Abstract
Aims: With advancement in technology, the number of percutaneous coronary interventions performed are rising. The goal of this study was to evaluate nationwide trend over a long period of time in the utilisation of percutaneous coronary intervention (PCI) using a large database.
Methods and results: The Nationwide Inpatient Sample (NIS) database was utilised to calculate the age-adjusted rate for PCI from 1988 to 2004. Specific ICD-9-CM codes for all PCIs were used to compile the data. The NIS database contained 1,747,736 patients who had PCI performed from 1988 to 2004. The mean age for these patients was 63.75±11.07 years old. From 1988, the age-adjusted rate for all PCI gradually increased to more than three times until 2001 (80.3 per 100,000 [95%CI=71.86-88.92] in 1988 and 244 per 100,000 [95%CI=221.31-266.39, p<0.01] in 2001), but remained relatively unchanged (slight decline in the last few years of the study) until the end of the study (232.17 per 100,000 95%CI=211.69-252.66) in 2004. These trends were similar across ethnicity, gender and comorbid conditions.
Conclusions: The utilisation of PCI has dramatically increased from 1988 to 2001, but remained steady thereafter. The availability of drug eluting stents in the USA after 2001 may have contributed to this trend.
Introduction
Percutaneous coronary intervention (PCI) has become a very common procedure in the United States and primary PCI is becoming the strategy of choice in many hospitals with a cardiac catheterisation laboratory. PCI can maintain complete and sustained restoration of flow to the coronary artery. Meta-analyses of randomised clinical trials have demonstrated that primary PCI in cases of acute myocardial infarction is better than fibrinolysis at reducing death, re-infarction, and stroke; it was also more cost-effective.1-3 Though PCI has been widely used, the trends have not been well studied in a large population and across ethnicities. In this study we sought to evaluate nationwide trends in the utilisation of percutaneous coronary intervention (PCI) in the past in comparison to recent years using a large inpatient database that ranged from 1988 to 2004.
Methods
Data collection and data sources
The Nationwide Inpatient Sample (NIS)4 is a set of longitudinal hospital inpatient databases included in the Healthcare Cost and Utilisation Project (HCUP). These databases are created by the Agency for Healthcare Research and Quality (AHRQ) through a federal-state-industry partnership. HCUP data informs decision making at the national, state, and community levels. Researchers and policymakers use the NIS to identify, track, and analyse national trends in health care utilisation, access, charges, quality, and outcomes. The NIS is the largest all-payer inpatient care database and contains data from approximately eight million hospital stays each year in the USA. This database is comprised of a 20% stratified sample of patients from all participating community hospitals across the United States, making it one of the largest representative inpatient databases in the USA. NIS data are available from 1988 to 2004, allowing analysis of trends over time. The number of states represented in the NIS has grown to 38 at present. The NIS is a national hospital database containing charge information on all patients, regardless of payer, including persons covered by Medicare, Medicaid, private insurance, and the uninsured. It also contains primary and secondary diagnoses, primary and secondary procedures, demographics, admission and discharge status with safeguards to protect the privacy of individual patients, physicians, and hospitals. In this study we evaluated the age- adjusted prevalence rate per 100,000 hospitalisations for PCI coded as primary procedure.
Furthermore, we performed subgroup analysis of PCI trends based on gender, race and comorbid conditions such as congestive heart failure (CHF), diabetes, ST elevation myocardial infarction (STEMI) or non-ST elevation myocardial infarction (Non-STEMI)
Description of the data
In this study we utilised International Classification of Diseases, ninth revision, Clinical Modification (ICD-9-CM) . The primary code for PCI (36.01, 36.02, 36.03, 36.05, 36.6, 36.07) as discharged diagnosis from NIS hospitals was used for our analysis. By using the NIS database, we obtained demographic information such as gender, ethnicity and age per 100,000 hospitalisations during the period 1988-2004. Detail information about NIS participating hospitals over the years can be seen at the NIS website at: http://www.hcup-us.ahrq.gov/databases.jsp. Table and Figure 1-2 summarise some of the population studied in the NIS data base.
