Abstract
Aims: The reported rate of stent thrombosis (ST) after drug-eluting stent (DES) implantation varies among registries. To investigate differences in baseline characteristics and clinical outcome in European and Japanese all-comers registries, we performed a pooled analysis of patient-level data.
Methods and results: The j-Cypher registry (JC) is a multicentre observational study conducted in Japan, including 12,824 patients undergoing SES implantation. From the Bern-Rotterdam registry (BR) enrolled at two academic hospitals in Switzerland and the Netherlands, 3,823 patients with SES were included in the current analysis. Patients in BR were younger, more frequently smokers and presented more frequently with ST-elevation myocardial infarction (MI). Conversely, JC patients more frequently had diabetes and hypertension. At five years, the definite ST rate was significantly lower in JC than BR (JC 1.6% vs. BR 3.3%, p<0.001), while the unadjusted mortality tended to be lower in BR than in JC (BR 13.2% vs. JC 14.4%, log-rank p=0.052). After adjustment, the j-Cypher registry was associated with a significantly lower risk of all-cause mortality (HR 0.56, 95% CI: 0.49-0.64) as well as definite stent thrombosis (HR 0.46, 95% CI: 0.35-0.61).
Conclusions: The baseline characteristics of the two large registries were different. After statistical adjustment, JC was associated with lower mortality and ST.
Introduction
Early, late and very late stent thrombosis (ST) remains a safety concern with durable polymer-based drug-eluting stents (DES). Late or very late ST is a rare but devastating event that has significant morbidity and mortality: 10% to 30% of patients with definite ST do not survive, whereas a proportion will experience an unexpected out-of-hospital death1-6.
The initial anecdotal ST occurring in the months and years after implantation of a DES was reported from Europe7, where the sirolimus-eluting stent was available on the market earlier than in other regions of the world. Subsequently, a registry from Bern and Rotterdam reported a stent thrombosis rate of 1.6% at one year, with a steady increase of very late stent thrombosis at 0.6% per year without abatement over a follow-up period of four years2,3. These numbers were largely confirmed by the follow-up of the Arterial Revascularisation Therapies Study Part II, showing a definite ST rate of 1.5% at 12 months, with a similar annual increase of definite very late ST of 0.4% to 0.5% up to five years (3.8% definite stent thrombosis at five years), in a population with a majority of three-vessel treatment and with an average stented length of 73 mm8,9. The other European registries, such as SCAAR (Swedish Angiography and Angioplasty Registry) (n=21,717), and the Pinto Slottow et al registry (n=8,000), have all indicated that the risk of very late ST persists at an annual rate of between 0.36% and 0.6% per year to at least five years after implantation.
On the other hand, Asian registries have consistently reported somewhat lower incidences of stent thrombosis. A nationwide post-marketing Japanese registry, including 10,778 patients exclusively treated with the CYPHER® stent (Cordis, Johnson & Johnson, Warren, NJ, USA), showed a one-year definite ST rate of 0.61% with a 0.2% per year increase of very late ST10. In large trials from Korea in 2,701 patients, with or without long-term dual antiplatelet therapy, the definite stent thrombosis rate was 0.2% at one year, and increased up to 0.4% at two years11.
These observed differences raise the following questions which have not been addressed as yet: I) Are there real geographical differences between Europe and the Far East in baseline characteristics and clinical outcomes in patients undergoing PCI? II) If so, what are the factors contributing to the differential clinical outcomes? To elucidate these points, we performed a pooled analysis of patient-level data of two large all-comers registries from Europe (Bern-Rotterdam registry: BR), and Japan (j-Cypher: JC).
