Abstract
Aims: Most studies investigating completeness of revascularisation and outcomes for multivessel disease (MVD) patients are limited by small sample size.
Methods and results: We searched PUBMED, Cochrane and EMBASE for studies comparing outcomes of MVD patients with complete revascularisation (CR) vs. incomplete revascularisation (IR) in the stent era. We identified nine studies that met our selection criteria. Compared to IR, patients undergoing CR had significantly lower risk of mortality (relative risk (RR): 0.82; 95% confidence interval (CI): 0.68-0.99; p=0.05), non-fatal myocardial infarction (MI) (RR: 0.67; 95% CI: 0.53-0.84; p <0.01) and subsequent coronary artery bypass graft surgery (CABG) (RR: 0.70; 95% CI: 0.52-0.95; p=0.02) whereas no difference was noted in the incidence of repeat percutaneous coronary intervention (PCI) (RR: 0.87; 95% CI: 0.69-1.11; p=0.28). Average weighted follow up was approximately 29 months for mortality, subsequent CABG and Repeat PCI whereas it was 19 months for non-fatal MI. The results were similar after excluding the only RCT or the one study restricted to diabetics or the study restricted to drug-eluting stent use.
Conclusions: In patients with multivessel coronary disease, complete revascularisation with PCI may be associated with better outcomes than incomplete revascularisation.
Introduction
Percutaneous coronary intervention (PCI), with the use of stents in general and drug eluting stents (DES) in particular, is an important revascularisation option that not only improves angina, but also reduces the need for subsequent revascularisation in patients with stable ischaemic coronary artery disease (CAD)1,2. In patients with multivessel disease (MVD), PCI operators often face a choice between seeking complete revascularisation (CR) of all haemodynamically significant lesions or a selective strategy often termed incomplete revascularisation (IR). As opposed to coronary artery bypass graft surgery (CABG) where CR is more often achieved3, CR with PCI is not attempted in the majority of patients for several reasons including: presence of serious medical conditions, one or more chronic total occlusions (CTO), left ventricular dysfunction or simply because in the opinion of the operator, treatment of selected lesions and vessels is considered adequate for relief of patients symptoms4. Although several randomised and non-randomised studies have compared PCI to CABG and/or medical therapy in MVD5-8, only a few have examined the effect of completeness of revascularisation, often with variable results4,9-16. Some studies have reported better outcomes in patients receiving CR with PCI compared to IR10,14, whereas others have demonstrated no significant differences in outcomes4,13. Therefore choice of CR versus IR with PCI for MVD remains a matter of debate. To our knowledge, there has been no systematic review summarising the literature based on completeness of revascularisation to assist in appropriate decision-making in patients with MVD undergoing PCI. In addition, since most studies investigating the completeness of revascularisation with PCI are individually limited by small sample size to detect differences in mortality and recurrent myocardial infarction (MI)11,15,16, we performed a meta-analysis to evaluate the effect of completeness of revascularisation with PCI on subsequent clinical outcomes.
Methods
We based our methods on the widely accepted (MOOSE checklist) guidelines for reporting meta-analysis of observational studies17.
Search strategy and study selection
We searched PUBMED, Cochrane and EMBASE for studies using the key words “Percutaneous coronary intervention”, “Angioplasty”, “multi-vessel” and “multivessel”, “multi vessel”, “PCI”, “PTCA”, “PCA”, “PCIA”, and “MVD”. We limited our search to studies in human subjects in peer reviewed journals until July 31, 2009 and in addition checked the reference lists of reviewed articles, editorials and original studies identified by the electronic search to find other potentially eligible studies. Two authors (V.A. and M.S.) independently selected the studies to be included in this analysis; discrepancies were resolved by a third reviewer (V.S.S.). The following criteria were used for study selection: 1)study population consisting of subjects with MVD disease not restricted to acute MI. 2)PCI with stents (if indicated) being the revascularisation modality of choice. 3)publication in a peer reviewed journal.
Study quality assessment
Study quality was assessed using the internal validity criteria of the US Preventive Services Task Force18,assigning a rating of “good” when all criteria were met; “fair” when one criterion was not met and “poor” if more than one criterion were not met. The specific criteria for this assessment were: 1)MVD definition based on presence of >50% diameter stenosis in >2 major epicardial vessels; 2)CR defined as no remaining lesion >50% stenosis after PCI; 3)subjects with prior revascularisation were excluded; 4)similar follow-up for both the comparison groups; 5)well defined individual outcomes. All nine selected studies met at least four of the five criteria and were judged to be either good or fair. Differences with regard to study quality or in any of the extracted data were resolved by re-examining the studies with a third observer (V.S.S.) and by consensus.
