Abstract
To illustrate the interplay between coronary surgery and percutaneous interventions in secondary revascularisation, we report on the case of a patient with a long-standing history of ischaemic coronary disease, who underwent multiple percutaneous coronary interventions (PCI) and two coronary artery bypass grafting (CABG) procedures. The course of action selected for treatment was based on the anatomical features of the coronary lesions and the patient’s clinical situation.
Description of case
We present the case of a 76-year old man with a history of smoking and surgery for a tongue tumour. In August 2005, he suffered a non-ST segment elevation myocardial infarction (NSTEMI) that was treated by percutaneous coronary intervention (PCI) of the right coronary artery (RCA) with the implant of a 4x15 mm Driver stent (Medtronic Inc., Minneapolis, MN, USA). In the angiogram, a 40% lesion in the left anterior descending artery (LAD) was observed.
In February 2008, the patient presented with angina that progressed to pain at rest (Braunwald Class IIB). Coronary angiography revealed a 40% lesion in the left main coronary artery (LMCA), a 40% lesion in the RCA and a 90% lesion in the LAD (Figure 1 and video 1). The therapeutic option decided upon was a left internal mammary artery (LIMA) bypass graft to the LAD. The intervention was performed without any incidences. Within two hours of arriving at the ICU, an ECG indicated ST-segment elevation in V1-V4 and anterior hypokinesia. Urgent coronary angiography revealed an obstruction in the LIMA-LAD graft (Figure 2 and video 2). Percutaneous revascularisation with two stents (Vision 2.75x16 mm; Abbott Vascular, Diegem, Belgium) in the middle and proximal LAD segments was performed with a good final outcome (Figure 3 and video 3). Seven days later the patient was discharged in a good clinical situation.

Figure 1. Coronary angiogram showing a 90% LAD lesion.

Figure 2. Coronary angiogram showing occlusion of the LIMA-LAD graft.

Figure 3. Angiogram showing the outcome of PCI of the proximal and middle LAD.
Four months later, in June 2008, the patient presented with CCS Class II exertional angina, and an angiogram revealed a 40% lesion in the LMCA and RCA and a new 70% lesion in the proximal portion of the stent implanted in the proximal LAD that affected the origin of the circumflex coronary artery (Figure 4).

Figure 4. Coronary angiogram showing a 70% proximal LAD intrastent restenosis affecting the origin of the circumflex coronary artery.
After discussing this case in a surgical-medical session, repeat surgery with a right mammary artery bypass graft to the LAD and an inverted saphenous vein graft to the circumflex artery was decided upon. Next, using the stabiliser Cor-Vasc System™(Coroneo QC, Montreal, Canada) for off-pump coronary artery bypass (OPCAB) surgery, the RIMA was anastomosed to the LAD and the saphenous vein to the circumflex artery in a heart-beating procedure. Finally, the saphenous vein was anastomosed to the aorta and graft patency was checked using the transit time flow meter Medi-Stim ASA™(Oslo, Norway) (Figures 5 and 6). The patient was sent home seven days later. Six months later he remains free of symptoms.
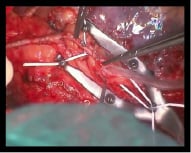
Figure 5. Anastomosing the RIMA to the LAD using the Coroneo system.
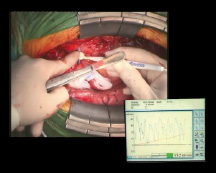
Figure 6. Measuring flow through the RIMA-LAD graft.
Discussion and conclusion
The present case illustrates the need for multiple percutaneous or surgical revascularisation procedures seldom found in cardiovascular patients. The choice of treatment should take into account the anatomical features and the patient’s clinical situation. In this case, surgery was pursued as initial therapy because of the lesion characteristics: the proximal LAD was affected and PCI was challenged by the involvement of the circumflex artery ostium. Unfortunately, the LIMA grafted to the LAD became occluded in the immediate postoperative period. This led to the deterioration of ventricular function and haemodynamic instability which required urgent coronary angiography and PCI to resolve the problem. Four months later, the patient suffered in-stent restenosis in the proximal LAD with involvement of the origin of the circumflex artery. At this point, ventricular function had improved. Thus, the decision of performing surgical secondary revascularisation was made when the risk of affecting the circumflex artery during re-stenting at a proximal LAD location was taken into account. Repeat CABG could then be performed out of a compromised haemodynamic situation, since left ventricular function had recovered after rescue PCI for the first intervention.
Our group performs systematically off-pump coronary surgery even in patients requiring re-interventions for coronary disease. We feel OPCAB is a very useful option for coronary re-operations. Several studies1,2 have documented that this strategy is superior to pump bypass surgery in terms of reducing complication rates (transfusion, atrial fibrillation, myocardial enzyme release) and, consequently, shortened hospital stay.
Of the many coronary stabilisation systems, we use the Cor-Vasc System™(Coroneo QC, Montreal, Canada) on the grounds of its excellent safety and proven results3. The system achieves both stabilisation, via a system of non-disposable articulated arms, and a bloodless surgical field, through the use of elastic bands.
We believe this case underlines the importance of multidisciplinary teamwork as the best strategy in repeat coronary procedures. Depending on the anatomical characteristics of the lesions and the clinical situation of the patient, we should choose between PCI or CABG. Interventional cardiologists and surgeons should work together in a multidisciplinary approach to select the best therapeutic option for the patient4.
Online data supplement
Video 1. Coronary angiogram showing a 90% LAD lesion.
Video 2. Coronary angiogram showing occlusion of the LIMA-LAD graft.
Video 3. Angiogram showing the outcome of PCI of the proximal and middle LAD.
Supplementary data
To read the full content of this article, please download the PDF.
Vidéo 1
Vidéo 2
Vidéo 3