Methods
STUDY DESIGN AND PATIENT POPULATION
Detailed descriptions of the two large registries are described elsewhere3,10. Briefly, between April 16, 2002, and December 31, 2005, the Bern-Rotterdam registry (BR) included 8,146 consecutive patients undergoing PCI with either sirolimus-eluting stent (SES; n=3,823) implantation or paclitaxel-eluting stent (PES; n=4,323) implantation at two academic hospitals in Switzerland and The Netherlands. The j-Cypher registry (JC) was a multicentre observational study conducted in Japan. From August 2004 to November 2006, 37 centres included 12,824 consecutive patients undergoing SES implantation with or without other types of stents, 12,812 patients receiving at least a sirolimus-eluting stent. Both registries had a similar design and were all-comers trials without any exclusion criteria according to clinical presentation. Since the incidence of stent thrombosis was related to the type of DES3, patients treated with a paclitaxel stent were excluded from the current analysis. As a result, the analysis included 16,635 patients treated with SES (BR: n=3,823, JC: n=12,812).
The principal investigators of the Bern-Rotterdam registry and the j-Cypher registry were contacted, and individual patient data were requested on a broad range of baseline characteristics, medication usage and clinical outcome up to five years. Clinical outcome included data on all-cause death and definite stent thrombosis at five years. The patient-level based data were subsequently managed, analysed and interpreted by two researchers (Y. Onuma, P.W. Serruys).
DEFINITIONS AND CLINICAL ENDPOINTS
In both registries, stent thrombosis was adjudicated according to the ARC definitions12. Definite stent thrombosis was defined as angiographically defined thrombosis with TIMI grade 0 or 1 flow or the presence of a flow-limiting thrombus, accompanied by acute symptoms, irrespective of whether there had been an intercurrent reintervention13. The major endpoints were all-cause death and definite stent thrombosis according to the ARC definitions. Since the definition of MI was different in two registries, this was excluded from the analysis. No attempt was made to re-adjudicate the events in the different trials to compensate for the differences in the individual endpoint definitions.
Risk factors and comorbidities in each patient were determined as classified by the treating physicians. Acute coronary syndrome was defined as the group of clinical symptoms, electrocardiographic changes, and elevation of cardiac biomarkers which are compatible with acute myocardial ischaemia and encompass an acute myocardial infarction (ST-segment elevation and non-ST-segment elevation myocardial infarction) as well as unstable angina14. Hypertension was defined as blood pressure of 140 mmHg or greater systolic, or 90 mmHg or greater diastolic, or current use of antihypertensive treatment. Dyslipidaemia was classified as a concentration of cholesterol in serum of 6.2 mmol/L or greater, or the use of lipid-lowering drugs, according to the historical guidelines prevailing at the time of the enrolment of the patients3.
STATISTICAL ANALYSIS
Summary statistics for all continuous variables are presented as mean±standard deviation, whereas categorical variables are expressed as percentages. Comparisons among groups were performed by independent t-test for continuous variables and Pearson’s chi-square test for categorical variables. All statistical tests were two-tailed and a p-value of <0.05 was considered as statistically significant. The incidence of events over time was studied with the use of the Kaplan-Meier method, whilst log-rank tests were applied to evaluate differences between the treatment groups. Patients lost to follow-up were considered at risk until the date of last contact, at which point they were censored. Landmark analysis was performed according to a pre-specified landmark point at one year and cumulative incidence rates were estimated separately for events up to one year and beyond.
To elucidate the difference of the two registries, separate Cox regression models were built to adjust for multiple potential confounders in the baseline characteristics. Type of registry was forced into forward stepwise models using the following parameters listed in Table 1 with entry and stay criteria of 0.05 and 0.10, respectively: age, gender, current smoking, hypercholesterolaemia, diabetes, presentation with STEMI, cardiogenic shock, body mass index, number of stents used, average stent diameter, treatment of right coronary artery, left anterior descending artery, left circumflex artery, saphenous vein or arterial graft, IVUS usage during the procedure, aspirin usage at discharge, thienopyridine usage at discharge, statin usage at discharge, beta-blocker usage at discharge, ACE-inhibitor usage at discharge. The type of registry was coded as 1 for the j-Cypher registry and 0 for the Bern-Rotterdam registry. The results are presented as adjusted hazard ratios (HR) with 95% confidence intervals (CI). The same analyses were performed in each subgroup. All statistical analyses were performed with SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). The authors had full access to and take full responsibility for the integrity of the data.
