![]()
Abstract
Sparsely populated and with wide non-urbanised areas, Sweden faces specific challenges in providing publicly financed, high-quality and equal healthcare to all parts of the country. As a result, a decentralised organisation for acute coronary care has been developed with coronary care units and catheterisation laboratories in several small- and medium-sized city areas. In contrast, highly specialised non-emergent interventional procedures are centralised to a few high-volume centres, mainly located at university hospitals in large city areas. Nationwide quality registries with nearly complete coverage facilitate healthcare quality improvement and form a basis for clinical research. In this report, we present an overview of demographics, healthcare organisation, quality registries and procedural data for coronary and structural heart interventions in Sweden over the past six years.
Demographics and organisation
Although relatively small, the population of Sweden is increasing, approaching 10 million in late 2016 and unevenly distributed, with more than 50% located in three large city areas (Stockholm, Gothenburg and Malmö) and almost 90% in the southern half of the country. Together with an ageing population and significant immigration these facts represent major challenges to the Swedish healthcare system. There has been a marked reduction in the incidence of and mortality from myocardial infarction (MI) in Sweden over the past 25 years. However, despite the adoption of new pharmacological and interventional treatment strategies, this trend is not reflected in 30-day and one-year mortality rates in patients treated with primary percutaneous coronary intervention (PCI) for ST-elevation myocardial infarction (STEMI), being unchanged at around 7% and 10%, respectively, over the past 10 years. The explanation is most likely to be found in the increasing mean age of the treated population.
Sweden is divided into 20 county councils/regions responsible for administration of healthcare. The level of local self-government is high, including independent powers of taxation, by which healthcare in Sweden is mainly financed. Catheterisation laboratories are located in 28 hospitals, of which eight have on-site cardiothoracic surgery and all but six with 24h/7d service for primary PCI (Figure 1). Wide areas with low population density and relatively large distances between emergency care centres place high demands not only on hospital-based care, but also on well-developed prehospital organisation, including distribution of fibrinolytic therapy when cathlab transfer time exceeds the guideline-recommended maximum delay for primary PCI.
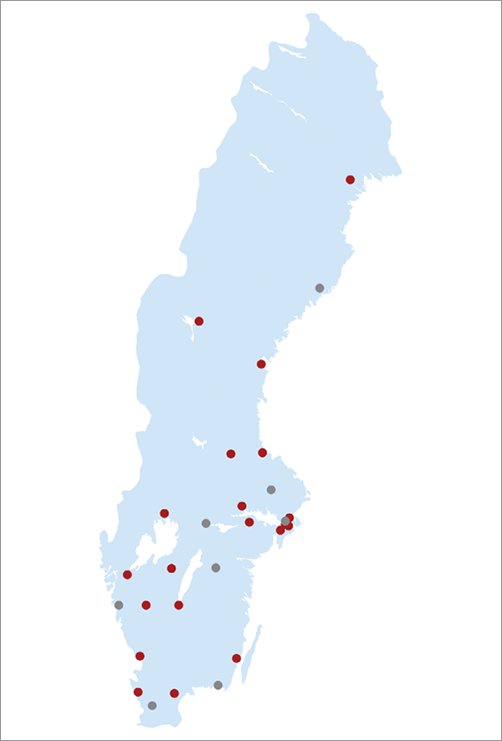
Figure 1. Interventional centres in Sweden with (grey), and without (red) on-site cardiothoracic surgery.
Catheter-based structural heart interventions are performed exclusively at the eight units with cardiac surgery on site. Sweden does not have a central reimbursement system for devices or pharmaceutical agents. Costs for all medical care, including devices, are defined by annual budgets for each department and hospital. Access to treatment is unlimited through public health insurance. The utilisation of cardiac interventional procedures is based on clinical indication and cost without any specific limitations regarding number of devices or procedures.
