Abstract
Aims: Few data document trends in cardiovascular (CV) risk-factors in patients with or without previous symptomatic CV disease. We assessed the prevalence and trends in (non) modifiable CV risk-factors, and the use of cardioprotective therapies in patients enrolled in coronary stent trials.
Methods and results: This analysis included prospective data on 10,253 mainly European adults who were enrolled in 32 coronary stent studies between 1995 and 2006. Data was collected at the time of enrolment using a standardised patient clinical record form, and was analysed by considering three consecutive time periods: 1995-1997 (I), 1998-2002 (II) and 2003-2006 (III) rendering approximately equal numbers per period. Overall the proportion of active smokers remained constant (Period I to III: 28%, 27%, 21%, p=0.45), however the proportion increased in females below 50 years (about 2%/ year, R.RR: 1.20, P: 0.05 period III versus I). Prevalent diabetes increased (16%, 17%, 25%; p=0.029). The prevalence of a body-mass index (BMI) ≥25 kg/m² was high, but no trend was observed (69%, 68%, 70%; p=0.24). The proportion of patients with elevated blood pressure (i.e., ≥140/90 mmHg, in diabetes ≥130/80 mmHg) remained unchanged (55%, 50.%, 53%; p=0.22), despite an increase in the number of patients taking anti-hypertensive agents (84%, 89%, 90%; p=0.30). Conversely, the proportion of patients with elevated total cholesterol (i.e., ≥4.5 mmol/L) decreased (80%, 66%, 52%; p=0.002), which was consistent with the increase in patients taking lipid lowering drugs (32%, 62%, 69%; p=0.083). The portion of patients reaching therapeutic targets for blood lipids improved, but no improvement was seen in blood pressure control (p=0.29).
Conclusions: There is an unmet clinical need in primary and secondary CV prevention in Europe. Patients requiring PCI are an important target population in whom lifestyle changes and aggressive secondary preventative measures should be aimed. Ultimately PCI should open the door towards optimising secondary prevention.
Introduction
Atherosclerosis and coronary thrombosis are a major cause of premature death worldwide, and are an important source of loss of disability-adjusted life years.1-3 As its clinical consequences are highly relevant for patients and society, so are the benefits of prevention. Effective prevention involves a strategy based on the knowledge of a population’s attributable risk, which itself is prone to variation as the prevalence of several risk factors may fluctuate within a population over time.4
Patients with established atherosclerotic cardiovascular disease (CVD) (coronary artery disease [CAD], cerebrovascular disease, and peripheral arterial disease [PAD]) are at particular risk of recurrent nonfatal and fatal cardiovascular (CV) events.5
The EUROASPIRE study group applied a cross-sectional design to assess trends in modifiable cardiovascular risk factors and medical treatment in CVD patients from 1995-96, 1999-2000, and 2006-07 in selected geographical areas and hospitals in Europe. The results were discouraging, and revealed a continuing gap between the standards set by guidelines on secondary cardiovascular risk prevention, and the results achieved in clinical practice.6 As per design, the EUROASPIRE surveys focussed on secondary prevention in routine clinical practice patients. We aimed to support the EUROASPIRE findings in the clinical trial setting, together with simultaneously addressing the aspect of primary prevention.
The prevalence of baseline demographics and the CV-risk profile of patients included in stent investigations is influenced by specific study inclusion and exclusion criteria, changes in the prevalence of CV-risk factors and related therapy, and may or may not mirror trends reported in routine clinical practice. This information is important when considering differences between trial results and extrapolations with routine clinical practice.
We conducted a retrospective analysis of prospectively collected data from stent trials conducted mainly in Europe by an Academic Research Organisation (ARO) over the last two decades focusing on modifiable CV-risk factors and medical treatment. The aim of the present investigation was to analyse apparent variations in overall CV-risk over time in this specific patient population.
