Abstract
Aims: The aim of the study was to investigate the 20-year trends in rates, patient selection and prognosis of coronary revascularisations in Finland.
Methods and results: We identified patients from nationwide registers who had undergone first-ever percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) between 1994 and 2013. We examined changes in procedure rates, patient characteristics and estimated hazard ratios (HR) and 95% confidence intervals for cardiovascular events during this period. Between 1994 and 2013, 85,482 PCIs and 74,338 CABGs were performed. During this period, PCI rates more than quadrupled while CABG rates declined by two thirds. Between 1994-1998 and 2009-2013, the proportion of urgent procedures and mean patient age increased while the proportion of women remained stable. Although unadjusted mortality rose, the multivariable-adjusted HRs for 28-day mortality (PCI: 0.62 [0.49-0.79]; CABG: 0.62 [0.54-0.72]) and five-year incidence of cardiovascular death (PCI: 0.72 [0.66-0.80]; CABG: 0.77 [0.72-0.83]), myocardial infarction (PCI: 0.47 [0.44-0.50]; CABG: 0.31 [0.29-0.32]) and stroke (PCI: 0.37 [0.34-0.40]; CABG: 0.36 [0.33-0.38]) were lower in the last five-year period than in the period 1994-1998.
Conclusions: Although revascularisation patients are older than before, post-procedural prognosis has improved drastically in recent years. Understanding the changing characteristics and prognosis of these patients is important for the interpretation of previous and future studies.
Abbreviations
CABG: coronary artery bypass grafting
COURAGE: Clinical Outcomes Utilising Revascularisation and Aggressive Drug Evaluation
CVDR: Finnish Cardiovascular Diseases Register
PCI: percutaneous coronary intervention
SYNTAX: Synergy between PCI with Taxus and Cardiac Surgery
Introduction
Percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) are standard revascularisation methods in patients presenting with significant coronary artery disease1. Since the late 1980s when PCI was introduced into wider clinical practice, the number of PCIs has rapidly overtaken the number of CABGs2. While CABG is associated with early morbidity and work disability, PCI is less invasive but more likely to be followed by repeat revascularisation3. In the last two decades, PCI procedure has evolved greatly from the use of plain old balloon angioplasty to bare metal stents and eventually to first- and newer-generation drug-eluting stents4-6. In addition to changes in procedural techniques, recent guidelines also recommend increasingly aggressive drug therapy with antiplatelet agents and statins in patients undergoing PCI and CABG7,8.
Despite the marked changes in revascularisation techniques and drug therapy, longitudinal, up-to-date, nationwide, large-scale data on patients undergoing coronary revascularisation are scarce, as most previous publications have been based on regional administrative registers with limited representativeness. Specifically, there is an unmet need for data describing how patient selection, gender distribution, revascularisation indications, and the relative proportion of PCI vs. CABG have changed over time. In addition, it is both an economic and a public health issue whether the new revascularisation techniques and drug therapies have resulted in improved short- and long-term outcomes post CABG and post PCI.
We therefore identified all patients who had undergone first-ever PCI or CABG between 1994 and 2013 in Finland from two nationwide registers whilst simultaneously assessing the validity and coverage of the Finnish registry data for coronary revascularisations. Our aim was to examine the 20-year changes in rates, patient selection and prognosis of coronary revascularisations in Finland.
Methods
DATA SOURCES AND STUDY POPULATION
Data from three nationwide administrative registers, the Hospital Discharge, Finnish Drug Reimbursement and the Causes of Death Registers, were used and linked on an individual level based on a personal ID code to form the Finnish Cardiovascular Diseases Register (CVDR). The National Hospital Discharge Register is maintained by the National Institute for Health and Welfare and, as mandated by law, comprehensively covers all periods of public and private inpatient care in all Finnish hospitals from 1967 onwards. The register contains information on diagnoses and procedures which have been performed during the periods of care and also includes a separate page designed for more detailed data collection on invasive cardiac procedures. The Drug Reimbursement Register is maintained by the Finnish Social Insurance Institution and contains nationwide information on data on all reimbursed drug purchases and entitlements to special reimbursement due to chronic diseases. The National Causes of Death Register is maintained by Statistics Finland and contains information on the underlying, contributing and immediate causes of death.