Launched in 2010, the SWEDEHEART (Swedish Web-system for Enhancement and Development of Evidence-based care in Heart disease Evaluated According to Recommended Therapies) registry, including RIKS-HIA (national registry for acute coronary care), SCAAR (national registry of angiography and angioplasty), Swedish heart surgery registry, SEPHIA (national registry of secondary prevention) and the Swedish Percutaneous Valve Registry, was created with the goal of supporting quality improvement in coronary care and cardiac interventional procedures1. In the registry, data are prospectively collected for all patients undergoing coronary angiography, PCI, heart surgery and percutaneous valve intervention. The registry is web-based with online registration. SWEDEHEART is sponsored by the Swedish health authorities and is independent of commercial funding. The technical platform, OpenQReg, is published as open source software with the possibility to import data from other databases and electronic medical records. SWEDEHEART provides manuals and technical support for users of the registry. The system has error-checking routines automatically alerting the user about out-of-range values, and auto-populating data fields if there is pre-existing information from previous entries. On-site monitoring is carried out on a regular basis, demonstrating a 95% agreement between registry data and medical records. Annual reports presenting key data on an individual centre level are published in both Swedish and English and may be downloaded from the registry website2. In order to facilitate benchmarking and quality improvement, quality indices based on selected registry parameters have been introduced for acute coronary care as well as for interventional procedures. These quality indices are created by setting target levels for a selected number of measures considered particularly indicative of high quality. Parameters used for the SCAAR quality index include (with target levels in brackets): proportion of coronary angiographies with intracoronary pressure measurements in patients with stable coronary artery disease (30%), proportion of PCI performed in the left main coronary artery (LM) where invasive imaging has been used (40%), proportion of patients with NSTEMI where coronary angiography is performed within 24 hours of admission (80%), proportion of PCI performed in patients with acute coronary syndromes where new P2Y12 inhibitors have been used (80%), and proportion of complication registrations after coronary angiography or PCI (99%). The TAVI Quality Index reflects structural factors (presence of a multidisciplinary Heart Team, on-site cardiac surgery facilities), experience (case volume), major complications (major vascular complications, major bleeding, stroke) and risk-adjusted mortality (30-day mortality adjusted for EuroSCORE II).
SWEDEHEART is frequently used for clinical research and there have been an increasing number of scientific publications in international peer-reviewed journals based on data from the registry, counting 58 in 2015. By merging data with the Swedish National Population Registry and the National Patient Registry, clinical endpoint data such as vital status and diagnoses for hospitalised patients can be obtained. Development of separate online randomisation modules has allowed a new clinical trial design, the registry-based randomised clinical trial (RRCT), with both randomisation and follow-up within the registry. The concept was first introduced in the Thrombus Aspiration in ST-Elevation myocardial infarction in Scandinavia (TASTE) trial3, followed by ongoing interventional trials, all with a sample size of several thousand patients4,5.
Similar to other procedural disciplines and many other countries, interventional cardiology training in Sweden traditionally followed a master-apprentice model. Although generally resulting in an appropriate level of technical skills, duration of training and theoretical knowledge may vary considerably. In order to structure and improve the quality of interventional cardiology training in Sweden, our working group developed a two-year training programme aiming to meet international standards. A mission statement was adopted, closely following the principles established by the European Association of Percutaneous Cardiovascular Interventions (EAPCI) and the European Society of Cardiology (ESC). Interventionalists in training follow the structure of the EAPCI/ESC eLearning platform. A two-day evaluation by a highly experienced examiner is followed by certification by the Swedish Society of Cardiology. Interventional fellows can closely monitor their clinical production and performance by dedicated reports in the SWEDEHEART registry.
Coronary interventions
Following a gradual increase during the 1990s and early 2000s, the annual number of coronary angiograms and PCIs in Sweden has levelled off, currently being approximately 40,000 and 21,000, respectively. A shift in the age spectrum is seen with an increasing proportion of interventional procedures performed in the elderly population, balanced by the decreasing incidence of coronary artery disease in younger patients. There is a considerable variation in procedural volume between centres, reflecting both regional differences in population density and comorbidity as well as regional levels of centralisation (Figure 2). The adoption rate of guideline-recommended strategies is generally high, although in some cases exhibiting regional variation. A summary of procedural volumes and temporal trends for some key variables of coronary interventions over the past six years is presented in Table 1. Individual operator procedure volume varies but the average number reaches a level generally accepted for maintenance of quality and skills. Between 2010 and 2015, 194 operators actively reported data in the SCAAR registry and 25 were under training at the beginning of 2015.