Data abstraction
Two authors (V.A. and M.S.) independently abstracted data from the selected studies. All reported baseline characteristics were extracted from each of the included studies. Further, we extracted the incidence rates for the following clinical outcomes: all-cause mortality, non-fatal MI, subsequent CABG, repeat PCI in both CR and IR groups as these outcomes were reported by most of the included studies. Appendix1 summarises the definitions for non-fatal MI used by all included studies. Repeat PCI did not include PCI performed as a staged procedure in any of the included studies. When available, adjusted hazard ratio (HR) was also extracted for all the outcomes.
Data synthesis
Treatment effect for each outcome was assessed as a relative risk (RR) with 95% confidence interval (CI). RR was defined as the risk of experiencing the outcome among those achieving CR compared with those achieving IR. Adjusted HR was used to estimate RR when available. The summary RR was estimated using the DerSimonian and Laird method for random effects19. The random-effects model is reported in the text and figures. To assess heterogeneity across studies, we used the Cochran Q statistic based on the pooled RR by Mantel-Haenszel and measured inconsistency (I2; the percentage of total variance across studies attributable to heterogeneity rather than chance) of treatment effects across studies20. Publication bias (i.e., the likelihood of small yet nominally significant studies being selectively published in the literature) was appraised by means of visual inspection of funnel plots21 and using the methods of Egger et al22. All p values were two tailed, and p<0.05 was considered statistically significant. All analyses were performed using STATA software, version 11.0 (STATA, College Station, TX, USA) and Comprehensive Meta-analysis software, version 2 (Biostat, Englewood, NJ, USA).
Results
Search results and study selection
Among the 1,634 studies initially screened, 48 met the criteria for afull text review out of which nine were deemed to be suitable for a study quality assessment. All nine studies were deemed to be either good or fair based on previously mentioned study quality assessment criteria and were included in the meta-analysis (Figure1).
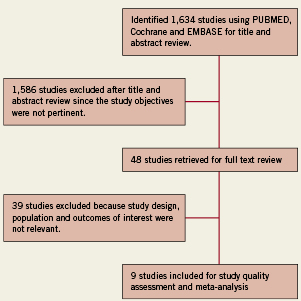
Figure 1. Flowchart of selection of studies for inclusion in the meta-analysis.
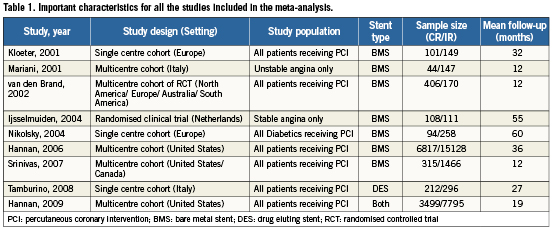
Study and patient characteristics
Important study characteristics are illustrated in the Table1 and baseline patient characteristics for all studies are summarised in Table2. Out of the nine selected studies, one was a randomised clinical trial (RCT)16 and the other eight were observational cohort studies4,9-15. Together, these studies included a total of 37,116 patients with MVD who received either CR (n=11,596) or IR (n=25,520). All included studies defined CR as no remaining lesions >50% in any of the major epicardial vessels. None of them used functional criteria for defining completeness of revascularisation. One study only included patients with diabetes mellitus (DM)12, one restricted itself to DES use14 and one only had patients with unstable angina15. There was no evidence for a publication bias in these analyses (Appendices2-6).