Diagnoses in the Hospital Discharge and Causes of Death Registers are recorded by the treating physicians with codes defined in the Finnish version of the 9th (ICD-9, until 1995) and 10th revisions of the International Classification of Diseases (ICD-10, 1996 onwards). Information on CABGs and PCIs are registered in the Hospital Discharge Register with codes defined by the Finnish Hospital Association (until 1995) and the Nordic Medico-Statistical Committee (1996 onwards).
Based on the procedure codes recorded in the Hospital Discharge Register, we identified 74,338 and 85,482 patients with a first CABG or PCI in Finland between 1994 and 2013, respectively.
FOLLOW-UP AND OUTCOMES
Follow-up data were accumulated until December 2013. The outcome events during the follow-up were identified from the National Hospital Discharge Register and from the Causes of Death Register. Due to the countrywide nature of these registers, the coverage of the follow-up, including out-of-hospital deaths, was 100% for people who continued to live in Finland. Only people who have permanently emigrated abroad are lost to follow-up and among elderly coronary patients this proportion is negligible. The validity of coronary, stroke and heart failure diagnoses in the Finnish registers has been described and validated in detail previously9-11.
Four endpoints were used in the study: all-cause mortality, cardiovascular mortality, myocardial infarction and stroke. Cardiovascular mortality was defined as mortality related to disease of the circulatory system (ICD-9 codes 410-414, 798, 79599, 76921, 431, 4330A, 4331A, 4339A, 4340A, 4341A, 4349A and 436; and ICD-10 codes I20-I25, I46, R96, R98, I61, I63 and I64) as the underlying, contributing or immediate cause of death. Myocardial infarction was defined with ICD-9 code 410 and ICD-10 codes I21 and I22 as a hospital discharge diagnosis or as the underlying, contributing or immediate cause of death. Stroke, excluding subarachnoidal haemorrhage, was defined with ICD-9 codes 431, 4330A, 4331A, 4339A, 4340A, 4341A, 4349A, 436 and ICD-10 codes I61, I63 (not I63.6 and I64) as a hospital discharge diagnosis or as the underlying, contributing or immediate cause of death.
STATISTICAL METHODS
The numbers of first-ever PCIs and CABGs per year are reported as age-standardised rates separately for men and women over 35 years. Age-standardised rates were calculated using the European Standard Population that dates back to 197612. To assess the longitudinal changes in post-procedural outcomes, we divided the patients into four categories by the year of the first coronary revascularisation: 1994-1998, 1999-2003, 2004-2008, and 2009-2013. Trends in patient characteristics across the time strata were compared using the Cochran-Armitage trend test for categorical variables and regression analysis for continuous variables. Survival rates were assessed with Kaplan-Meier curves. We used Cox regression models with follow-up truncated at five years to estimate the hazard ratios for post-procedural cardiovascular events in different time periods. 1994-1998 was used as the reference category. In addition, Cox regression was used to assess the 28-day post-procedural hazard of all-cause mortality in the different time periods. The validity of the proportional hazards assumptions was evaluated by plotting the Schoenfeld residuals of each covariate against time. The models were adjusted for sex, age, urgency of procedure, diabetes (yes/no), hypertension (yes/no), chronic lung disease (yes/no), previous MI status (yes/no) and previous stroke status (yes/no). A patient was considered to have prevalent diabetes, hypertension or chronic lung disease (i.e., asthma or chronic obstructive pulmonary disease) if an entitlement to special medicine reimbursement for the disease in question had been recorded in the Drug Reimbursement Register or an ICD diagnosis code matching with these diseases was found in the Hospital Discharge Register prior to the coronary procedure. After 2003, a procedure was defined as urgent if it was necessary to perform the procedure within one week (usually in case of acute coronary syndrome). Before 2003, when this information was not available, all procedures in which the patient had arrived in the hospital through the emergency room were defined as urgent.
Results
VALIDATION AND COVERAGE OF THE CVDR PROCEDURE DATA
To study the validity and coverage of our register, the procedures found in the CVDR were compared to those found in three separate data sources. First, we compared the number of procedures of the CVDR with those reported by the chiefs of cardiology and cardiac surgery to the Finnish Cardiac Society between 2006 and 2011 (Table 1). There were 16% more CABG procedures found in the CVDR than the number reported by the department chiefs, while 20% fewer PCI procedures were found.