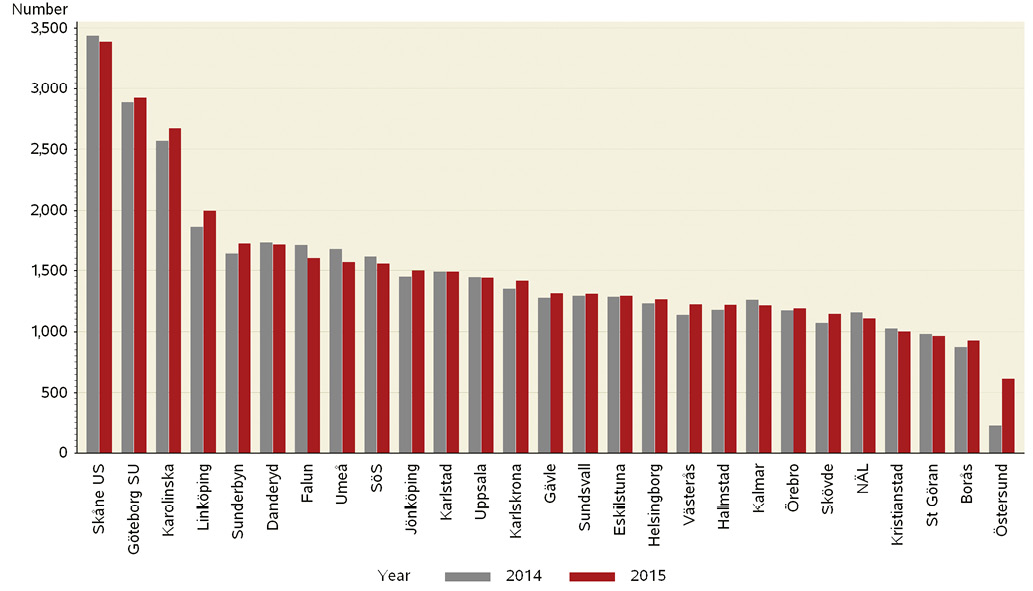
Figure 2. Number of coronary angiographies, per hospital, in Sweden 2014-2015. Adapted from SWEDEHEART Annual report 2015. ISSN: 2000-1843, www.ucr.uu.se/swedeheart/. Adapted with permission from Uppsala Clinical Research Center, Uppsala, Sweden.
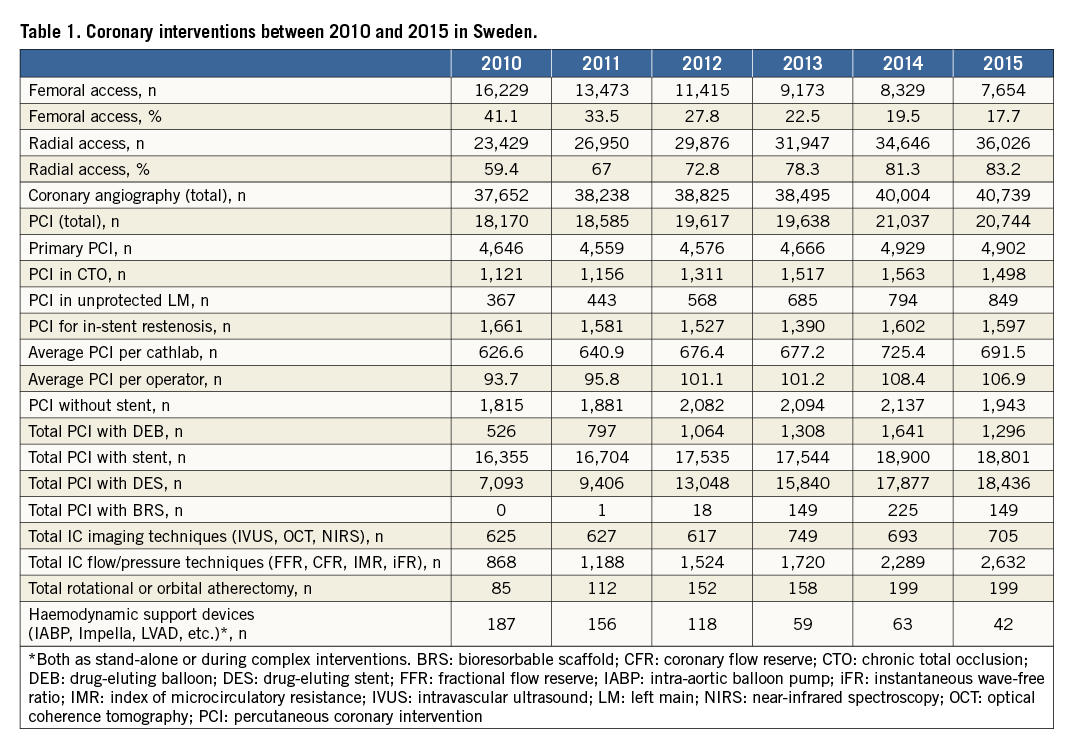
The proportion of procedures performed via radial access is continuously increasing, presently averaging more than 80%, which, together with the adoption of new antithrombotic strategies, may explain a significant reduction of bleeding events seen during the same time period.
Waiting time for elective coronary angiography is relatively short and same-day discharge after PCI has become a routine in most centres. The vast majority of patients hospitalised for myocardial infarction undergo coronary angiography and PCI within guideline-recommended time intervals, both for STEMI and for non-ST-elevation myocardial infarction (NSTEMI). However, due to logistic challenges in hospitals without cathlab resources, revascularisation may be significantly delayed by the need for transfer of patients to invasive centres. The number of primary PCIs for STEMI has been relatively stable, only marginally increasing during the time period.
The use of intracoronary imaging techniques such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT) has been relatively low, with significant between-centre differences even for guideline-recommended use in left main (LM) intervention (ranging from 0% to 60% in 2015). Although subject to similar regional variation, the use of pressure wires has increased continuously over time. As a reflection of the growing evidence supporting the addition of fractional flow reserve (FFR) to coronary angiography, intracoronary pressure measurements are now performed in almost 25% of all patients undergoing coronary angiography for stable CAD in Sweden (range: 5 to 50%).