Methods
Study population and data collection
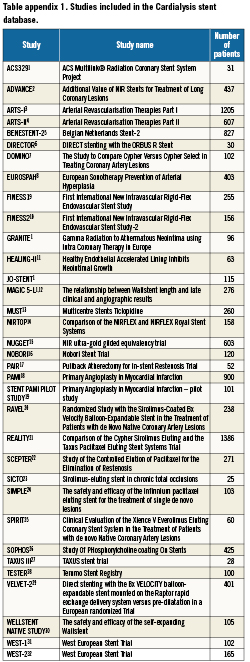
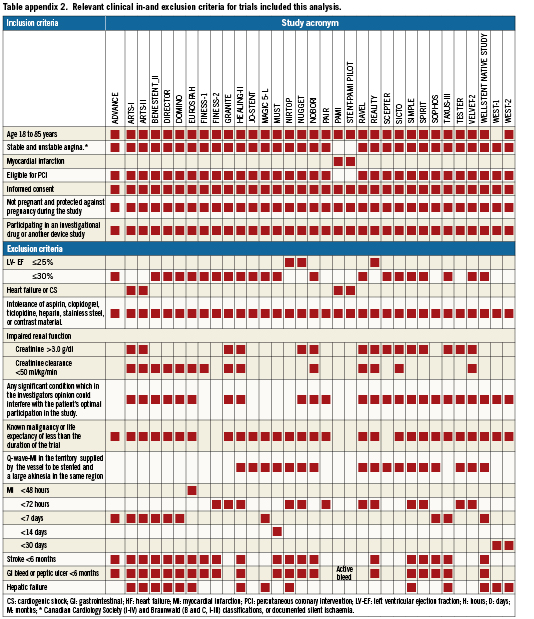
We analysed the baseline data sets of 10,253 patients, with angiographic proven obstructive atherosclerotic CAD, enrolled in one of 32 prospective, randomised native coronary stent trials conducted predominantly in Europe by a single independent ARO (Cardialysis, Rotterdam, The Netherlands) between 1995 and 2006 (last patient in 10/2006) All trials except two were registered in the ClinicalTrials.gov database [ClinicalTrials.gov]. A summary of all trials included in the current analysis, together with their inclusion and exclusion criteria are presented in Appendices 1 and 2, respectively. Detailed trial information and trial results are available elsewhere. Individual databases were managed by Cardialysis, Rotterdam, The Netherlands who conducted systematic audits and quality checks.
We addressed trends in the prevalence of diabetes and individual modifiable CV risk factors, together with the presence of established symptomatic atherosclerotic peripheral or cerebral arterial disease. Modifiable CV-risk factors considered in this analysis consisted of current smoking, systolic blood pressure (SBP), body mass index (BMI) and hypercholesterolaemia. Patients were classified as to their gender and age (men: 65 years or older; women 70 years or older). The cut-offs for age were arbitrary set considering the relation between age and cardiovascular disease in men and women with or without diabetes.7 The standard case record form (CRF) did not record the participants’ level of physical activity.
The use of cardioprotective drugs such as cholesterol lowering medications (statins, fibrates), antiplatelet drugs (clopidogrel, ticlopidine, aspirin), anti-hypertensive agents (beta-blockers, calcium antagonists, angiotensin-converting enzyme [ACE] inhibitors/angiotensin receptor blockers, diuretics) and any diabetic treatment prior to randomisation was systematically recorded. Information on contra-indications against the use or reasons for stopping or specific cardio-protective drugs could not be captured from the data base.
Each individual study was approved by the appropriate local regulatory and ethics committee of the participating trials. All participants provided informed consent before taking part in each of the individual studies.
Definitions
Information about the patient’s previous history of coronary or other atherosclerotic disease, reported medication, and baseline CV-risk factors were obtained via a standardised patient CRF used by the ARO in all stent trials, thus enabling the following definitions to be used in the current analysis:
Current smoking was defined as the consumption of an average of at least five cigarettes per day within the month prior to enrolment.