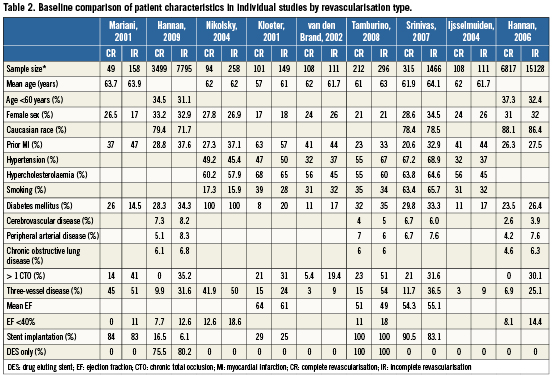
All-cause mortality
Compared to IR, patients undergoing CR had significantly lower risk of mortality (RR: 0.82; 95% CI: 0.68-0.99; p=0.05) during an average (weighted mean) follow up of 29.4 months (Figure2). There was no significant heterogeneity observed across these studies (Q statistic=11.0, p=0.14, I2=36.1%). The results were similar after excluding the only RCT16 (RR 0.82; 95% CI: 0.71-0.95; p<0.01) or when the study restricted to patients with DM alone12 was excluded (RR: 0.85; 95% CI 0.77-0.94; p<0.01).
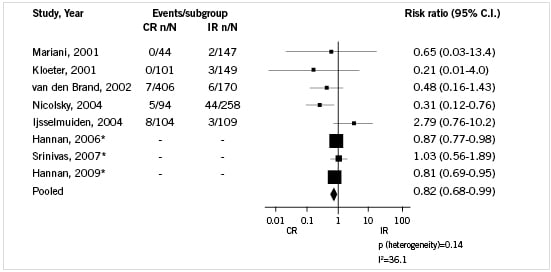
Figure 2. Pooled analysis with risk ratios and related 95% CI’s for the occurrence of all-cause mortality. *Adjusted hazard ratio was used as an estimate of risk ratio. Boxes are the relative risk estimates from each study; the horizontal bars are 95% CI’s. The size of the box is proportional to the weight of the study in the pooled analysis. Diamonds represent pooled random-effect estimates (risk of experiencing the outcome among those achieving CR compared with those achieving IR). The vertical line at 1.0 indicates no effect of completeness of revascularisation on the risk of experiencing the outcome. CR: complete revascularisation; IR: incomplete revascularisation; CI: confidence interval
Non-fatal MI
Compared to IR, patients undergoing CR had significantly lower risk of non-fatal MI (RR: 0.67; 95% CI: 0.53-0.84; p<0.01) during an average (weighted mean) follow-up of 19.8 months (Figure3). There was no significant heterogeneity observed across these studies (Q statistic=6.7, p=0.46, I2=0.0%). The results were similar to the overall results after excluding the only RCT16 (RR: 0.64; 95% CI: 0.50-0.80; p<0.01), when the study restricted to patients with DM alone was excluded12 (RR: 0.71; 95% CI : 0.56-0.91; p<0.01) or when the study restricted to DES use14 was excluded (RR: 0.68; 95% CI : 0.52-0.88; p<0.01).
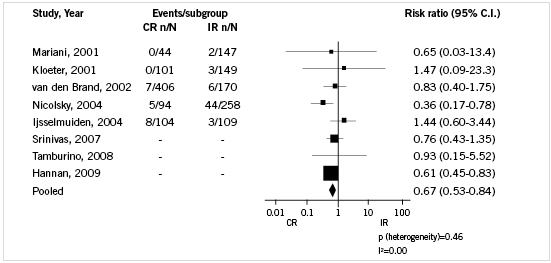
Figure 3. Pooled analysis with risk ratios and related 95% CI for the occurrence of non-fatal MI. Boxes are the relative risk estimates from each study; the horizontal bars are 95% CI’s. The size of the box is proportional to the weight of the study in the pooled analysis. Diamonds represent pooled random-effect estimates (risk of experiencing the outcome among those achieving CR compared with those achieving IR). The vertical line at 1.0 indicates no effect of completeness of revascularisation on the risk of experiencing the outcome. CR: complete revascularisation; IR: incomplete revascularisation; CI: confidence interval; MI: myocardial infarction
Subsequent CABG
Compared to IR, patients undergoing CR had significantly lower risk for undergoing subsequent CABG (RR: 0.70; 95% CI: 0.52-0.95; p=0.02) during an average (weighted mean) follow-up of 29.1 months (Figure4). There was significant heterogeneity observed across these studies (Q statistic=15.7, p=0.03, I2=55.4%). Whereas, excluding the study by van den Brand et al13 eliminated the heterogeneity (Q statistic=3.4, p=0.76, I2=0.0%), the results remained similar for CR vs. IR (RR: 0.86; 95% CI: 0.78-0.95; p<0.01). In sensitivity analysis, the RR was similar to the overall results both after excluding the only RCT16 (RR: 0.68; 95% CI: 0.48-0.95; p=0.03) and on excluding the study restricted to DES use14 was excluded (RR: 95% CI: 0.52-0.98; p=0.04).