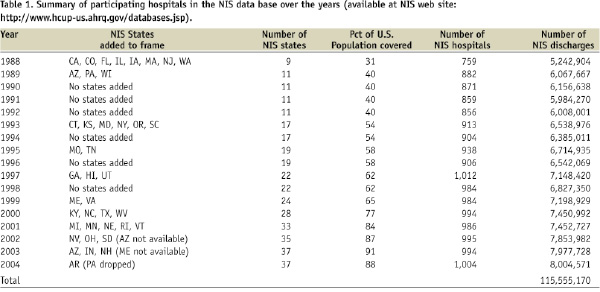
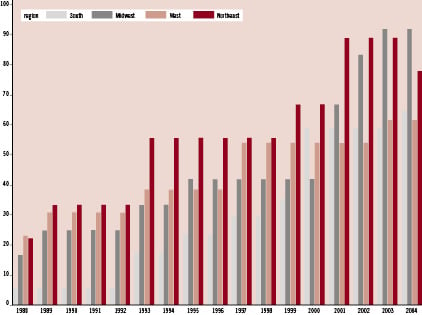
Figure 1. Percentage of states covered by NIS, by region (available at NIS web site: http://www.hcup-us.ahrq.gov/databases.jsp).
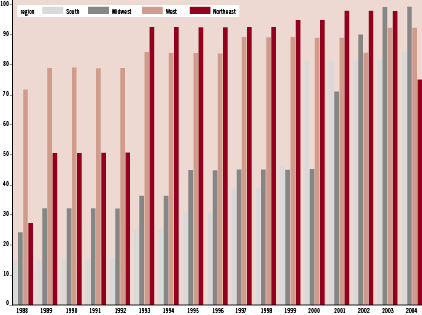
Figure 2. Percentage of population covered by NIS states by region (available at NIS web site: http://www.hcup-us.ahrq.gov/databases.jsp).
Statistical analysis
The average age-adjusted rates for PCI and 95% confidence intervals (95% CI) for each year were analysed by multiplying the age-specific rates of PCI by age-specific weights. The weighted rates were calculated for each year from 1988 to 2004, then summed across the age groups for the calculation of age-adjusted rate. The weights used in the age-adjustment of the data were the proportion of the year 2000 standard USA population within each age group. We used Statistical Package for the Social Sciences (SPSS) software13 for our analysis. Quantitative variables were expressed as means _ standard deviation (SD). For comparison, the Independent Samples T-Test was used. Furthermore, we calculated the rates of the reported procedure over time using calendar year, race, age, and gender. A p-value of <0.05 was deemed as statistically significant.
Results
The NIS database contained 1,747,736 patients who had PCI performed from 1988 to 2004. The mean age for these patients was 63.75±11.07 years old. Males underwent PCI twice as often as females (male: 66.27, female 33.73). From 1988, the age-adjusted rate for all PCI gradually increased to more than three times until 2001 (80.3 per 100,000 [95%CI=71.86-88.92] in 1988 and 244 per 100,000 [95%CI=221.31-266.39, p<0.01] in 2001), but remained relatively unchanged (slight decline in last few years of the study) until the end of the study in 2004 (232.17 per 100,000 [95%CI=211.69-252.66] in 2004). These trends were similar across ethnicity and gender. However, PCI utilisation rates for women, African Americans and minorities were much lower in comparison to men and Caucasians (Figures 3 and 4).
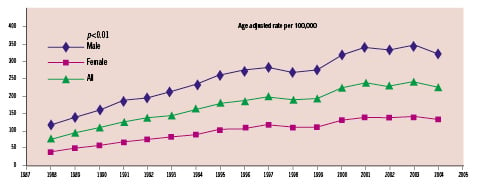
Figure 3. Age adjusted rate of PCI per 100,000 based on gender.
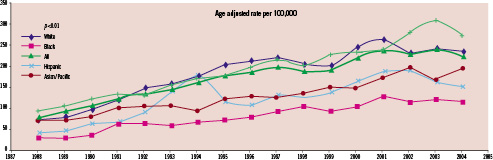
Figure 4. Age adjusted rate of PCI per 100,000 based on ethnicity.
Furthermore, our subgroup analysis revealed similar rates in the PCI utilisations in patients with type 2 diabetes mellitus, CHF and non-STEMI (Figure 5). However, the PCI trend for patients with the diagnosis of STEMI mildly declined after a steady increase in the recent years (Figure 5).