Stenting is reported in more than 90% of coronary interventional procedures, with the proportion of drug-eluting stents (DES) increasing from 43% in 2010 to more than 98% in 2015. In procedures where stents are not used, drug-eluting balloons (DEB) have become the predominant treatment. For bioresorbable scaffolds (BRS), the adoption rate is low and has levelled off in the absence of strong scientific evidence and guideline recommendations.
The frequency of chronic total occlusion (CTO) PCI has increased following the development of dedicated programmes in a few high-volume centres.
Parallel to the historical increase in the use of PCI, the number of patients referred for coronary artery bypass graft surgery (CABG) has declined. Notably, there is a relatively large difference between centres regarding the adherence to class 1 guideline recommendations for CABG in preference to PCI (e.g., the combination of diabetes mellitus and complex multivessel disease in patients with stable angina). Similar regional differences in treatment strategy also apply for patients with unprotected left main disease with a variation from 20% to more than 90% for CABG as the primary decision following coronary angiography. These referral patterns probably reflect both local traditions and logistic factors such as the presence or absence of on-site surgery, distance to surgical centres and regional differences in waiting time for surgery.
Complication rates are generally low with self-reported periprocedural complications at the level of 0.1-0.6% for individual components such as arrhythmias, perforations, haemodynamic and neurological complications. The most common complication is bleeding with an overall frequency of 2.8%. Registration of complications after coronary angiography is completed in 99.9% of patients within the SCAAR registry.