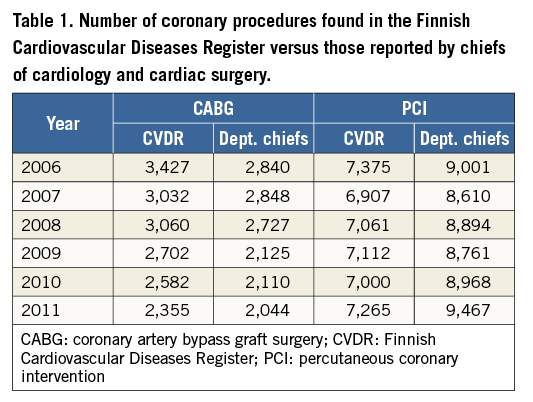
Second, a nationwide health survey with a nationwide randomised sample of approximately 10,000 individuals is performed every five years in Finland10. The self-reported information on CABGs, PCIs and procedure years from the 2002, 2007 and 2012 surveys were compared with the procedures found in the CVDR. Ninety-four percent (186 out of 197) of the CABGs reported by the participants of the FINRISK survey were found in the CVDR. In addition, 186 out of 188 CABGs found in the CVDR were also self-reported by the FINRISK participants, resulting in a positive predictive value of 99%. Eighty-three percent of the self-reported PCIs were found in the CVDR. However, 20 survey participants who had self-reported a PCI had in fact undergone a coronary angiography without PCI and therefore 92% (206 of 225) of the self-reported PCIs were also found in the CVDR. In addition, 186 of 193 PCIs found in the CVDR were self-reported by the FINRISK participants, resulting in a positive predictive value of 97%.
Third, the FINAMI is a population-based myocardial infarction register, which covers five specific areas in Finland in which trained nurses, supervised by study physicians, collect the information on coronary events and revascularisations from hospital documents, death certificates, and autopsy reports9. The coronary procedure data found in the FINAMI register were compared with the CVDR data (for up to one year after the myocardial infarction). Ninety-five percent (1,035 of 1,088) of the CABGs in the FINAMI register were also found in the CVDR. For PCIs, the same figure was 90% (1,889 of 2,100).
TRENDS IN PCI AND CABG RATES
A total of 159,820 coronary revascularisations were performed in Finland between 1994 and 2013. The mean age of all PCI and CABG patients was 65.9 years and 28% were women. On average, 35% and 5% had experienced a previous myocardial infarction or stroke, respectively. Altogether, 41% of the procedures were urgent.
The trends in coronary interventions in Finland are depicted in Figure 1. In both men and women, the number of age-standardised first PCIs per 100,000 inhabitants per year more than quadrupled from 1994 to 2013 (men: 56 to 268; women: 20 to 99). The majority of this increase occurred between 1998 and 2004. From 1994 to 2013, the age-standardised rate of CABGs per 100,000 inhabitants (men: 290 to 95, women: 68 to 29) per year reduced by 67% in men and 57% in women. This reduction in the number of CABGs occurred quite steadily during the whole period.