Results
BASELINE CHARACTERISTICS
Baseline demographics of the two all-comers populations were significantly different. As summarised in Table 1, patients in the JC registry were older, more frequently diabetic and hypertensive. Patients in the BR registry had a larger BMI, more frequently were smokers and had hyperlipidaemia, and presented more frequently with STEMI or acute coronary syndrome compared to those in the JC registry. The treated vessel was significantly different. The total stented segment was significantly longer in the JC registry than in the BR registry. IVUS use was 47.5% in the JC registry, while it was 3.5% in the BR registry.
Medication at discharge was also different. Aspirin use was higher in the JC than in the BR, while the use of any thienopyridine was higher in the BR registry than in the JC registry. The most frequently prescribed thienopyridine was ticlopidine in the JC, while it was clopidogrel in the BR. The planned duration of thienopyridine prescription was significantly longer in the JC (713±778 days) than in the BR (94.7±109 days, p<0.001). The actual duration of thienopyridine was 805±706 days in the JC registry.
CLINICAL OUTCOMES UP TO FIVE YEARS
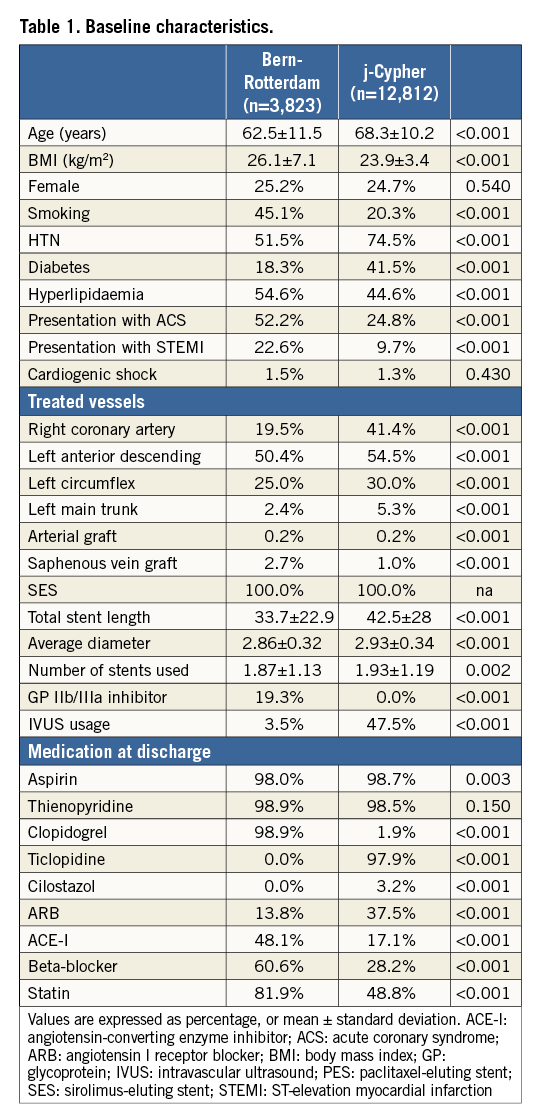
The Kaplan-Meier estimates of cumulative incidences of five-year clinical endpoints are presented in Figure 1A. In early time points after the index procedure, the crude all-cause mortality rate was lower in the JC than in the BR (at 30 days, JC: 0.2% vs. BR: 2.1%), while the long-term mortality at five years tended to be lower in the BR than in the JC (BR: 13.2% vs. JC: 14.4%, log-rank p=0.052). The incidence density of ARC definite stent thrombosis was 0.2 per 100 person-years in the JC and 0.7 per 100 person-years in the BR. The five-year incidence rate of ARC definite ST was lower in the JC (1.6%) than in the BR (3.3%, log-rank p<0.001), while the two Kaplan-Meier curves separated immediately after the procedure (at 30 days, JC: 0.4% vs. BR: 1.0%) (Figure 1B). In the landmark analysis after one year (Figure 1C), very late stent thrombosis was more frequently observed in the BR than in the JC (BR: 2.1% vs. JC: 1.1%, p<0.001).