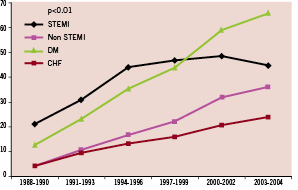
Figure 5. Age adjusted rate of PCI per 100,000 based on history of diabetes mellitus, congestive heart failure, STEMI and non-STEMI.
Discussion
Cardiovascular disease is the leading cause of mortality in the USA and developed countries. Multiple randomised clinical trials have shown that primary PCI is better than fibrinolysis.1,2 The use of primary PCI has grown considerably in hospitals in recent years and there is improvement in observed and expected hospital mortality rates attributed to greater use of PCI.5 A study from an urban community in the USA suggested that, initially, the usage of thrombolytic therapy increased from the mid 1980s to the early 1990s with a progressive decline in use thereafter. Additionally, there was a marked increase over the past two decades with 3.5% of patients treated with thrombolysis vs. 42.1% treated with PCI during hospitalisation for acute myocardial infarction (AMI) in 2003.6
A study on revascularisation utilisation from 1990 to 2004 suggested a 69% increase in PCI accompanied by a 33% decrease in CABG with an increase of 24% in total revascularisation.7 This finding is consistent with our results that the utilisation of PCI has dramatically increased to more than double from 1988 to 2001, but remained unchanged thereafter. The reason for the lack of steady increase in PCI rate in the more recent years is unknown. It could be related to the approval of drug eluting stents reducing PCI in the setting of in-stent restenosis or secondary to aggressive lipid lowering treatments. Introduction of drug eluting has shown a significant advantage over the bare metal stents, which has reduced the rate of revascularisation and re-hospitalisation in various age groups.8 Also, the addition of glycoprotein IIb/IIIa inhibitors before PCI has further improved the outcomes. In a meta-analysis of nine trials in diabetic patients it was concluded that GP IIb/IIIa inhibitors decreased the rate of myocardial infarction (MI) at 30 days (1.1% vs. 3.3%) and at one year (1.1% vs. 4.7%,).9 The beneficial effect of aggressive lipid lowering therapy and increased utilisation of statin therapy in patients at-risk or in patients with documented coronary artery disease has most likely contributed to the lower cardiovascular event rates leading to the recent decline in PCI procedures. The recently published Optimal Medical Therapy With or Without PCI for Stable Coronary Disease (COURAGE) trial10 confirms the beneficial effect of optimal medical therapy that could be as effective as PCI in patients with significant coronary disease. This finding would probably cause further decline in the rate of PCI.
Our study showed that males underwent PCI at twice the rate of females (male: 66.27, female: 33.73). This is most likely related to a lower age-adjusted rate of coronary artery disease in women. Although previous studies have shown that the risk profile and absolute adverse event rates in women are higher than in men11,12, in a recent report from registry review of gender differences in mortality after percutaneous coronary intervention (PCI) it was suggested that there were no significant differences in short-term or long-term mortality observed between men and women. Our data match published data using the American College of Cardiology established National Cardiovascular Data registry (AAC-NCDR) in regards to the population studied.13 They found that 34% of women underwent PCI similar to our data of 33.7%. Their average age was also identical to our average age (64 vs. 63.7). This suggests that our data is a valid representation of patients undergoing PCI in the US. Furthermore, an increasing trend found in our study is concordant to the published European data by Cook et al showing steady increase in the utilisation of PCI procedures across Europe.14
Furthermore, we found that increasing in the utilisation of PCI trend persist for patient presenting with the diagnosis of CHF, diabetes and non-STEMI suggesting that comorbid condition has no important rule in the increase utilisation of PCI. However, we found that PCI rate for patients with the diagnosis of STEMI stabilised in the recent years with mild decline. The cause of this finding is most likely related to the lower incidence of STEMI in the recent years in the United States that has been recently presented.15 Furthermore, our study confirms previous findings of lower PCI utilisation rates in minorities in the United States warranting further investigation.
In conclusion
Our study demonstrated an increase in utilisation of PCI from 1998 to 2001 and relatively no further change after 2001. The increase, and subsequent levelling of usage, is most likely due to a result of approval of drug eluting stents or secondary to aggressive lipid lowering strategy with similar trends across ethnicity and sex.
Limitations
We used ICD-9 code based on administrative coding which has inherited limitations in diagnosis accuracy, limiting our analysis. Changes in coding over the study years could have caused some inaccuracy in the reported data.

