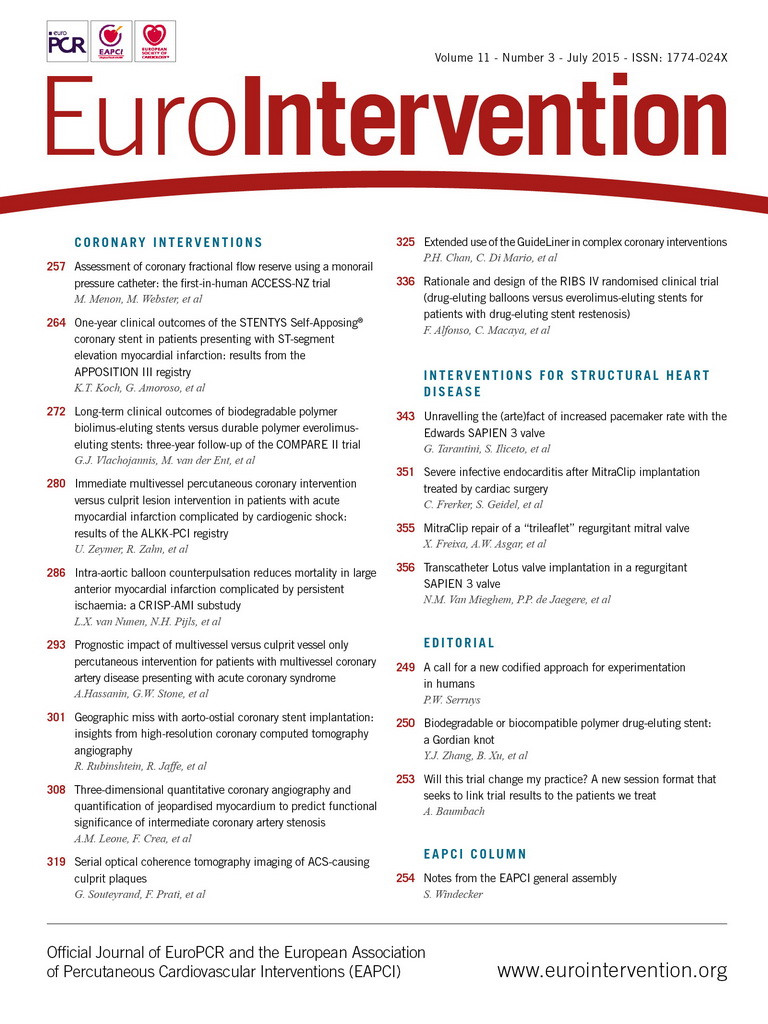
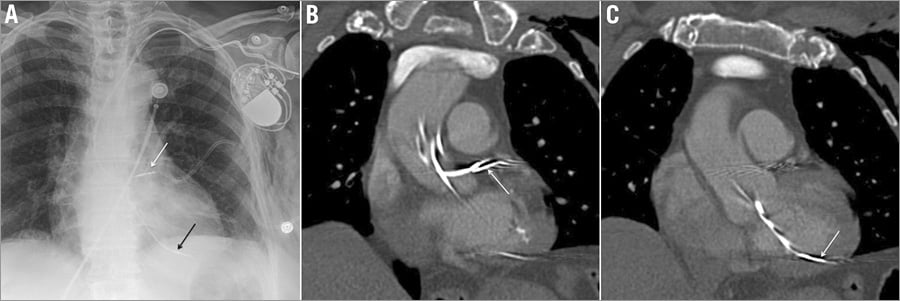
An 80-year-old female was transferred to our institution after undergoing permanent pacemaker implantation complicated by transarterial lead placement. Imaging revealed the misplaced ventricular lead within the left ventricle and the “atrial” lead within the left main coronary artery (Online Figure 1, Moving image 1). The ventricular lead was removed without complication. Angiography and echocardiography confirmed the “atrial” lead at the junction of the left anterior descending and ramus intermedius arteries (Figure 1, Moving image 2). We advanced two guiding catheters loaded with covered stents to the ascending aorta to prepare for possible coronary perforation. After removal of the “atrial” lead, a hazy filling defect was observed within the left main coronary artery which was retrieved using manual thrombectomy (Online Figure 2). The leads were then removed from the left subclavian artery and a covered stent deployed (Moving image 3).