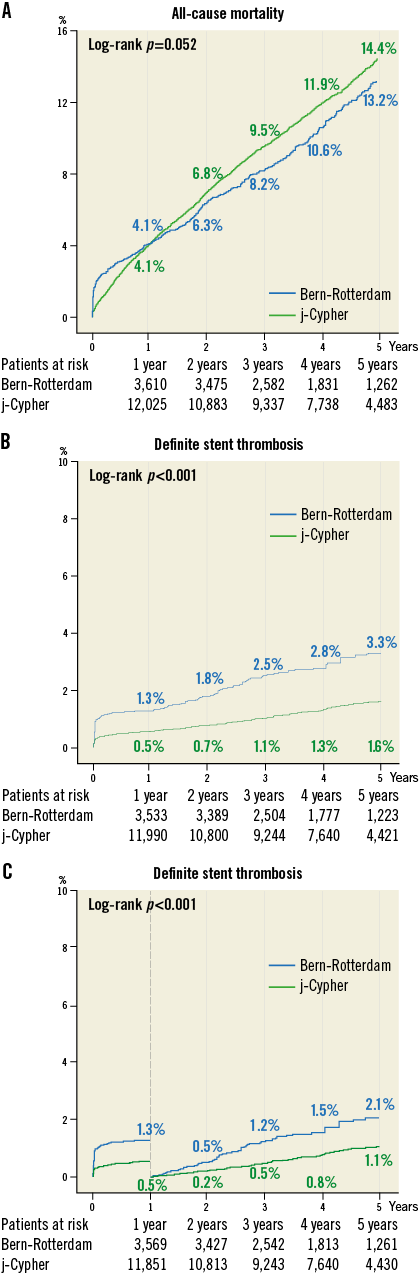
Figure 1. Kaplan-Meier curves. A) Unadjusted Kaplan-Meier event estimates of all-cause mortality. B) The cumulative incidence of definite stent thrombosis up to five years. C) The cumulative incidence of definite stent thrombosis up to five years with a landmark beyond one year (365 days).
COX REGRESSION ANALYSIS
The results of Cox regression analysis are presented in Table 2. After adjustment, the j-Cypher registry was associated with a significantly lower risk of all-cause mortality compared to the BR registry (HR 0.56, 95% CI: 0.49-0.64). The lower mortality in the j-Cypher registry was persistent across the different subgroups, as shown in Figure 2. Similarly, j-Cypher patients were associated with a lower adjusted risk for definite stent thrombosis than the BR registry (HR 0.46, 95% CI: 0.35-0.61). This lower risk of the JC was persistent across the subgroups (Figure 3).