Prevalent diabetes mellitus was defined as a fasting serum glucose level ≥7.0 mmol/l (126mg/dl), non-fasting glucose level ≥11.1 mmol/l (200 mg/l), or a patient indicating a previous diagnosis of diabetes mellitus made by a physician, or the current use of diabetes medication. Diabetes treatment was specified: exercise/diet only, treatment with oral hypoglycaemic agents, or treatment with insulin.8
Prevalent hypertension was defined as a seated systolic (SBP) ≥140 mmHg and a diastolic (DBP) ≥90 mmHg, (except among patients with diabetes in whom this was defined as BP >130/80 mmHg). Patients were further stratified as “optimal” if mean SBP was <120 and diastolic pressure <80 mmHg, as “normal” if mean SBP was <130 mm Hg/DBP was 80-84 mm Hg and “high normal” if SBP 130-139 mmHg/DBP 85-89 mmHg.9 If the systolic and diastolic pressure readings belonged to different categories, the higher of the two readings was used to assign the blood-pressure category.
Body mass index was calculated as weight in kilograms divided by the square of height in meters. Patients were considered to be of normal weight, overweight or obese if their respective BMI’s were <25, 25≤ and <30, or ≥30.10
Established, symptomatic CVD5 consisted of one or more of the following criteria: history of unstable angina with documented obstructive CAD, history of percutaneous coronary intervention (PCI), history of coronary artery bypass grafting, or previous myocardial infarction (MI). Documented cerebrovascular disease consisted of a hospital or neurologist’s report with the diagnosis of transient ischaemic attack or ischaemic stroke. Documented PAD consisted of a history of intermittent claudication together with a previous and related intervention, such as angioplasty, stenting, atherectomy, peripheral arterial bypass graft, or other vascular intervention including amputation.
Prior MI was defined as either a self-reported history of physician diagnosed MI, or a history of MI identified on the baseline electrocardiogram, which was characterised by the presence of a major Q-wave or a minor Q-wave with ischaemic ST-T changes.
Statistics
We considered three consecutive study periods: 1995-1997 (Period I), 1998-2002 (Period II) and 2003-2006 (Period III), rendering approximately equal numbers of patients per study period. The time period refers to the starting date of the study. We respected the time periods used in the EUROASPIRE program.6
Analyses were done applying the method of Generalised Estimated Equations (GEE) with a Poisson distribution, a logarithmic link, modelling the study period either as factor or as a covariate.11 By taking the study level as a random factor, using patients as replicates, nested within the study we acknowledge patients within a study form a more homogeneous group than between studies. This model also allowed to accommodate for “ignorable” missing data.12 An exchangeable working correlation matrix was used to apply the GEE methodology. For the purpose of this analysis baseline values from stent investigations, recorded in the database, were grouped into higher level terms. In the case that a patient scored positively on one of the lower level terms, he or she became member of the higher level term, otherwise the existence of one variable that showed that the patient did not belong to the higher level term was sufficient to exclude him/her from membership, even in the presence of missing data on other lower level terms. This strategy was used to minimise the loss of data, however, this may have led to some underestimation when calculating the prevalence percentages of these high level terms (e.g., statins and fibrates were grouped into the class of lipid lowering drugs). Patients were classified into using lipid lowering drugs when they reported using at least one of the drugs. In the case that there was no information at all about any drug in this class they were classified as missing, in all other cases they were classified as using no lipid lowering drug at all. This strategy was used for all grouped variables.
With this approach, the estimated regression coefficients were identical to those obtained using ordinary logistic regression, but the standard errors were adjusted to account for the clustered data structure. All tests were 2-sided, p-values were not used to reject null hypotheses, and they are only shown to inform the reader on the probability level of a given outcome.
Results are summarised as relative risks for study periods 1998-2002 (RR1) and 2003-2006 (RR2) both with respect to the 1995-1997 period. Trends are calculated by using the time period as a covariate into the GEE model.