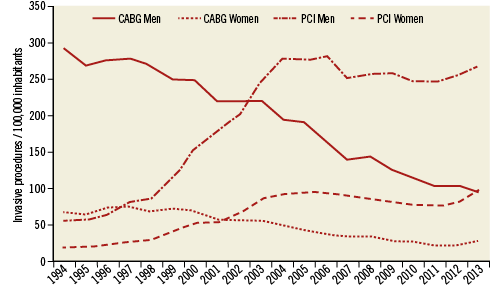
Figure 1. Trends in the number of first percutaneous coronary interventions and coronary artery bypass grafting in Finland in the period 1994-2013 by sex. The curves have been age-standardised according to the European Standard Population. CABG: coronary artery bypass graft surgery; PCI: percutaneous coronary intervention
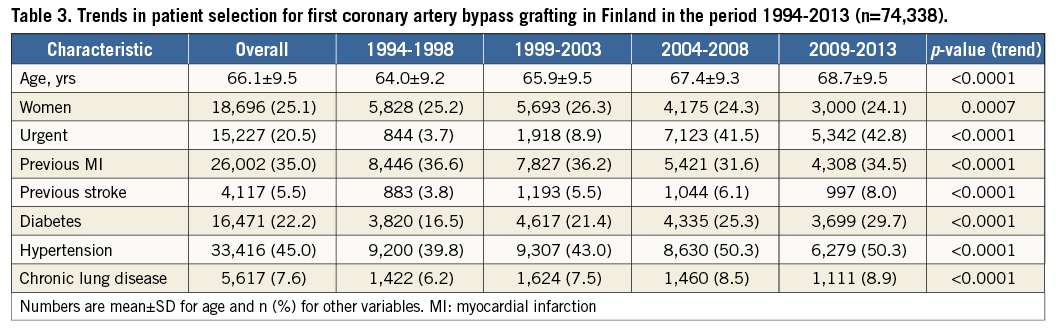
TRENDS IN PATIENT SELECTION
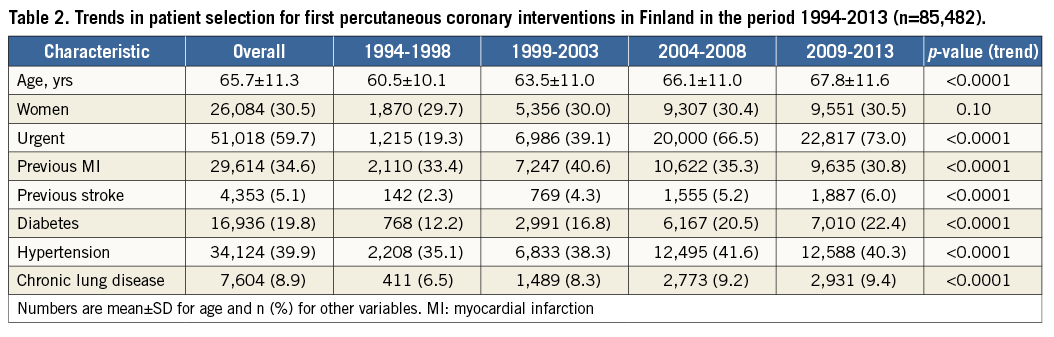
The trends in patient selection for first PCI or CABG in the four time strata are reported in Table 2 and Table 3. Between 1994 and 2013, the patients undergoing their first PCI or CABG became older and a greater proportion of patients underwent an urgent procedure. Although mostly statistically significant, no striking changes were observed in sex distribution or previous diagnoses of myocardial infarction and stroke.
TRENDS IN 28-DAY PROGNOSIS AFTER CORONARY PROCEDURES
The Kaplan-Meier curves and hazard ratios for all-cause mortality within 28 days after the procedure are presented in Table 4 and Figure 2. Although the crude hazard ratios for death post PCI and post CABG were significantly higher in 1999-2003, 2004-2008 and 2009-2013 than they were in 1994-1998, the fully adjusted hazard ratios were significantly lower during the latter time periods. However, the improving trend in post-procedural outcomes seems to have stopped after 2004-2008. The post-procedural risk of death in later time periods was similar to 1994-1998 if the large increase in the proportion of urgent procedures is not adjusted for.

TRENDS IN FIVE-YEAR PROGNOSIS AFTER CORONARY PROCEDURES
The Kaplan-Meier curves and hazard ratios for the five-year incidence of cardiovascular death, myocardial infarction and stroke are presented in Table 5, Table 6, Figure 2, and Figure 3. Both the crude and adjusted hazard ratios for myocardial infarction and stroke post PCI and post CABG were significantly lower in 1999-2003 and 2004-2008 than they were in 1994-1998. Although the crude hazard ratios for cardiovascular death increased with time, the adjusted hazard ratios decreased with time. The increase in the proportion of urgent procedures had a smaller impact on the five-year risk of cardiovascular events than on the 28-day post-procedural risk of death.