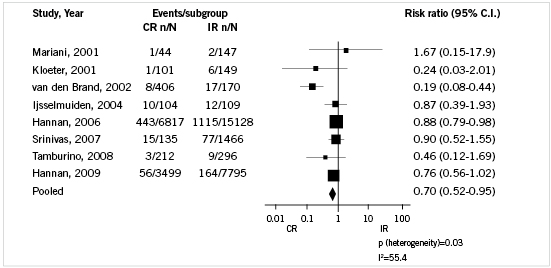
Figure 4. Pooled analysis with risk ratios and related 95% CI for the occurrence of subsequent CABG. Boxes are the relative risk estimates from each study; the horizontal bars are 95% CIs. The size of the box is proportional to the weight of the study in the pooled analysis. Diamonds represent pooled random-effect estimates (risk of experiencing the outcome among those achieving CR compared with those achieving IR). The vertical line at 1.0 indicates no effect of completeness of revascularisation on the risk of experiencing the outcome. CR: complete revascularisation; IR: incomplete revascularisation; CI: confidence interval; CABG: coronary artery bypass graft surgery
Repeat PCI
Repeat PCI rates were similar in both groups (CR and IR) (RR: 0.87; 95% CI: 0.69-1.11; p=0.28) during an average (weighted mean) follow-up of 29.1 months (Figure5). There was significant heterogeneity across these studies (Q statistic=72.6, p<0.01, I2=90.4%). Excluding the van den Brand et al13 and Tamburino et al14 studies eliminated the heterogeneity (Q statistic=10.1, p=0.07, I2=50.5%) but the results were similar to the overall analysis (RR: 1.04; 95% CI: 0.84-1.29; p=0.72). In sensitivity analysis, the RR was similar to the overall results both after excluding the only RCT16 (RR: 0.90; 95% CI: 0.70-1.16; p=0.449) or when the study restricted to DES use14 was excluded (RR: 0.95; 95% CI: 0.74-1.21; p=0.69).
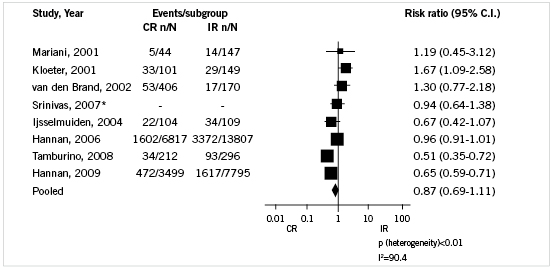
Figure 5. Pooled analysis with risk ratios and related 95% CI for the occurrence of repeat PCI. *Adjusted hazard ratio was used as an estimate of risk ratio. Boxes are the relative risk estimates from each study; the horizontal bars are 95% CI’s. The size of the box is proportional to the weight of the study in the pooled analysis. Diamonds represent pooled random-effect estimates (risk of experiencing the outcome among those achieving CR compared with those achieving IR). The vertical line at 1.0 indicates no effect of completeness of revascularisation on the risk of experiencing the outcome. CR: complete revascularisation; IR: incomplete revascularisation; CI: confidence interval; PCI: percutaneous coronary intervention
Discussion
The results of this meta-analysis clearly demonstrate the lack of well powered randomised studies looking at completeness of revascularisation and long-term outcomes. However, based on existing reports we observed that patients receiving complete revascularisation with PCI experience better clinical outcomes than those receiving incomplete revascularisation. To our knowledge, this is the first report in the literature of pooled analysis of existing evidence that compares complete with incomplete revascularisation.