Statistical analyses and graphics were produced with assistance of a commercially available statistical software package (SAS version 8.2; SAS, Cary, NC, USA)
Role of the funding source
The sponsors of the individual trials had no role in this study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
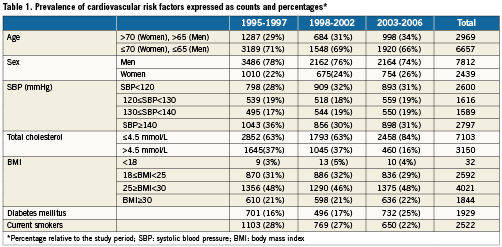
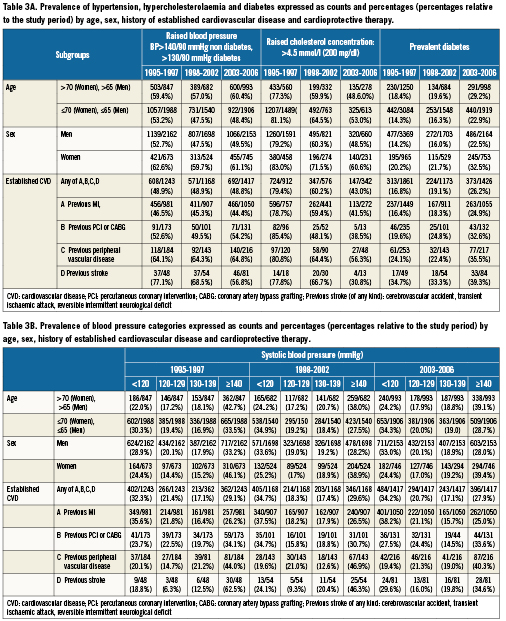
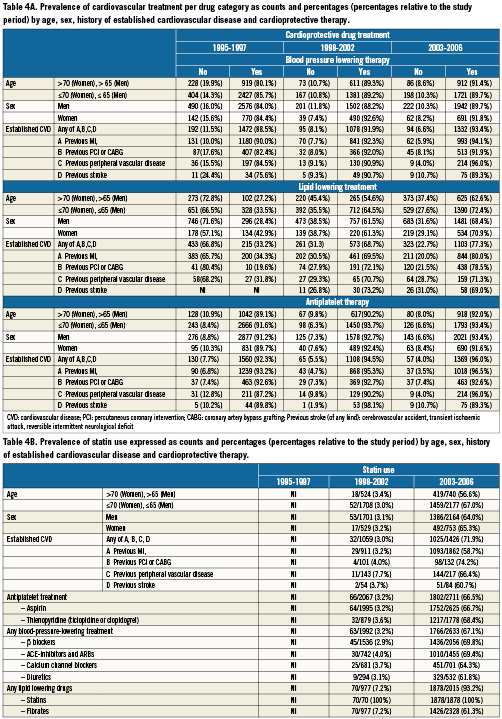
Between February 1995 and 2006, 10,253 patients (male: 76%) were pooled from 32 coronary stent trials in patients with obstructive CAD. The mean age of patients included in the analysis was respectively 60.1, 60.6 and 62.0 years for time Periods I, II, and III (Table 1). Tables 2-4 show the frequency and distribution of the modifiable CV-risk factors over the study periods in relation to patient age, gender, medical history of CV disease, and treatment. Relative changes between consecutive time periods, taking Period I as a reference, are expressed as relative risks, and are shown in Table 5, together with trends over the 12 year study period.
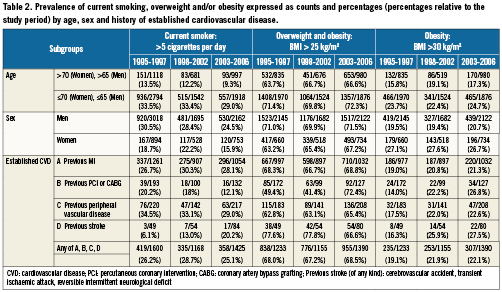
Overall the proportion current smokers did not differ between time periods (p trend: 0.45), not even in the subgroup of patients with known CVD (p trend: 0.43) Tables 2 and 5. There was a decrease in male smokers over time which was consistent in all age categories, however this trend was offset by an increase in the proportion of women smokers aged less than 50 years (Figure 1).