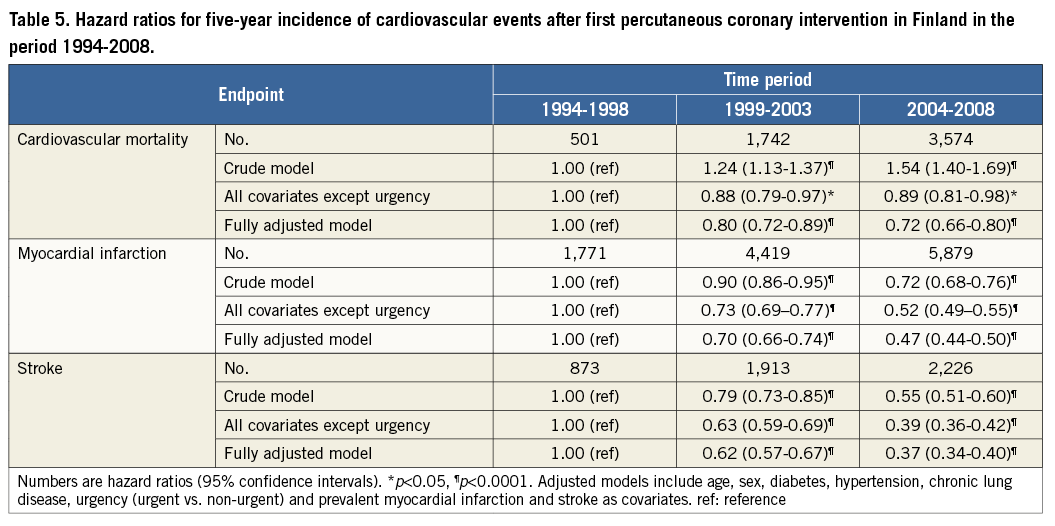
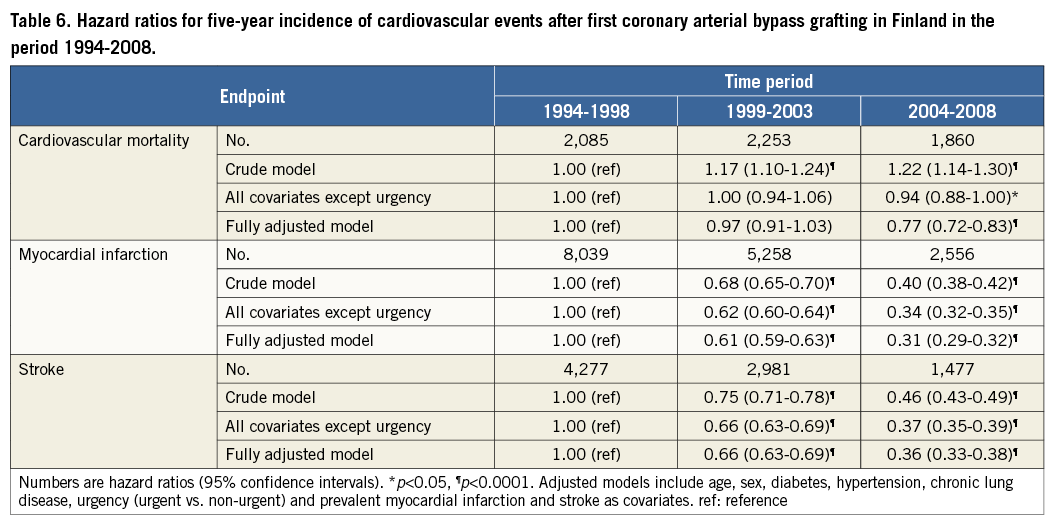
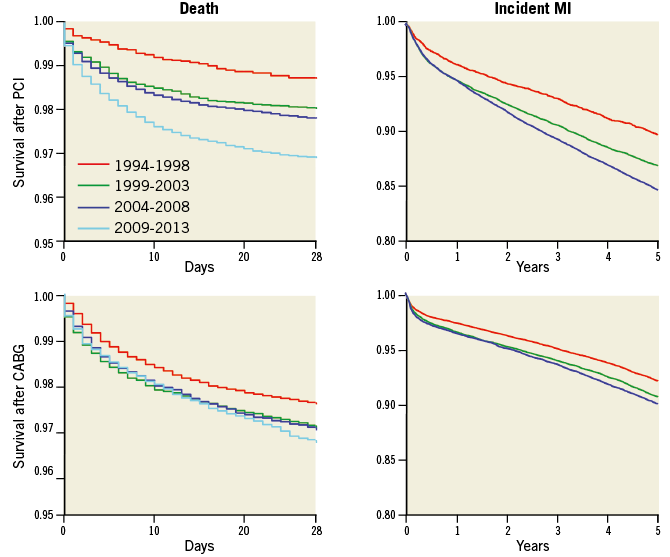
Figure 2. Kaplan-Meier curves for 28-day post-procedural mortality and five-year incidence of myocardial infarction after percutaneous coronary interventions and coronary artery bypass grafting in Finland in the period 1994-2013. CABG: coronary artery bypass graft surgery; MI: myocardial infarction; PCI: percutaneous coronary intervention
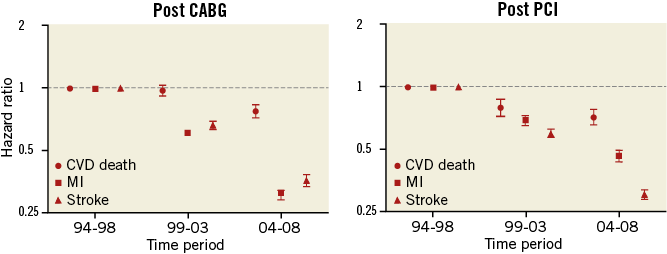
Figure 3. Multivariable-adjusted hazard ratios for five-year incidence of cardiovascular death, myocardial infarction and stroke after first percutaneous coronary interventions and coronary artery bypass grafting by time period. Vertical bars represent 95% confidence intervals. CABG: coronary artery bypass graft surgery; PCI: percutaneous coronary intervention
Discussion
This study describes for the first time the evolution of coronary revascularisation procedures from 1994 to the contemporary era in a nationwide setting in Finland. There are several trends evident from the data. First, a shift is seen towards more percutaneous procedures accompanied by the decline in surgical interventions with a plateau in recent years. Second, a smaller proportion of the procedures are elective and the patients are significantly older than 20 years ago. Third, both the short-term and long-term post-procedural prognoses of the patients have improved during the past two decades in spite of a most likely increased comorbidity burden. Fourth, the nationwide coverage and validity of coronary revascularisation procedures in the CVDR is good, as 90-95% of procedures which are self-reported or have been registered in a separate myocardial infarction register can also be found in our register.
The shifting balance from CABG to PCI in Finland mirrors the international trends in coronary revascularisation seen in many Western world societies such as the USA, UK and Sweden13-15. In Finland, the number of PCIs performed quadrupled and the number of CABGs declined by two thirds from 1994 to 2013. These figures are virtually identical to those reported from Sweden15. These findings could be partly explained by the less invasive nature of PCI which allows relatively safe treatment of symptomatic yet prognostically benign stable angina when compared to the unequivocal invasiveness of CABG. In addition to changes in procedure types, the mean age of patients undergoing CABG and PCI revascularisation has increased by four and seven years for CABG and PCI, respectively, in Finland during the past 20 years. This increase in age in PCI patients is similar to that reported from Sweden between 1990 and 201015. Although the focus of this study was not to examine the comorbidities of the patients, the comorbidity burden most likely increased due to the patients becoming markedly older.
