Introduction
Percutaneous suture-mediated patent foramen ovale (PFO) closure with the “device-less” NobleStitch system (HeartStitch) has been employed in clinical practice as an effective and safe alternative to traditional device closure123. In previous studies, recurrence of a residual atrial right-to-left shunt (RLS) during follow-up was estimated at almost 20%123. In any case, specific mechanisms of failure have not been systematically described and they still remain unknown. The aim of the study was to describe the mechanisms of failure after NobleStitch from a prospective single-centre cohort.
Methods
Study population
Between June 2016 and September 2021, 122 patients (female 50.0%; mean age 48±12 years) underwent percutaneous suture-mediated PFO closure with NobleStitch at our institution. The overall population was divided into 2 groups on the basis of recurrence of atrial RLS ≤1 or RLS ≥2 grade at echocardiographic follow-up with transcranial doppler (TCD) or transthoracic echocardiography (TTE) bubble study, within 6 months following the procedure. Patients with RLS ≥2 grade were then studied with transoesophageal echocardiography (TOE), in order to define specific mechanisms of ineffective closure. Study design is illustrated in Supplementary Figure 1. Echocardiographic assessment is specified in Supplementary Appendix 1.
Data analyses
Statistical analyses are illustrated in Supplementary Appendix 2.
Results
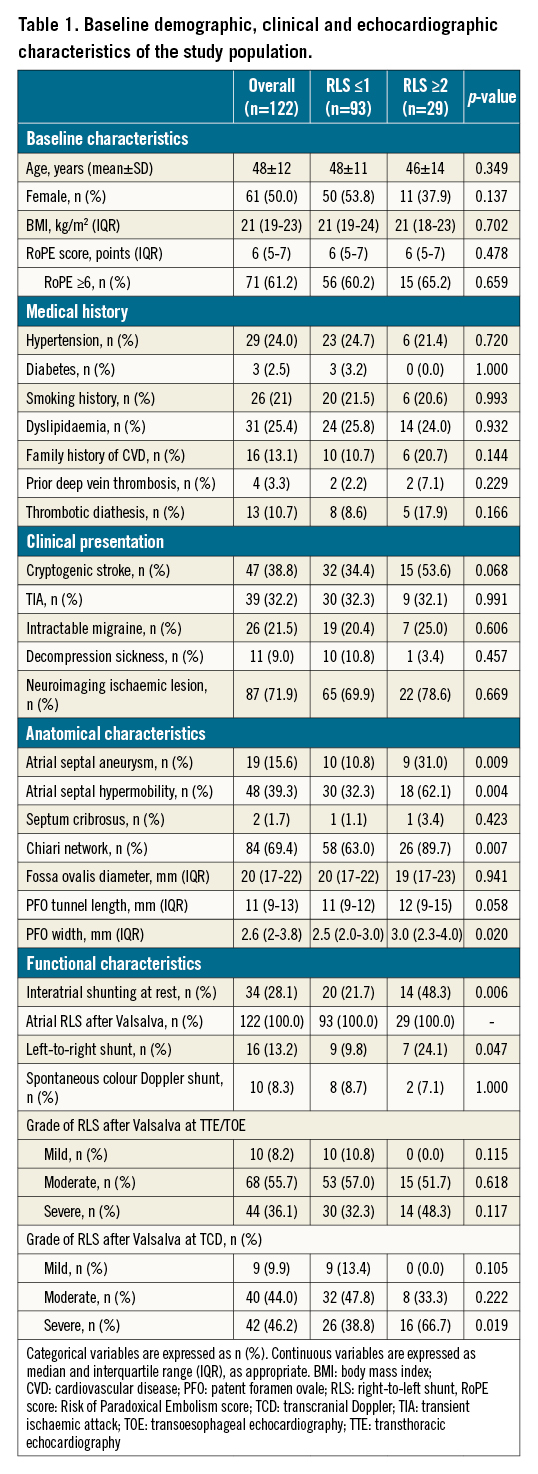
The baseline characteristics of both groups, with and without significant residual RLS, are summarised in Table 1.
