical records or discharge summaries from the other institutions were systematically reviewed. General practitioners, referring cardiologists and patients were contacted as necessary if further information was required. The protocol was approved by the hospital ethics committee and is in accordance with the Declaration of Helsinki. Written informed consent was obtained from every patient.
Statistical analysis
The patient population was stratified into five groups using the 20th, 40th, 60th and 80th age percentiles as cut-off points. Categorical variables are presented as percentages and were compared by Pearson’s chi-square test or Fisher’s exact test. Continuous variables are presented as mean ±standard deviation and were compared by means of the F test for analysis of variance. A 2-sided p value of <0.05 was used to indicate statistical significance. The cumulative incidence of adverse events was estimated according to the Kaplan-Meier method and curves were compared using the log-rank test. Patients lost to follow-up were considered at risk until the date of last contact, at which point they were censored. To adjust for differences in baseline characteristics between the age groups, each paired age group comparison was forced into separate Cox regression models, using all variables listed in Table 1. To investigate the effects of stent type on outcomes, stent type was forced into separate Cox regression models for each age group, again using all variables in Table 1. The final results are presented as adjusted hazard ratios (HR) with 95% confidence intervals (CI).
Results
Complete follow-up was available for 98.6% of patients, with a median duration of follow-up of 1,366 days (interquartile range [IQR]: 962-1,797). The mean age of the total cohort was 61.9±11.6 years. The values for the 20th, 40th, 60th and 80th age percentiles were 51.8, 58.4, 65.4 and 73.0 years, respectively. The patient population was subsequently stratified into five age groups using these cut-off values. There were significant differences in the duration of follow-up between the groups, with a shorter duration for the older groups: Group 1 median follow-up 1,463 days (IQR: 966-2,010), Group 2 median 1,481 days (IQR: 922-2009), Group 3 median 1,379 days (IQR: 887-1,768), Group 4 median 1,332 days (IQR: 833-1,766) and Group 5 median 1,212 days (IQR: 750-1,652).
There were significant differences in risk factor profiles across the groups (Table 1): as the patients became progressively older, there were more women and higher rates of hypertension, diabetes mellitus, renal impairment and the patients more often had undergone previous revascularisation. The eldest groups had lower rates of hypercholesterolaemia and a family history of coronary disease, and were less often current smokers. The older groups were more likely to present with unstable angina or non-ST-elevation-MI, while the younger groups were more likely to present with ST-elevation MI.
Angiographic and procedural variables are also described in Table 1. The older cohorts had more extensive coronary disease and underwent more extensive revascularisation: they were more likely to have treatment of the left main coronary artery or a saphenous vein graft and to undergo multivessel PCI. Glycoprotein IIb/IIIa inhibitors were used less frequently as age increased.
The mortality rates were significantly higher in the eldest two groups (Figure 2A) although there were no differences in TVR rates (Figure 2B). The cumulative rates of composite MACE were also higher in the oldest two cohorts (Figure 2C). Table 2 shows the adjusted hazard ratios for all-cause mortality, TVR and composite MACE between the different age groups. The eldest two cohorts had a trend towards higher TVR rates when compared to the younger three groups (statistically significant when compared to group 2). Mortality rates were higher in the older groups (although not reaching statistical significance when comparing group 1 with group 2, and group 2 with group 3). Although MACE rates also increased in the older groups, the relative excess in risk for MACE compared with younger patients was lower than the risk for death.
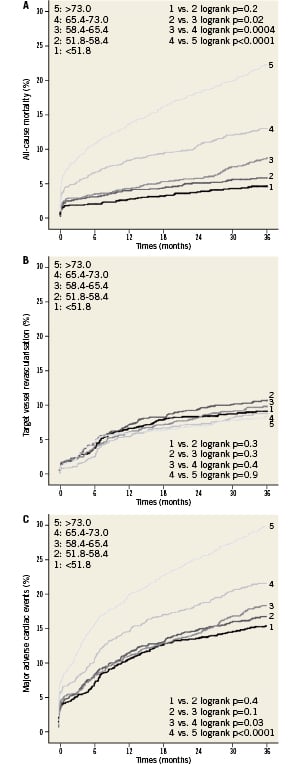
Figure 2. Kaplan-Meier curves for the cumulative incidence of (A) all-cause mortality (B) target vessel revascularisation and (C) composite major adverse cardiac events (all-cause death, nonfatal myocardial infarction or target vessel revascularisation) amongst patients stratified by age.
When examining clinical endpoints according to stent type, DES were associated with consistent non-significant trends towards lower all-cause mortality in all age groups (Figure 3A). There were no differences in the rates of cardiac death comparing DES with BMS across all five age groups (Figure 3B).TVR was significantly lower with DES in all apart from the oldest group, where the benefit just failed to reach statistical significance (Figure 3C). Overall MACE was lower in all age groups, although not reaching statistical significance in the youngest and oldest (Figure 3D).