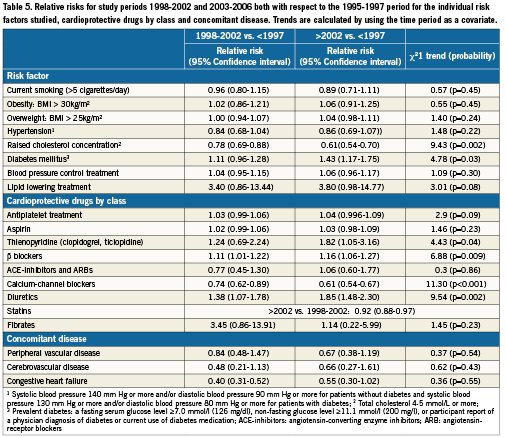
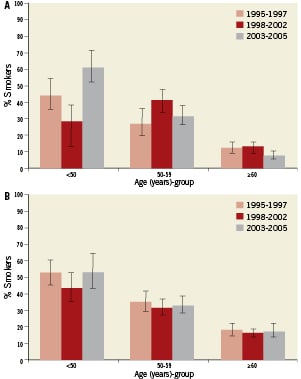
Figure 1. A) Percentage current female smokers and 95% confidence interval by age and study period; B) Percentage current male smokers and 95% confidence interval by age and study period.
Mean body weight respectively was 78.3, 78.8, and 78.7 kilogram for periods I, II and III. The overall proportion of obese and overweight patients did not show a trend over time, not even in the patient group with history of CV disease (Table 5). There was a possible increase however, in the proportion of overweight women (p trend: 0.15), whilst the proportion of obese women remained much the same (Table 2). The proportion of obese women was higher than obese men throughout the study period.
Only three fifth of patients in all three periods had their BP below target levels (respectively: 55%, 50%, 53%), and most compelling this occurred in only half of the patients with established CVD (respectively: 51%, 52%., 51%; p trend: 0.56 ) Table 3, 3B, Appendix 2, and Table 5. Of those patients taking BP lowering drugs, although not necessarily taken as anti-hypertensive treatment, the proportion that achieved the SBP target of <140/90 mm Hg (<130/80 mm Hg in patients with diabetes) did not differ over time (period I: 47%, period II:49%, period III: 47%; p=0.53; Tables 3 and 5). The proportion of hypertensive patients not taking blood-pressure-lowering treatment declined over time (respectively: 19%, 10%, 9.0%%; p=0.21). Overall, the proportion of patients with a raised total blood cholesterol concentration decreased over the three time periods (p trend: 0.002) Tables 3 and 5, with a similar trend observed in the subgroup of patients with established CVD (p trend: <0.001). Although the proportion of patients taking lipid-lowering drugs (statins, fibrates) who achieved the cholesterol target of <4.5 mmol/L, was twice as high in period III than in Period I (Tables 3 and 5), only 48% of patients receiving treatment in Period III achieved the target for optimal cholesterol control, a trend consistent with the increase in statin use (Table 4; R.R= 9.7, p:0.02). Of note, statin use was absent, or not specifically asked about in the CRF in Period I, and therefore the relative risk was calculated comparing Period III to II, and consequently no trend could be calculated.
The frequency of prevalent diabetes increased over time (p trend: 0.03) and this increase was more prominent in men than in women (Tables 3 and 5). There was a parallel, proportional increase in the concomitant use of lipid lowering and antihypertensive drugs in these patient groups. In the group of diabetics, the proportion of patients with hypertension increased, whilst those with a cholesterol level >4.5 mmol showed a reverse trend (Figure 2).