In order to interpret the results of clinical trials and registers, it is necessary to understand how the PCI population has changed over time. In our study, the indication for revascularisation evolved towards urgent procedures from 1994 to 2013 in patients undergoing both CABG and PCI. Whereas in 1994-1998 only every fifth PCI was performed with an urgent indication, the rate was three out of four in 2009-2013. Similarly, the rate for urgent CABG rose from 3.7% to 42.9% in the same time period. The rate of urgent PCI procedures in Finland is in line with Swedish registry data15, but much higher compared to data from the UK16. Several administrative and strategic changes account for the changes in the rates and indication of the patient selection. The number of hospitals performing CABG rose to eight during the study period while it fell to six afterwards. Reflecting the PCI practice in the Western world, bare metal stents were first used in 1994; the first primary PCI was performed in 1996 in Finland. Nevertheless, generally the delay to invasive assessment of symptomatic stable disease or ACS was weeks to months in the 1990s. The widespread use of percutaneous interventional procedures evolved only after the year 2000 with the establishment of new catheterisation lab sites around the country. This explains the low urgency rate in the first time period 1994-1998 and the higher rates thereafter. In addition, indications for urgent PCI and CABG have also changed with accumulating scientific evidence and other improvements, such as the introduction of highly sensitive troponins. Altogether, 15 central hospitals started their PCI programmes (most of them between 2001 and 2006) without on-site surgery back-up also including treatment of urgent cases. The Finnish healthcare system is distinctive because distances to PCI hospitals are long due to the large land area and one of the lowest population densities in the Western world. In order to minimise excessive delays in primary PCI, a vast network of PCI hospitals is needed. In spite of these geographical challenges, the proportion of urgent procedures of all PCIs and CABGs is currently relatively high in Finland.