Structural heart interventions
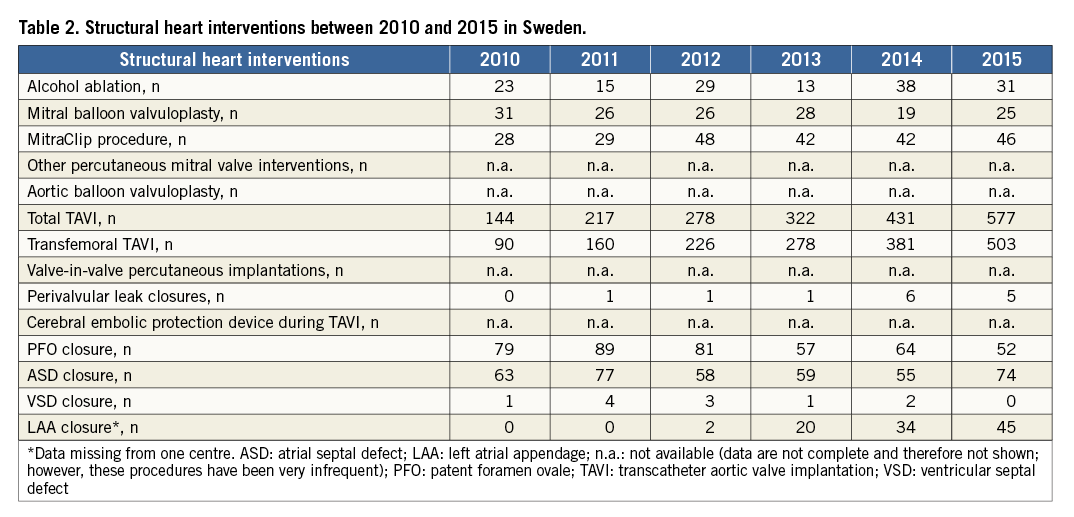
The most common structural heart intervention is TAVI, with 577 procedures in 2015, an increase of 34% from the previous year. This is equivalent to 57 TAVI procedures per million inhabitants, lower than in some other European countries. One centre had more than 100 procedures, five centres had 50-99 procedures and two centres had fewer than 50 procedures in 2015. The average age of TAVI patients is currently 82 years and the surgical risk score is high (mean logistic EuroSCORE I 21%). Transfemoral TAVI accounts for more than 85% of the procedures since 2013, with two centres reporting 100% transfemoral TAVI in 2015. Thirty-day mortality after TAVI was 2% in 2015, comparable to the surgical results in younger and healthier patients. One-year mortality is still at 15% but is expected to decrease as younger patients will be treated. Procedural volumes for structural heart interventions in Sweden 2010-2015 are presented in Table 2. Left atrial appendage (LAA) occlusion has been performed in low numbers since 2012, although it is expected to increase. The MitraClip procedure is carried out in a few centres at low volumes. In national guidelines, MitraClip has received a low priority because of limited scientific evidence.
Conclusion
In summary, coronary and structural heart interventions in Sweden largely meet international standards, albeit with regional variation in the adoption of guideline-recommended therapies. Benchmarking using quality indices based on data from national registries may help to level out these differences.
Acknowledgements
The authors wish to thank Peter Eriksson, MD, PhD, Ole Kongstad, MD, PhD, Niels-Erik Nielsen, MD, PhD, Jacob Odenstedt, MD, PhD, and Magnus Settergren, MD, PhD, for providing regional centre data on structural heart interventions.
Conflict of interest statement
N. Witt has received research grants from St. Jude Medical. A. Rück has received grants from St. Jude Medical, Medtronic and honoraria from Symetis and Edwards. S. James has received institutional research grants and honoraria from Boston Scientific and Abbott Vascular. S. Koul has received honoraria from AstraZeneca and Bristol-Myers Squibb. B. Lagerqvist has no conflicts of interest to declare.