The NobleStitch procedure was successfully performed in 116 (95.1%) patients (in 6 patients traditional devices were then used, due to RLS ≥2 at the end of the NobleStitch procedure). Follow-up was complete in 100.0%. At a median follow-up of 335 days, atrial RLS ≥2 occurred in 19.8% (23/116) of patients. Three different mechanisms of late failure (Figure 1, Supplementary Figure 2) were identified by TOE: partial stitch detachment, atrial septal tear and KwiKnot (Heartstitch) embolisation.
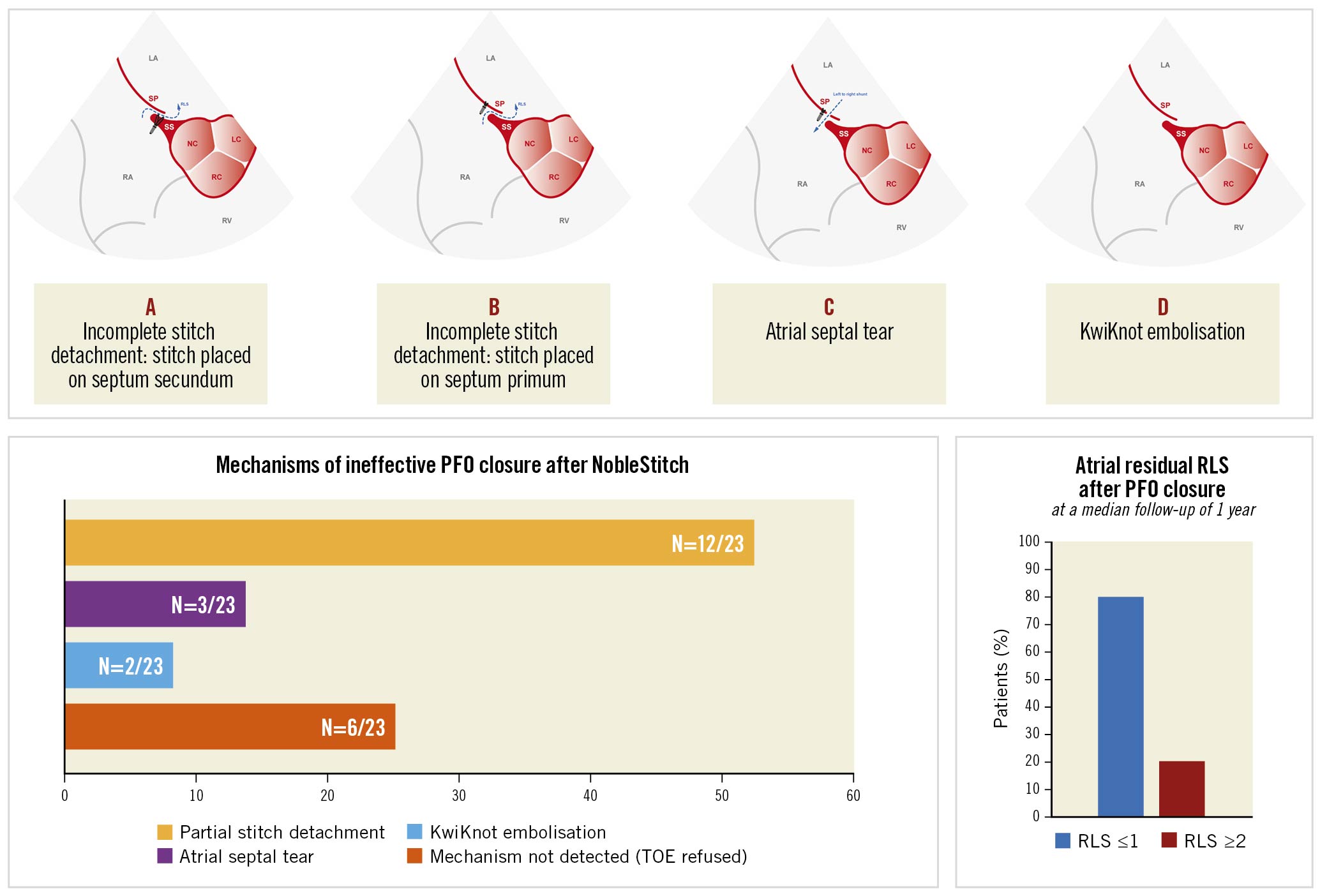
Figure 1. Representative transoesophageal echocardiographic images of different mechanisms of ineffective PFO closure. A. Incomplete stitch detachment: one of the most frequently identified mechanisms of ineffective PFO closure was partial stitch detachment with opening of the foramen ovale and right-to-left passage of microbubbles at bubble test. In this case the stitch is placed only on the septum secundum; B. Incomplete stitch detachment: the same mechanism described in (A) but in this case the NobleStitch was found on the septum primum resulting in recurrent atrial shunt; C. Atrial septal tear: a new atrial septal tear occurred very close to the stitch after the NobleStitch procedure causing a left-to-right shunt; D. KwiKnot embolisation: complete detachment of the stitch and the KwiKnot into the pulmonary circulation resulting in PFO reopening. PFO: patent foramen ovale; RLS: right-to-left shunt; TOE: transoesophageal echocardiography
Discussion
The NobleStitch system is a good alternative for PFO closure when compared to classic device closure, although there is still a lack of information about the long-term follow-up of this procedure and its real effectiveness. In our analysis, the occurrence of effective PFO closure after the NobleStitch procedure - with atrial RLS ≤1 - was 80.2%, which was in line with the rate in previous reports123, although lower than the results obtained with traditional devices4. Although the initial learning curve may have had an impact, specific selection criteria are mandatory in order to improve the outcomes of this procedure.