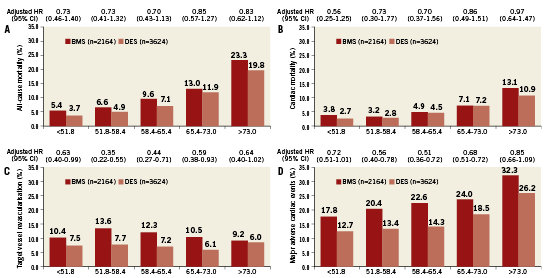
Figure 3. Rates of adverse events in patients according to stent type with hazard ratios for treatment with drug-eluting vs. bare metal stents after adjustment for differences in baseline characteristics: (A) all-cause mortality (B) cardiac mortality (C) target vessel revascularisation and (D) composite major adverse cardiac events (all-cause death, nonfatal myocardial infarction or target vessel revascularisation). BMS: bare metal stents; DES: drug-eluting stents; HR: hazard ratio; CI: confidence interval
Discussion
The main findings of this study are that DES are safe and effective irrespective of age: they reduce TVR and overall MACE and are associated with non-significant reductions in mortality compared to BMS across all age groups. Although TVR rates were similar between the age groups, MACE and mortality rates increased with age: the oldest group had a five-fold increase in mortality compared with the youngest group within three years of the procedure (adjusted HR 5.15, 95% CI 3.55-7.49).
A recent analysis of Medicare patients in the USA aged 66 or older found a significant reduction in 2-year mortality with DES when compared to contemporary BMS patients (adjusted HR 0.83, 95% CI 0.81-0.86) and historical BMS patients (adjusted HR 0.79, 95% 0.77-0.81)20. We found a similar risk reduction amongst our patients groups, although the smaller sample size of our population meant the reduction in mortality across all age groups did not reach statistical significance.
The United Nations department of Economic and Social affairs has estimated that the global life expectancy at birth has risen from 58 years in 1970-1975 to 67 years in 2005-2010, and is expected to keep on rising to reach 75 years in 2045-2050. In developed countries, the projected rise is from 77 years today to 82 years by the middle of the 21st century, and in the less developed regions, from 65 years in 2005-2010 to 74 years in 2045-2050. In The Netherlands, the current overall life expectancy is 79.8 years (77.5 years for male and 81.9 years for females) which is the 17th highest life expectancy in the world (below Japan but above the USA)9. Given this data, and the fact that in our population the age of 80 represented the 95th centile, rather than using an arbitrary cut-off point, we have employed a more recognised statistical methodology by stratifying our patients by age into equal groups by quintiles. The patients in our oldest group (age >73.0 years) had a mean age of 78 years, and therefore represent the very elderly. These patients had significantly higher all-cause mortality than the patients in Group 4 (age 65.4-73.0 [adjusted HR 1.83, 95% CI 1.43-2.34]).
It is already well established that the elderly have more extensive coronary disease and more comorbidities than younger patients. Furthermore, they have greater degrees of coronary artery calcification and a higher risk of bleeding, particularly if glycoprotein IIb/IIIa inhibitors are used21,22. Nevertheless, there is evidence that PCI with BMS may improve quality of life1,2,7 and survival3,23 in elderly patients, even though their short- and long-term survival remains poor compared to younger patients24-28. It is reasonable to assume that provided that DES are safe and effective in reducing restenosis in the elderly, the quality of life benefits may even supersede those provided by BMS. Nevertheless, existing data on revascularisation in elderly patients (irrespective of the definition or cut-off point used) in the DES era are limited either by small numbers or short-term follow-up13,29. The randomised trials comparing DES and BMS provide little data on elderly patients22. Data from the German Cypher registry found that in 954 patients aged over 75 years, the 6-month unadjusted mortality (3.6%) was three times that of patients under 75, with no difference in TVR (7.3%) or MACE (14.6%)14. Our data are therefore unique, since we found a decrease in TVR and overall MACE with DES in all age groups after a median of 1,366 days, despite more advanced coronary disease and more extensive revascularisation in our elderly patients. The similar rates of reduction in TVR across all age groups show that DES are effective, regardless of age. Although the mortality in the eldest group was markedly higher than in younger patients, we found a non-significant trend towards reduced mortality with DES compared to BMS with no increase in cardiac deaths across the board, providing reassuring evidence regarding the safety of DES in elderly patients.
Limitations
This is a single centre observational study. Furthermore, there were significant baseline and procedural differences between the three historical stent groups, together with different lengths of follow-up due to their sequential nature. We have attempted to account for differences between the cohorts in terms of baseline demographics by using Cox regression analysis, although we acknowledge that each statistical method has limitations and there is no consensus method for adjusting for these differences. Nevertheless, the use of a single stent type at any particular time period eliminates bias towards using DES in higher risk patients. Furthermore, very elderly patients (age >90) were not investigated separately in this analysis: further research on this subset of patients is required.
Acknowledgements
We would like to acknowledge the senior cardiologists involved in the PCI procedures: P.J. de Feyter, MD, PhD; P.P.T. de Jaegere, MD, PhD; H.J. Duckers MD,PhD; S.H. Hofma, MD, PhD; E. McFadden, MD, PhD; E.Regar, MD, PhD; G. Sianos, MD, PhD; P.C. Smits, MD, PhD; M.J. van der Ent, MD, PhD; W.J. van der Giessen, MD, PhD; C.A. van Mieghem, MD.
Conflict of interest statement
The authors have no conflicts of interest to declare.