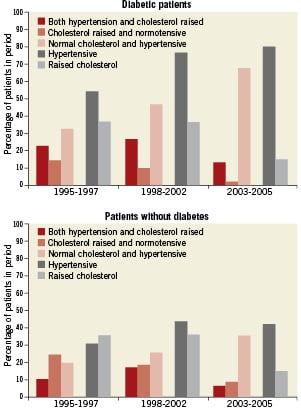
Figure 2. Influence of hypertension and cholesterol in patients with or without diabetes.
The proportion of patients taking either statins, calcium channel blockers, β-blockers, diuretics and antiplatelet treatment increased over time and to the same extent considering age and gender, in secondary and primary prevention (Tables 4 and 5).
Discussion
The lack of improvement in modifiable behavioural risk factors in patients enrolled in stent investigations in Europe between 1995 and 2006 reflects similar evolutions in the general population.6,13-15 Potential patient selection bias, reflecting the specific inclusion and exclusion criteria of the individual studies must be taken into account when putting the current results into perspective. This study emphasises the continuing gap between the standards set in guidelines on CV risk prevention, and the results achieved in clinical practice. Our results are the product of lifestyle, inadequate risk factor management, and the under-use of prophylactic drug therapies, even after the development of a potential life-threatening disease. Overall, these results call for action.
In our analysis the prevalence of smokers was systematically higher than in the corresponding time periods of the EUROASPIRE surveys, however similar trends appeared. Overall, there was a decrease in smoking over time in all age categories, although this trend was partially offset by an increase in the proportion of women smokers younger than 50 years. The high number of smokers in patients with previous symptomatic CV disease is worrisome. Promotion of smoking cessation is important at both a population and individual level, for both primary and secondary prevention.16,17 The magnitude of the increase in CV-risk through smoking is closely, and linearly, related to the number of cigarettes smoked, with even low levels of smoking (e.g., five cigarettes per day) still being associated with an appreciable increased risk of acute MI.18 A physician’s advice to stop smoking is one of the most important first steps in the cessation process, but efforts need to be sustained over time, and more than likely will need to be complemented by pharmacological therapies to counteract nicotine dependence.19,20
The prevalence of obesity, systolic hypertension and to slightly lesser extent diabetes was lower in our analysis as compared to EUROASPIRE and a recent all-comers trial setting.21 Most studies involved in our analysis only included patients with “simple” coronary lesion morphology. Consequently, we potentially excluded from our analysis a patient cohort with high arterial atherosclerotic burden and hence patients with a high prevalence of obesity, hypertension and diabetes.
The frequency of overweight and obese patients included in elective stent studies was slightly lower when compared to the general population for the three time periods considered.6 In EUROASPIRE, but not in our analysis, the distribution of BMI shifted in a skewed fashion such that the proportion of the population with morbid obesity increased by a greater extent than the proportion who were overweight. Still in period III seven out of ten patients had a BMI ≥25 kg/m² and over one fifth were obese. The numbers of patients classified as overweight and/or obese has reached epidemic proportions, despite both being associated with numerous comorbidities. More than 70% of overweight patients were on anti-hypertensive or lipid lowering drugs in our analysis. The maladaptive effects of excessive body weight on various CV-risk factors, together with its adverse effects on CV structure and function, results in its propensity to reduce overall survival.22,23 Weight reduction interventions, beyond bariatric surgery, involves lifestyle choices including dietary intervention and increased physical exercise.24 In a stepwise approach approved prescription medications targeting the various systems that regulate eating behaviour and body weight can be a valid adjunct to behavioural changes. The long-term maintenance of weight reduction is difficult and needs sustained personal and family motivation, and long-term professional support.
The prevalence of diabetes in the current study is less than reported in the real world,6 though there was a possible trend towards an increase in the proportion of diabetics, especially in women (p trend: 0.19) and the elderly (p trend: 0.03) over time.