In this prospective study, we introduced a systematic approach during the follow-up with a bubble test at TTE and TCD on all patients and a further investigation with TOE only in patients with RLS ≥2 to investigate failure mechanisms. After excluding the 6 patients with early technical failure who were managed with a classic device for closure, there remained 116 patients who were successfully treated, of whom 23 (19.8%) presented RLS ≥2. Among them, specific mechanisms of failure were detected in 17 (73.9%). Six patients, all asymptomatic, presented a large residual atrial RLS and refused further TOE. A partial stitch detachment was found as the main mechanism in 52.2% of cases. In these cases, the KwiKnot was attached only on the septum primum or septum secundum, with the clear identification of 2 separated septal sheets, leading to an opening tunnel with consequent atrial RLS. A second mechanism found was an atrial septal tear (13%) occurring really close to the stitch, with consequent atrial RLS. Finally, the third mechanism identified was a complete embolisation of the stitch and the knot into the pulmonary circulation (8.7%). To the best of our knowledge, this is the first study in which partial stitch detachment and KwiKnot embolisation have been identified as possible mechanisms of RLS ≥2, whereas atrial septal tear was previously described in an anecdotal case report5.
Limitations
Different limitations should be considered in the interpretation of our results. This was not a controlled study, so several confounding factors could have influenced our results; secondly, a small sample size from a single centre, with limited follow-up, was included, so our results need to be confirmed in multicentre analyses with longer follow-up. Reflecting real-world clinical practice, an independent core laboratory did not review the echocardiographic data. However, the analyses were conducted by dedicated, highly experienced echocardiographists, utilising validated methods.
Conclusion
Percutaneous closure of PFO by suturing with the NobleStitch system is an effective and safe technique that has obvious advantages over traditional device closure, although recurrence of RLS after PFO closure is not uncommon. Partial stitch detachment, atrial septal tear and KwiKnot embolisation were the main mechanisms encountered during follow-up.
TOE is an essential tool for assessing the anatomical and functional characteristics of PFO, in order to improve patient selection for the NobleStitch procedure, guide the operator in sutureorientation and correct placement, and identify possible mechanisms of failure during follow-up. Defining mechanisms and predictors of failure may help to improve long-term results.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.