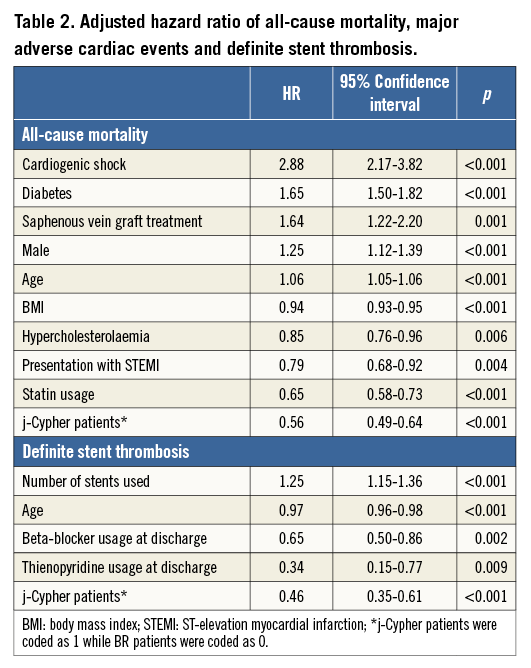
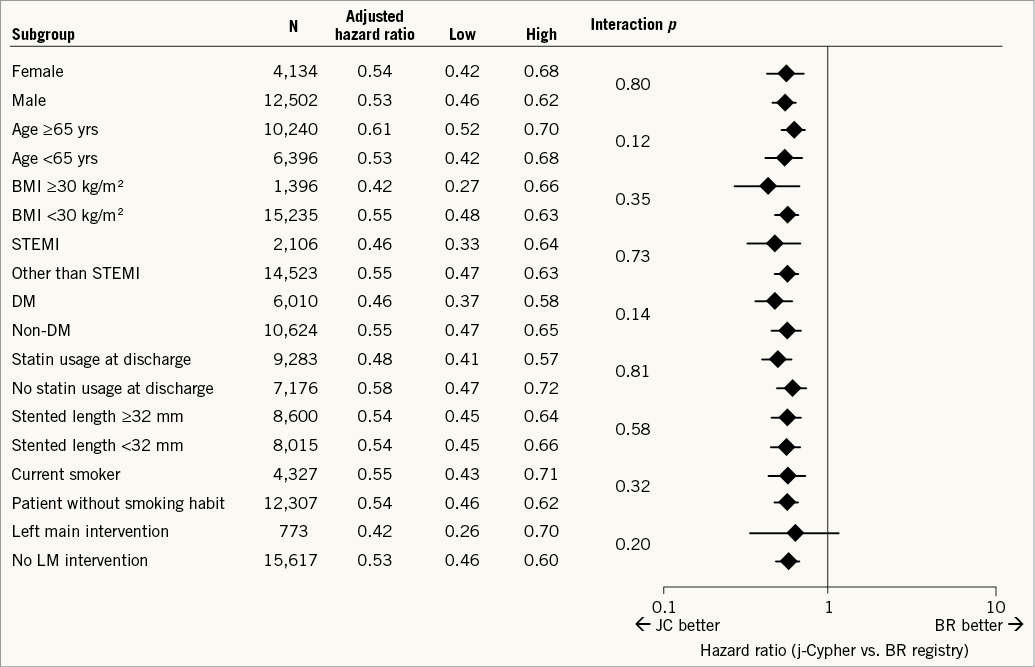
Figure 2. Subgroup analysis of all-cause mortality. Cox regression analysis was performed in each subgroup to calculate all-cause mortality risk of the j-Cypher registry over Bern-Rotterdam registry. DM: diabetes mellitus; LM: left main; STEMI: ST-elevation myocardial infarction
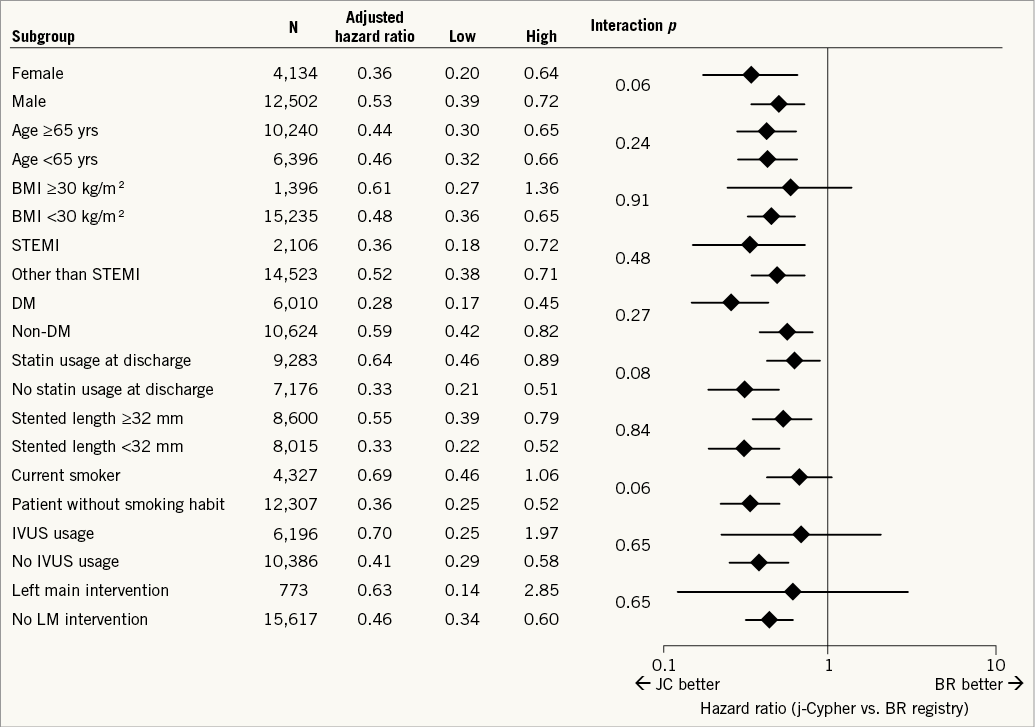
Figure 3. Subgroup analysis of definite stent thrombosis. Cox regression analysis was performed in the subgroup to calculate hazard ratios of definite stent thrombosis between the j-Cypher registry and Bern-Rotterdam registry. DM: diabetes mellitus; LM: left main; STEMI: ST-elevation myocardial infarction
Discussion
The main findings of the current analysis are the following: i) despite the same all-comers inclusion of the two large registries from Europe and Japan, the baseline characteristics were significantly different, reflecting the difference in clinical practice and ethnicity of the two regions; ii) definite stent thrombosis was less frequently observed in the Japanese registry compared to the European registry, while crude mortality tended to be higher in the JC registry than in the BR registry; iii) after statistical adjustment, the j-Cypher registry was associated with lower risks of mortality as well as stent thrombosis compared to the Bern-Rotterdam registry.
DIFFERENCES IN CORONARY RISK FACTORS
The baseline demographics amongst these two registries were completely different. The patients in the Japanese registry were approximately six years older, and were more commonly diabetic (JC: 41.5% vs. BR: 16.2%, p<0.001) but were less obese (BMI: 23.9 vs. 25.1 kg/m2, p<0.001), compared to European patients. These findings were in line with previous studies comparing the risk factors of Japanese patients with the American population, showing the similar difference of baseline characteristics15,16.