Also the prevalence of hypertension was relatively low, compared to the corresponding time periods in the EUROASPIRE surveys, and only showed a small time trend towards better blood pressure management in the subgroup of younger patients (p trend: 0.18). Despite the increased number of patients with systolic hypertension taking one or more BP lowering drugs, there was no corresponding improvement in overall BP control. Moreover, the proportion of patients taking one or more anti-hypertensives that lowered their systolic BP within the normal range did not change. This failure to manage BP effectively was higher than reported in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA) at both one and two years follow-up.25 Potential explanations for this are the sub-optimal dosing and titration of medication and/or poor patient compliance. BP lowering is essential for CV disease prevention; in a previous large meta-regression analysis within trial gradients in achieved systolic pressure almost completely accounted for the differences in cardiovascular outcomes, including stroke and MI.26
In contrast with BP, the management of blood lipid concentrations improved substantially, which is largely attributed to the increased use of statins from 1998 onwards. Despite this however, only about half of patients achieved the target cholesterol concentration of below 4.5 mmol/L, set by the 2003 joint European societies guidelines on CV disease prevention.27 Lipid control in patients taking lipid lowering drugs has improved, however, reaching the 2007 total cholesterol target of 4.0 mmol/L or less may prove to be an important challenge for patients and physicians.28 Systematic reviews indicate that a reduction of total (and LDL) cholesterol by statins is associated with marked reductions in both fatal and non-fatal CV events.29 In the subgroup of patients with a history of CV disease we noticed a reduction in the portion of patients using concomitant cardioprotective drugs, that remarkably paralleled the trend for those that did not reach the preset cut-off threshold target of total cholesterol (≤4.5 mmol/l) accepted for this analysis. Again, this might be an indication of lack of change in lifestyle, suboptimal prevention or both, in this subgroup of patients.
Even if drug treatment according to guidelines and blood lipid status substantially improved, the attainment of therapeutic targets for BP did not. Again this might, point to the fact that drug treatments alone are not sufficient, and must be combined with a professional lifestyle intervention. The recommendations for lifestyle management remain the foundation of preventive cardiology: to stop smoking, make healthy food choices, and become physically active. Moreover, the evidence for their effectiveness in cardiovascular disease prevention and rehabilitation programmes that address lifestyle is compelling.30 The preset targets as recommended by clinical practice guidelines are not unrealistic. In the Clinical Outcomes Utilising Revascularisation and Aggressive Drug Evaluation (COURAGE) trial, patients had high rates of adherence to the regimen of diet, regular exercise, and smoking cessation.31
An important strength of this analysis is that all baseline data were collected using a standardised CRF in an established network of participating sites across Europe by a single ARO.
The findings of this analysis must be considered within the context of the studies’ limitations. Our study results only apply to patients in the need for PCI for symptomatic CAD, extrapolations to the general populations may not be valid. A selection bias towards the sickest patients, not receiving effective CV prevention cannot be excluded. Patients included in stent investigations were recruited in specialist cardiac centres and may not be a representative sample of all patients with CV disease requiring PCI and stenting in Europe. The reality of preventive therapy and lifestyle changes in non-specialist centres may be considerably different. Our analysis included only those aged 25-84 year because of the limited data available in older patient groups. Moreover, elderly patients and women have been shown to be under-represented in many clinical trials and surveys in cardiovascular heart disease.32
Changes in the baseline characteristics of patients who were enrolled in these stent investigations between 1995-2005 most probably reflect the shift in the general patient population. However, we acknowledge the slight variation in individual inclusion and exclusion criteria among studies which may have had an impact on the results. On the other hand, our statistical analysis allows correction for a relatively large variation of some items between studies within (a) study period(s) with respect to the observed trend over time.
Conclusion
Patients requiring PCI are an important target population in whom lifestyle changes and aggressive secondary preventative measures should be aimed. PCI should open the door towards optimising secondary prevention.
Conflict of interest statement
G.E. Van Es and D. Goedhart are employees of Cardialysis. All other members of the analysis and writing committee have no conflict of interest to declare.