Multiple surgical series have reported better long-term outcomes for patients receiving CABG with complete revascularisation13,23-25. However, individual studies that compare outcomes for CR versus IR have yielded mixed results with PCI10,12,15,16. Overall, our systematic review included only nine studies comparing IR vs. CR that fulfilled stringent criteria and all except one were either registries or a cohort within a RCT13. The only randomised comparison16 was underpowered to detect a difference in individual outcomes and did not show any difference in outcomes between IR and CR groups. While randomised control trials are desirable, meta-analyses based on observational data are commonly reported in literature, including the coronary revascularisation literature5 and at the moment we only have observational data as a guide to clinical decision making on this issue of completeness of revascularisation with PCI. In our meta-analysis, patients who received CR had a marginally lower risk of death, MI and subsequent CABG compared to patients receiving IR, although the risk of repeat PCI was not significantly different. Anatural question that follows is why patients with CR experience lower risk of death or non-fatal MI. One possible explanation is that CR somehow protects against clinical events. However, an alternative explanation is that patients receiving CR had better clinical risk profile than those receiving IR. In fact, in almost all the studies in this meta-analysis, patients receiving CR had lower incidence of clinical comorbidities, had better ejection fractions, had fewer CTO’s attempted and more often had two-vessel disease rather than three-vessel disease compared to IR patients (Table2). Although we used risk-adjusted point estimates whenever available, residual confounding cannot be entirely discounted. Nonetheless, the observation that CR is associated with a lower incidence of subsequent death and non-fatal MI is novel and bears consideration. Similarly, the effect of CR on reducing the frequency of subsequent CABG is not surprising and has been observed in multiple individual studies4,9-14,16. However, the absence of significant differences in subsequent PCI rates is likely to be related to several possible factors. To begin with, repeat PCI in patients with MVD is a result of either restenosis or plaque progression. Except for two studies10,14, BMS was used predominantly in all the rest, likely resulting in higher need of repeat revascularisation than would have resulted if DES had been used. Furthermore, recent evidence also indicates that a significant proportion of patients with MVD have progression requiring subsequent revascularisation within five years of initial PCI26,27. Therefore, the presence of these competing risks of higher restenosis rates from BMS use and plaque progression possibly resulted in the lack of difference in repeat PCI rates between CR and IR.
The implications of these results are that for patients with MVD, the achievement of CR, whenever possible, ought to be the goal of revascularisation. All studies in this meta-analysis used anatomic criteria to guide revascularisation choice; current evidence suggests that a functional testing strategy may be superior. Although non-invasive stress imaging studies are limited in their ability to accurately localise ischaemia-producing lesions particularly in MVD28, results from the FAME study support the use of physiologic techniques such as fractional flow reserve measurement to ascertain lesions requiring revascularisation29.
Currently there are several effective therapies for patients with MVD including medical therapy, PCI and CABG. Therefore, the current challenge facing practitioners is that of choosing the optimal therapy or combination of therapies to achieve the best possible outcome. Although completeness of revascularisation may not be the primary consideration when determining suitable options, the results of our analysis seems to suggest otherwise. Therefore, practitioners need to carefully consider the optimal modality to achieve complete relief of ischaemia in patients with MVD. For some it may mean the judicious use of DES, whereas in others, for whom CR may not be achievable with PCI, CABG may be an appropriate alternative.
However, these results should be interpreted with some degree of caution and are only hypotheses generating, since the choice of CR versus IR was not random in eight out of nine studies. As a result, the differences in outcome may reflect the underlying differences in clinical characteristics rather than the result of completeness of revascularisation. Albeit, individual studies did compare baseline characteristics and adjusted for confounding wherever indicated and we used adjusted hazard ratios to estimate our pooled estimates whenever reported, nonetheless residual confounding can still be present. This meta-analysis included studies from United States, European and Canadian centres diversifying the patient population, but these results are largely driven by the reports from the New York State PCI reporting system9,10 and the Dynamic registry4 which have their inherent limitations30. Although we used standard meta-analytic techniques for pooled analysis, there were substantial variations in the quality of data based on the outcome variable. As a result, although the tests for heterogeneity were not significant for the pooled analyses of death and MI, significant heterogeneity was observed for subsequent CABG and PCI, limiting the accuracy of the pooled estimate for these latter endpoints. Lastly, since we excluded studies of culprit only versus complete revascularisation in the setting of AMI, the results of this analysis may not be applicable to such clinical scenarios.
In conclusion, the results of our meta-analysis demonstrate the lack of well powered randomised studies comparing clinical outcomes in patients undergoing elective PCI by completeness of revascularisation and suggest that complete revascularisation with PCI is associated with better clinical outcomes than incomplete revascularisation. These results are only hypothesis generating and further investigation with larger randomised controlled trials is warranted to address this issue.
Acknowledgements
We sincerely thank Racheline Habousha, Jennifer Shangkuan and Atul Limaye for their help in study search and selection.
Conflict of interest statement
The authors have no conflict of interest to declare.

