Abstract
Aims: Drug-eluting stents (DES) have shown to reduce restenosis rates in all lesional subsets. This has expanded the application of percutaneous intervention (PCI). In this study we address the impact of the high DES penetration on the management of patients referred for coronary angiography.
Methods and results: We have studied the cohorts of patients referred for coronary angiography in 2000-2001 prior to DES availability, and in 2005-2006 with a 73% DES implementation. In 2000-1 of 2,458 coronary angiographic studies, 84% had significant lesions (>50%), 56% had PCI, 8.8% had CABG and in 443 (18%) with significant lesions no revascularisation was attempted. In 2005-6 out of 2,600 angiographies, 84% had significant lesions, 64% had PCI, 6% had CABG and in 312 (12%) with significant lesions no revascularisation was done. The increase in PCI, the reduction in CABG and the decrease in non-revascularised diseased cases were all significant (p<0,001). The PCI and CABG groups in 2005-6 compared to 2000-1 had a more complex lesion profile with, however, less in-stent restenotic lesions treated (10% vs 4.2%; p<0.001).
Conclusions: The wide clinical introduction of DES was associated with a significant increase in patients undergoing any kind of revascularisation, increasing the PCI volume to the detriment of CABG activity. Patients with PCI in 2006 had more complex lesions treated, whereas restenosis was less frequent.
Introduction
The actual standard of care of coronary artery disease includes both coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) as revascularisation tools. The latter has recently experienced a great revolution following the advent of drug eluting stents (DES). These devices have clearly diminished the restenosis rate in different lesional and clinical subsets1-7. This has lead to a spread in percutaneous revascularisation indications, including not only more complex lesions, but also multivessel disease and left main coronary artery involvement8-13.
The efficacy of DES has been evaluated in many different settings, but the impact of its use regarding the choice between the two different revascularisation options has not been well assessed. In our study, we sought to discern how the introduction of DES and its frequent use in the interventional laboratory has influenced the amount as well as the profile of the patients sent to each of these treatment modalities.
Methods
Patients and design
We studied two different periods of time (two years each). All patients that where sent consecutively to our hospital (a tertiary referral centre) for an angiography to rule out ischaemic coronary artery disease in each period were included. The first cohort involved the two years prior to the introduction of DES (2000 and 2001: BMS group) and the second one comprised the years 2005 and 2006 (DES group), when the employment of DES was part of current clinical practice with a rate of use of 73% related to the total of stents implanted (ranging from 60% in the first trimester to 77% in the last one). In the latter period, the criteria for use of BMS were the following: chronic oral anticoagulation, low platelet count, patient life expectancy <1 year, known allergies to clopidogrel or aspirin, recent major haemorrhage, any previous cerebral bleeding episode, active gastric ulcer, planned surgery in the following year and acute STEMI with cardiogenic shock or large thrombus or large vessel (>3 mm) without long lesion (<20 mm).
Demographic, clinical and angiographic characteristics of all the patients were collected as well as strategy of choice, procedural characteristics and adverse effects. All data were obtained from individual reports and charts available at the hospital, cardiology department and interventional cardiology unit data base and files. The information was evaluated and downloaded into a specific database by six cardiologists. Consensus was achieved for those cases showing any kind of conflicting data.
Statistics
Continuous variables are expressed as mean±standard deviation (SD) if the data are normally distributed, and as median and interquartile range if not (Kolmogorov-Smirnov test used to assess normal distribution). Categorical variables are presented as counts and percentages. Continuous variables were compared with two-tailed unpaired t test when normal distribution applied and otherwise with Mann-Whitney test. Categorical variables were compared with Chi-square or Fisher exact test as appropriate. All variables were compared in between the two different groups (BMS and DES). Statistical significance was assumed for p<0.05. Statistical analysis was performed with the use of SPSS 15.0.
Results
In the BMS period, 2,458 coronary angiographies were performed; 2,068 (84.1%) showed lesions greater than 50%, 1,383 (56%) patients underwent PCI and in 217 (8.8%) cases CABG was the treatment of choice. From the total of patients with >50% stenosis, 443 (18%) did not underwent any final intervention strategy. In the DES period, 2,600 coronariographies were performed; 2,179 (83.8%) showed lesions >50%, 1,665 (64%) patients underwent PCI and in 158 (6%) cases CABG was the treatment strategy. Out of the total of patients with lesions >50%, in 312 (12%) none of the two revascularisation options was used. (Table 1).
