
PLSVC: persistent left superior vena cava
These images describe a rare case of platypnoea-orthodeoxia syndrome caused by a persistent left superior vena cava (PLSVC) draining into the left atrium (LA) (Online Appendix).
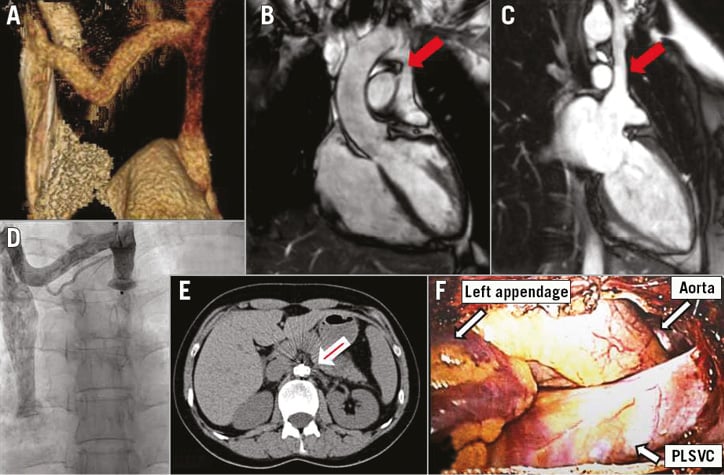
A 39-year-old woman was admitted to our department after hypoxia had been discovered at a preoperative screening for orthognathic surgery. Her oxygen saturation was 99% in the supine position, but dropped to 92% when standing. Thoracic CT scan and MRI revealed an anomalous connection between the innominate vein and the LA; moreover, a vein connecting the PLSVC to the azygos vein was identified (Panel A-Panel C).
Transthoracic echocardiography with venous injection of agitated saline showed immediate appearance of the microbubbles in the LA. No atrial septal defects were recognised. Normal right heart catheterisation was revealed; no oxygen step-up between the caval veins and the pulmonary artery was found. The PLSVC was closed percutaneously through the left internal jugular vein, using a 16 mm AMPLATZER™ Vascular Plug II (St. Jude Medical, St. Paul, MN, USA). Post-procedural venous angiography revealed complete PLSVC sealing (Panel D), and oxygen saturation control revealed no postural differences. The patient exhibited good clinical progress and was discharged home with no symptoms.
After three days, she experienced chest pain and shortness of breath. Orthostatic desaturation of the arterial blood was present again. A CT scan showed that the device had embolised to the abdominal aorta (Panel E). It was removed percutaneously through the right femoral artery, and afterwards the PLSVC was ligated through a left minithoracotomy in the 3rd intercostal space (Panel F). The patient had an uneventful recovery and has remained asymptomatic at twelve-month follow-up.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online Appendix. Platypnoea-orthodeoxia and left superior vena cava
Platypnoea-orthodeoxia syndrome (POS) is a rare clinical phenomenon defined by dyspnoea and arterial deoxygenation induced by orthostatic position and relieved by clinostatic position. Three main mechanisms have been postulated: intracardiac shunting, vascular pulmonary shunting with ventilation/perfusion mismatching, and physiologic pulmonary shunting1.
This report describes a case of POS caused by a persistent left superior vena cava (PLSVC) draining into the left atrium (LA). As the PLSVC drains most frequently into the coronary sinus2, it goes unnoticed, unless a left-sided approach is used for cardiovascular cannulation purposes. Less often, the PLSVC may drain into the left atrium, either directly, or via an unroofed coronary sinus; in this case a right-to-left shunt is expected, with cyanosis and the risk of paradoxical embolisms and cerebral abscesses. This, however, is not always the case, as exemplified by reports of acyanotic patients3. The direction of the shunt depends on the presence and size of connection(s) between the PLSVC and the right superior vena cava, and by the impedance of the right and left ventricles.
That the direction of flow through a PLSVC can vary under changing haemodynamic conditions has already been reported. A right-to-left shunt through a PLSVC that emptied directly into the LA was demonstrated by Chow et al in a 76-year-old man, who presented with cyanosis and heart failure. After diuretic therapy, the shunt was not evident anymore4.
What may have caused the POS associated with an isolated PLSVC in our patient? Bearing in mind that there are three components of mechanical energy that affect intravascular flow, pressure energy, kinetic energy and potential (gravitational) energy5, we hypothesise that, when she changed her position from supine to upright, the addition of gravitational energy to the blood in the PLSVC caused it to flow to the LA.