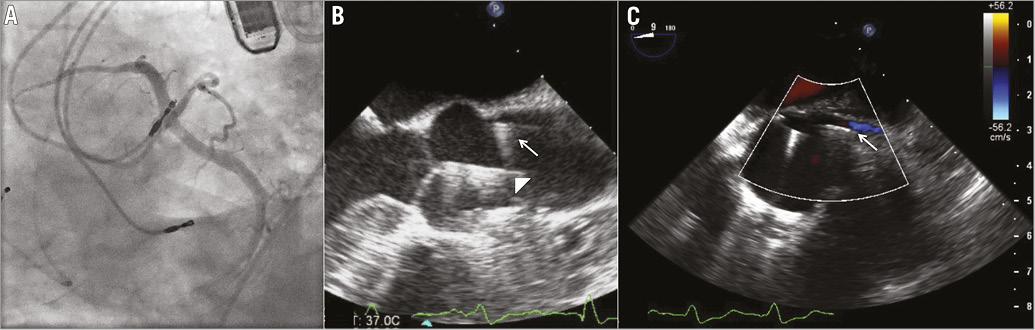
Figure 1. Pacemaker leads within the left ventricle and left main coronary artery. A) Coronary angiography, and B) & C) transoesophageal echocardiography images demonstrating placement of the “atrial” lead within the left coronary system. Echocardiography was performed to monitor for the development of tamponade upon extraction of the lead. Images revealed both leads in the aortic root with one directed towards the left cusp (arrow) and the other crossing through the aortic valve (arrowhead).
Erroneous introduction of a pacing lead into the subclavian artery is a rare complication that in our case was in part due to the use of a micropuncture needle for vascular access. We demonstrate the efficacy of a multidisciplinary team approach by which malpositioned leads were safely explanted from the left ventricle and coronary system without the need for sternotomy and without evidence of myocardial injury.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. Fluoroscopic imaging during temporary right ventricular pacing wire implantation clearly demonstrates the right ventricular lead following the superior vena cava to right ventricle contour. In contrast, the malpositioned wires follow the aortic contour.
Moving image 2. Angiography revealed a trifurcating left main coronary artery with the malpositioned “atrial” pacemaker lead terminating at the branch point of the left anterior descending and ramus intermedius coronary arteries. The pacing lead screw appears fixated to the vessel wall with its distal end exiting the vessel.
Moving image 3. Under fluoroscopic guidance, the pacing leads were quickly removed from the left subclavian artery. A polytetrafluoroethylene (PTFE)-covered self-expanding 8 mm×5.0 cm stent was deployed via a long sheath from the right femoral artery to repair the subclavian arteriotomy.
Online Figure 1. Radiographic appearance of dual chamber pacemaker leads within the left heart. A) Frontal chest radiograph demonstrates the presence of a dual chamber pacemaker with the leads extending above the medial aspect of the left clavicle, consistent with a left subclavian arterial course. The atrial lead projects to the left of the thoracic spine (white arrow) and the ventricular lead projects over the expected position of the left ventricle (black arrow). B) Coronal reformatted images from a contrast-enhanced chest CT showed the atrial lead extending into the proximal left main coronary artery (white arrow). C) The ventricular lead extended across the aortic valve to terminate within the left ventricle (white arrow).
Online Figure 2. Filling defect on angiography and intravascular ultrasound within the left main coronary artery found to be large wire-associated thrombus. A) Upon removal of the pacing lead, a filling defect was observed within the mid portion of the left main coronary artery. B) Intravascular ultrasound confirmed the presence of a filling defect as opposed to a coronary artery dissection, perforation, or other pathologic process. C) Manual thrombectomy retrieved a large wire-associated thrombus from the left coronary system. FD: filling defect