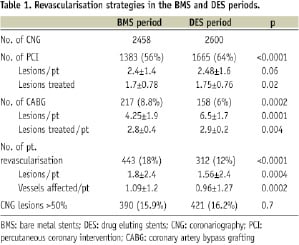
The rise in the proportion of cases treated with PCI, and the decline in both the percentage of surgical approach and the percentage of patients not undergoing revascularisation, was found to be statistically significant. In the DES period, the degree of coronary artery disease was greater in the subset of patients undergoing invasive therapy (especially those sent to CABG), and lower in the cohort of patients treated medically as compared to the BMS period.
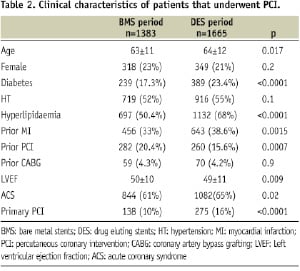
After comparing the clinical characteristics of the patients that underwent PCI in the two different periods of time, we found that the patients treated in the DES period were more likely to be older, have a worse lesion profile and have more diabetes mellitus, hyperlipidaemia, previous myocardial infarction (MI) and lower ejection fraction. The only characteristic that was less frequent in these patients was the antecedent of previous PCI (Table 2).
As shown in table 3, the characteristics of the procedures were widely and significantly different.

In the DES period, the number of lesions treated per patient was higher, the amount and length of the stents being also superior. More diffuse, small vessels, chronic total occlusion and left main lesions were treated as well as in the setting of an acute MI. There was an important reduction in the treatment of restenotic lesions which were highly related to BMS. An increment in the thrombosis rate (in most of the cases late thrombosis) was observed: however, it was not statistically significant. The immediate success rate, and the use of intravascular ultrasound were similar, as well as the in-hospital mortality.
Regarding the group of patients sent to CABG, the clinical and angiographic characteristics are shown in tables 4 and 5 respectively.

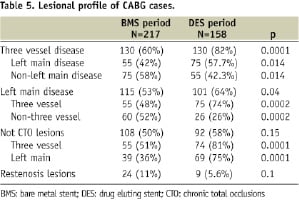
The patients that underwent CABG in the DES period were more likely to have diabetes mellitus, hyperlipidaemia and less likely to have chronic obstructive pulmonary disease (COPD) when compared to the BMS period, while the logistic EuroSCORE remained similar. The biggest differences were found in the lesion profile: the surgical patients in the latest period had more three vessels or left main coronary artery disease, often with overlapping of both characteristics, whereas there was a trend towards less restenotic and less total chronic occlusion lesions.
Discussion
In this study we are able to assess the preliminary, instinctive idea that the advent of DES has significantly increased the ratio of patients undergoing PCI. With a similar proportion of studies showing no significant lesions in both periods, the proportion of cases not undergoing any kind of revascularisation decreased from 18% to 12%. This was due to a higher proportion of patients undergoing PCI (56% to 64%) in the DES period, with a corresponding reduction in surgical rate (8.8% to 6%). The explanation could be a shift from CABG to ICP (mainly multivessel cases and some LMCA lesions amenable to PCI) which increases the complexity of the percutaneous group and worsens the surgical group.
Having taken this into account, it is remarkable that the need for procedures to treat restenotic lesions, both in PCI and CABG options, was significantly lower in the DES period, which testifies to its already proven efficacy. Of note, in the DES period, restenosis events still occur in the majority of cases in previously BMS treated lesions (BMS having been used at a lower rate in this interval).
Regarding stent thrombosis, it accounted for 1.4% of the whole activity in the DES period, as compared to 0.9% in the BMS period. A drop in subacute stent thrombosis incidence and a rise in the late stent thrombosis rate was observed in the second time period. The use of oral and intravenous antiplatelet therapy has certainly improved with the years, which could, to some extent, explain the lower subacute stent thrombosis incidence, whereas the rise in late stent thrombosis could be related to the use of DES.
The characteristics vessels seen in CABG recipients during the DES period are also more complex. These differences are only slightly reflected in their clinical profile. The DES period shows a mildly higher value of the logistic EuroSCORE, but this is not translated into a statistically significant difference. This paradox of a worse anatomic profile while presenting with a similar clinical profile could be the result of the fact that higher surgical risk three-vessel and left main coronary artery disease patients have been treated with PCI in the DES period.