PROCEDURAL DIFFERENCES
Our analysis demonstrates the procedural differences between European countries and Japan. For example, glycoprotein IIb/IIIa is not approved for the Japanese market, while IVUS use seems frequent in Japan probably due to the reimbursement system. IVUS use is speculated to be low in European daily clinical practice since this imaging modality is not reimbursed throughout most European countries17,18. The left main trunk was more frequently treated in the Japanese registry than in the European registry. This might reflect the fact that in Japan PCI was performed more frequently than CABG in patients with complex coronary artery diseases, although the Japanese guidelines regard a PCI to the unprotected left main in elective cases as class III19. Kohsaka et al reported that the proportion of PCI among first coronary revascularisation procedures in a Japanese multicentre CREDO-Kyoto PCI/CABG registry was approximately 80% and 50% in two-vessel and three-vessel diseases, respectively16.
POST-PROCEDURAL DIFFERENCES
Medication after the index procedure was also significantly different. At the time of the JC enrolment (2004-2006), clopidogrel was not reimbursed for usage after stenting in the Japanese market and therefore 97.9% of patients received ticlopidine. In patients with an adverse effect due to thienopyridine, it was common that Japanese physicians prescribed cilostazol20. On the other hand, beta-blockers and statins are more frequently used in Europe than in Japan.