Between 1994 and 2013, the proportion of women undergoing revascularisation procedures varied between 24.1% and 26.3% and 29.7% and 30.5% for CABG and PCI, respectively. These numbers are clearly higher than those reported in clinical trials such as SYNTAX or COURAGE3,17, and slightly higher than in “real-world” registries such as the Swedish Coronary Angiography and Angioplasty Registry and the British Cardiovascular Intervention Society15,16, yet lower than those reported from the USA13,18. Although the absolute number of procedures increased over fourfold between 1994 and 2013, no clinically meaningful changes in gender distribution occurred in PCI or CABG patients in the same time period. This phenomenon has two clinical implications. First of all, because the ratio between men’s and women’s age-standardised mortality rates is approximately the same in Finland as it is in Sweden and the United Kingdom, it could be that the gender equality in access to coronary revascularisations is better in Finland than in some other countries19,20. Second, despite the increasing age and comorbidity burden of patients undergoing coronary revascularisation, the patient selection for these procedures has remained as gender-neutral as before.
These register-based results provide clear-cut evidence that MI, stroke and mortality rates after revascularisation have continued to decrease in Finland during the past 20 years. This decrease is most probably explained by better secondary prevention of cardiovascular disease including the widespread use of statins since the late 1990s21, and adenosine diphosphate receptor inhibitors since the early 2000s in the medical management of these patients. Strikingly, both short-term mortality and long-term mortality have decreased dramatically since 1994-1998. Moreover, a phenomenal evolution of percutaneous techniques has also occurred from simple plain old balloon angioplasty to bare metal stents and eventually to newer-generation drug-eluting stents, consequently diminishing the occurrence of restenosis and stent thrombosis, which in turn has allowed more confidence in the percutaneous treatment of more complex pathologies. In addition, cardiac care units have been proliferating since Killip and Kimbal demonstrated a 20% reduction in mortality for acute coronary syndrome patients treated in a cardiac care unit setting22. During our study period, cardiac care units have been adopted gradually in virtually every Finnish hospital that treats acute coronary syndrome invasively. Concomitant advances in perioperative and intensive care account for a great deal of improvement in short-term results, especially after surgical revascularisation, although the evolution of intensive care is best seen in the relatively steady mortality rates over the years despite an equally steadily advancing risk profile23. In fact, while coronary revascularisation may be essential for the treated patients, it is a sobering thought that invasive treatment is estimated to account for only 15% of the 47% decline in coronary artery disease mortality seen, for example, between 1980 and 200024.
Limitations
Despite the advantages of our study, such as a large unselected nationwide population, the results of our analyses must be interpreted within the context of their potential limitations. First, data from observational registries have more missing data and data that are of lower quality than randomised clinical trials. However, the representativeness and generalisability of nationwide data are fundamentally different from data from clinical trials. Also, as demonstrated by our validation, the coverage of our coronary procedure register is good as compared with self-reported and specific MI register-based data. In addition, the cardiovascular diagnoses in the Finnish registers have been successfully validated previously9-11. Second, the definitions of the procedures and endpoints, excluding death, may have changed slightly during the past 20 years. Third, all relevant covariates, such as pre- and post-procedural medication, disease severity variables such as left ventricular ejection fraction and angiographic extent of disease were not available, which would have allowed us to examine more closely the underlying causes behind the improved post-procedural outcomes.
Conclusion
This nationwide study on the trends in surgical and percutaneous coronary interventions and their outcomes spanning 20 years demonstrates that patient selection characteristics have changed substantially over time in terms of increasing age, more frequent urgent procedures and thereby a most likely higher comorbidity burden. However, despite revascularisations being performed in more challenging patients, a drastic improvement in the short- and long-term outcomes after PCI and CABG is evident. Understanding the changing characteristics and prognosis of these patients is important for the interpretation of previous and future cohort studies and trials.
| Impact on daily practice Although revascularisation patients are older than before and the proportion of urgent procedures has increased, post-procedural prognosis has improved drastically in recent years. Understanding the changing characteristics and prognosis of these patients is important for the interpretation of previous and future studies. |
Funding
Veikko Salomaa was supported by a grant from the Finnish Foundation for Cardiovascular Research.
Conflict of interest statement
The authors have no conflicts of interest to declare.