The changes noted between the different periods regarding final interventional strategy could be related to other factors other than the use of DES such as changes in the profile of patients sent to coronariography or modifications in the cardiology, haemodynamic or surgical team strategies. However, this is quite unlikely for the following reasons:
1) The reference population is the same in both periods;
2) The number of coronariographies falls under a pre-determined incremental rate which is the same in all centres throughout our country. This higher number of patients sent to coronariography is not caused by an increase in patients with less coronary disease, because the ratio of patient with lesions >50% is the same;
3) The medical team has remained constant during this interval (2000-2006) without important changes. Neither have new protocols or clinical pathways been introduced that could have affected the main indications, with the exception of the primary use of primary PCI;
4) Apart from DES, no new devices have been introduced into the PCI armamentarium that could account for such an important spread. The mechanical characteristics of BMS in the 2000-2001 period was the same, if not better, than those of DES used in 2005-2006 and the employ of intravascular ultrasound (IVUS) was similar in both periods.
Therefore, the only factor that could have strongly influenced this is the use of DES. Their outcomes, both published and observed in daily practice have prompted the subsequent percutaneous approach for cases that otherwise would have been either managed surgically (multivessel and left main disease with higher surgical risk) or not revascularised (very small vessel or very long lesions).
Previous experiences
There are very few studies that have looked at the impact that DES could have on the revascularisation strategy, and most have only focused on partial aspects. The Rotterdam team published a study with this aim14. They compared a six months period of time in 2002 with a 100% DES penetration against the six previous months using BMS. In this first period, they treated 1,120 patients, 314 (28%) with CABG and in the period with DES, 1,073 patients, 275 (25.6%) with CABG. The authors found a more complex profile in both the patients that underwent PCI or CABG and a lower rate in the need for reintervention in the second period. The study evaluates shorter and consecutive periods of time, which implies that BMS restenosis cases were treated in the DES period. Also, stable changes introduced by the use of DES had not yet been established. Therefore, the impact in the number of cases sent to CABG can not be neatly studied. On the other hand, a DES implantation rate of 100% is very unusual and does not reflect daily practice in most hospitals14.
Another study evaluated only the change in the profile of cases treated with PCI after the influx of DES15. They analysed two consecutive years, the first one without, and the second one with DES, but with a very variable rate of DES use (ranging from a 49% in the first three months, to an 84% in the last three). They observed a change in a greater complexity of cases as well as a larger number of stents deployed per patient and an increase in the stent length. Concordant with our findings, the angiographic success rate and the in-hospital mortality remained similar15. The association of the widespread use of DES and the reduction in repeat procedures without any increase in death or infarction has been confirmed in large,recent studies16.
Other studies have only focused on the impact in the number and characteristics of patients sent to surgery. A study conducted at the Mayo Clinic sought to anticipate the impact that DES use would have in the quantity and profile of patients sent to CABG17. They reviewed the angiograms of those cases sent to CABG before the introduction of DES (1999-2001) and determined how many of those patients could have undergone DES PCI. They found that 46% of cases had lesions amenable for DES treatment (6% of lesions with similar characteristics to those included in clinical trials with DES, and 40% of lesions not yet included in DES trials published by the time the study was conducted in 2003).
Another study compared the surgical series of two different periods before and after widespread established use of DES, similar to what we have assessed in our study18. This study evaluated the surgical series of the year prior to implantation of DES (2002-2003) versus those of the year 2003-2004 when DES were widely used. A significant although small reduction in the number of patients sent to CABG (9.9% vs. 8.5%) was observed. Regarding the patient characteristics, they only found differences in the proportion of cases with left main disease (higher in the post DES group, 44% vs. 36%) and cases with ejection fraction <50% (lower in the post DES group, 45% vs. 52%). The authors concluded that the use of DES has increased the proportion of patients with left main disease and preserved ejection fraction in the surgical recipients, which implies that patients with multivessel disease and non-preserved ejection fraction are more likely to be treated with PCI. Finally, a Japanese study evaluated the impact of DES therapy over the volume of coronary surgery, showing a modest decrease (1.7% in DES era vs 1.9% in BMS era), with preoperative conditions becoming worse19. However, the very low proportion of cases sent to surgery in the BMS period account for such a modest decrease.
Limitations
The observational and retrospective design is the major limitation of this study. The evaluation of clinical experiences in different time periods is difficult and it is never possible to exclude the presence of factors, some of them already mentioned, and other not identified, that could have influenced in the changes observed; in any case, if these factors do really exist their relevance would be lower as compared to that of DES.
Conclusions
The wide use of DES has increased the global revascularisation rate, raising the amount of cases sent to PCI in detriment of CABG. This has made the lesion profile of cases sent to PCI to become much more complex, but has been related to a reduction in the restenosis rates as well. Patients undergoing CABG, although with a worse anatomical profile, do not suffer from a significant increase in surgical risk; this could be explained by the PCI approach for patients with three vessel or left main disease with higher surgical risk.