DIFFERENCE IN MORTALITY
A higher adjusted mortality risk was observed in the European population when compared to the Japanese population in the current analysis. Although this is in line with the previous literature comparing survival after PCI or CABG in Japan than in the USA15,16, the reasons for these differences remain unclear. Previously, the MONICA project showed a lower mortality from coronary heart disease in the Chinese population21. Kronmal et al showed that the presence and progression of coronary atherosclerosis was more prevalent with white ethnicity compared to the black, Hispanic and Chinese populations. In general, the two BR European countries have a relatively high rate of foreigners (including people from Asia): 19.1% of the Dutch population has a foreign background22, while in Switzerland approximately 20% of the population were foreigners23. On the other hand, only 1.74% of the Japanese population have a foreign background, mainly from China and Korea (Ministry of Justice). However, the potential impact of ethnicity on mortality remains speculative since our registries do not have information on ethnicity.
DIFFERENCE IN DEFINITE STENT THROMBOSIS
Our analysis demonstrates that the Japanese registry was associated with a lower risk of definite stent thrombosis than the European registry, even after adjustment of clinical factors such as presentation with STEMI. The difference appears early after the index procedure and remains until very late. The early difference might relate to the procedural difference, while IVUS usage was not a significant independent predictor of stent thrombosis. In the current registries, however, no data were available as to whether IVUS was used for guidance to optimise the procedural results or solely for documentation. As a post-procedural factor, the difference in duration of thienopyridine might have influenced the incidence of stent thrombosis. The planned duration of thienopyridine prescription was significantly longer in the JC registry (713±778 days) than in the BR registry (94.7±109 days, p<0.001). On the other hand, the type of thienopyridine was not a significant predictor of definite stent thrombosis.
Limitations
The limitations of our study include the fact that there are important differences between the two registries, such as indication for PCI and indication for DES. However, in the current analysis, the individual patient-level data were merged, which enabled us to perform statistical adjustment to address the difference in the baseline characteristics. In addition, the statistical adjustments were performed only for the variables collected in both registries. There might be hidden confounding factors such as the physicians’ mindset, approaches to diagnosis, procedure, health policies, social and cultural situations. For example, in Japan, the interventional cardiologists frequently follow up the patient in the outpatient clinic, while in European clinical practice the follow-up after procedure is left to the referring general practitioners. The j-Cypher registry was a post-marketing all-comers registry, which was initiated by physicians in Japan. At the time of conducting the registry, SES was the first commercially available drug-eluting stent in the country. The penetration of SES usage at that time was varied due to the availability of the device and the difference in the investigators’ decision. Although the original reports of the two registries included various endpoints such as target vessel revascularisation and myocardial infarction24,25, these endpoints were excluded from the current analysis. Different thresholds of cardiac enzyme were used to adjudicate reinfarction or spontaneous myocardial infarction events in the two registries. In the JC registry, scheduled re-angiography was often performed according to local practice, which could influence the revascularisation rate.
Conclusion
This report highlights the important differences in pre-procedural, procedural and post-procedural characteristics as well as clinical outcomes in the two large cohorts from Europe and Japan. After statistical adjustment, the Japanese registry had a lower risk of stent thrombosis and mortality than the European PCI registry. However, the reasons for the differences remained unclear and speculative.
| Impact on daily practice In the two large all-comer registries of sirolimus-eluting stents from Europe (Bern-Rotterdam [BR] registry) and Japan (j-Cypher [JC] registry), the patient-level data were merged and compared. The JC population was older and more frequently diabetic and hypertensive than the BR registry. IVUS was more frequently used in JC than in BR. The mortality and stent thrombosis rates were significantly lower in JC than in BR even after statistical adjustment. This could be caused by hidden confounding factors (difference in ethnicity, physicians’ mindset, health policies, etc.) but the reasons for the differences remained unclear. Caution should be exercised when comparing the registry data from two geographic territories. |
Guest Editor
This paper was Guest Edited by Adnan Kastrati, MD, Deutsches Herzzentrum, Munich, Germany.
Conflict of interest statement
The authors have no conflicts of interest to declare. The Guest Editor has received advisory board meeting and lecture fees from AstraZeneca, Biotronik, MSD and Biosense Europe.