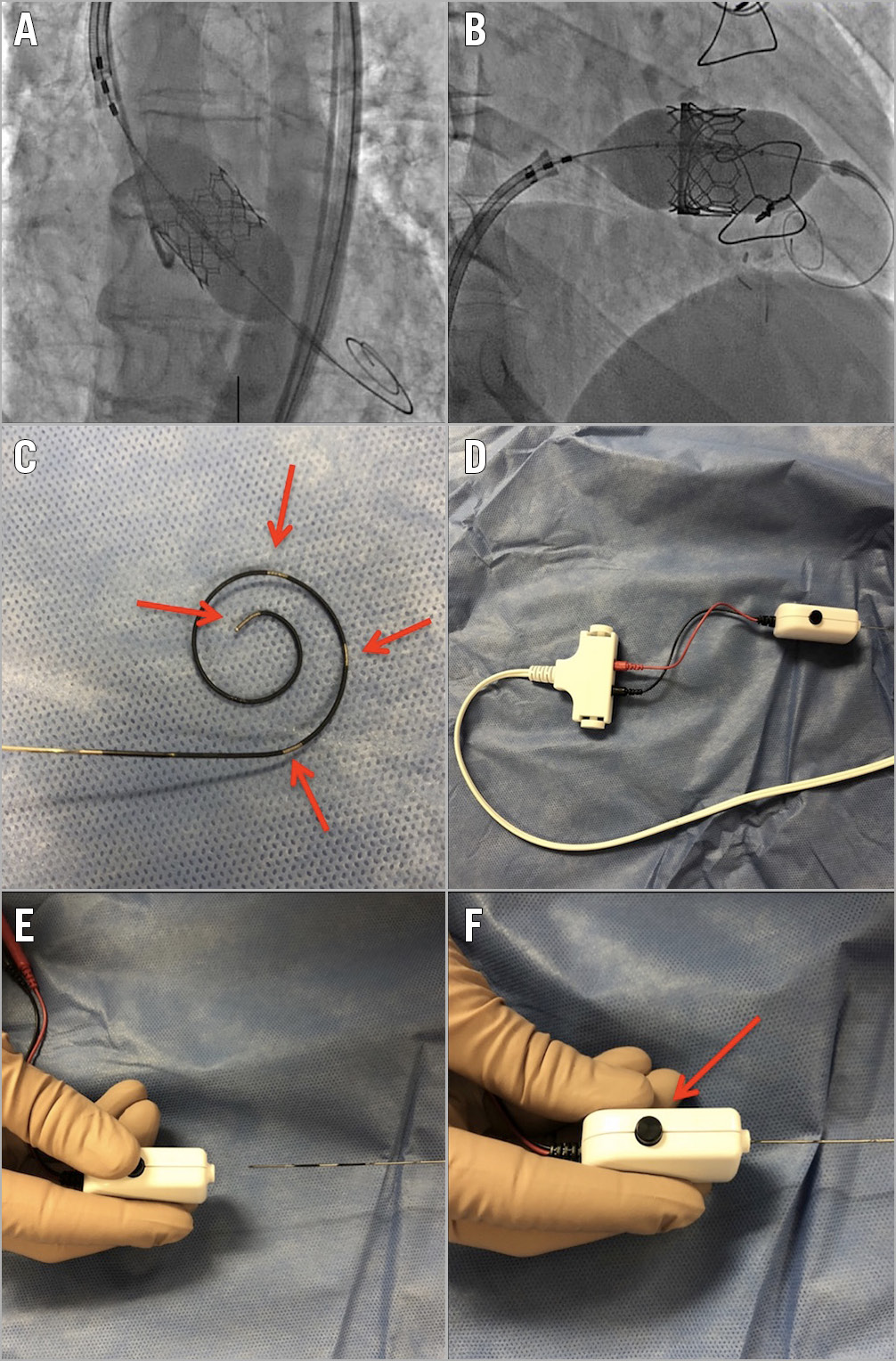
Figure 1. The Wattson temporary pacing guidewire. A) SAPIEN 3 deployment in the aortic position with the Wattson wire. B) Tricuspid valve-in-valve with SAPIEN 3 with the Wattson wire. C) Pigtail with exposed electrodes (arrows). D) Pacing set-up with adaptor connected to external pacing device. E) Connection of adaptor. F) Adaptor release button (arrow).
Transcatheter heart valve implantation generally requires both a ventricular guidewire and a temporary transvenous pacemaker (TVP). TVP insertion is not without risks, namely vascular injury, cardiac perforation and tamponade1. The modification of a ventricular guidewire to deliver unipolar pacing for transcatheter aortic valve implantation (TAVI) has been validated2,3 and has also been described for tricuspid valve-in-valve (TViV) procedures4; however, this requires expertise, adds complexity and may result in high thresholds and unreliable pacing.
We describe the first-in-human experience with the purpose-designed Wattson™ temporary pacing guidewire (Teleflex, Maple Grove, MN, USA) for concomitant valve delivery and pacing. Three patients underwent TAVI and two underwent TViV with a balloon-expandable SAPIEN 3 (Edwards Lifesciences, Irvine, CA, USA) device (Figure 1A, Figure 1B). All valves were successfully implanted under rapid pacing using the Wattson wire. Mean pacing threshold was 2.2±0.45 mA, with sustained blood pressure drop and no loss of capture in any case. There was no pacing requirement post valve delivery and there were no complications.
Using a guidewire as a concomitant pacing wire reduces the risk of venous access-site complications, fluoroscopic time/dose and, notably, the risk of cardiac perforation. Pacing for TViV is particularly challenging as it may necessitate pacing wire placement in the left ventricle or coronary sinus, or guidewire modification.
The Wattson wire is 0.035” in diameter, 280 cm in length and offers similar stiffness to other commercially available moderate-support guidewires. It has a 3 cm diameter distal pigtail with multiple exposed electrodes providing predictable bipolar pacing (Figure 1C). The wire has an adaptor that connects the wire to a standard external pacemaker (Figure 1D-Figure 1F). If pacing is required post valve deployment, the wire length allows removal of the valve delivery system from the sheath while providing pacing and facilitating TVP insertion. In patients at high risk of needing longer-term pacing (e.g., pre-existing high degree atrioventricular block), an indwelling TVP might still be preferred.
In this small series, the Wattson wire offered reliable pacing and rail support for valve delivery in aortic and tricuspid positions. It could potentially make transcatheter valve implantation safer and more efficient but requires further clinical validation.
Conflict of interest statement
D. Daniels will receive royalties from the Wattson temporary pacing guidewire. D. Wood is a consultant to Edwards Lifesciences. J.G. Webb is a consultant to and has received research funding from Edwards Lifesciences, Abbott and Boston Scientific. The other author has no conflicts of interest to declare.