Failure after mitral annuloplasty or replacement is one of the long-term complications after mitral surgery. Reoperation in this frail population is associated with high postoperative mortality and morbidity1. Transcatheter mitral valve replacement (TMVR) procedures, including mitral valve-in-valve (ViV), valve-in-ring (ViR) and valve-in-mitral annular calcification (ViMAC), have recently emerged as off-label alternative therapies for prosthesis dysfunction and severe mitral calcification2. Even though TMVR without rapid pacing has been successfully performed, it can improve valve stability and so optimises deployment and valve positioning. Temporary right ventricle pacing (RVP) is potentially associated with vascular and ventricular complications such as perforations and tamponades. Transcatheter procedures have undergone significant simplifications that have improved intervention duration, complication rates and patient outcomes particularly in this high-risk population. Direct wire pacing (DWP), as with direct left ventricular (LV) pacing in transcatheter aortic valve replacement (TAVR), has been shown to be as efficient as RVP. Procedural cost, duration and fluoroscopy time were significantly lower in the DWP group compared to the RVP group in TAVR3. Similarly to TAVR, we sought to simplify TMVR procedures without sacrificing safety and efficiency.
We report here the first series of DWP via the valve delivery guidewire during TMVR.
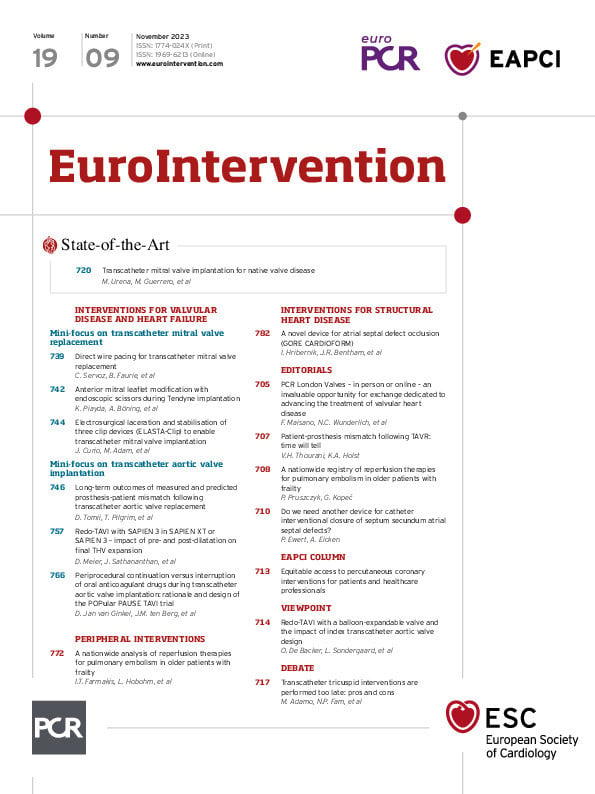
In 4 international centres, TMVR were carried out using the transseptal technique by transfemoral venous approach as previously described4. No additional femoral vein puncture was performed for temporary pacemaker insertion and RVP. The cathode of an external pacemaker was attached to the distal external end of the guidewire using a crocodile clip. The anode (second crocodile clip) was attached to the anaesthetised skin at the main insertion site (Figure 1A). The efficacy of stimulation was tested before valve deployment. During valve deployment, electrical stimulation was delivered in an asynchronous mode at an amplitude of 15 to 25 mA (at the discretion of the operator)

Figure 1. A) Example of DWP during TMVR via the 0.035 inch stiff guidewire placed in the left ventricle. The cathode of an external pacemaker is attached to the distal external end of the guidewire using a crocodile clip. The anode (second crocodile clip) is attached to the incised skin at the insertion site of the arterial sheath in the anaesthetised groin. B) Main results of the DWP TMVR registry. All patients had procedural success. Two patients had major femoral bleeding complications. DWP: direct wire pacing; MACE: major adverse cardiac events; TMVR: transcatheter mitral valve replacement
and a rate of 160 to 220 bpm using a constant-current external pacemaker.
From January 2017 to November 2022, 26 patients underwent TMVR with DWP. Twenty-one patients had a ViV, 2 patients had a ViR and 3 patients had a ViMAC. The mean age was 81.1±9.1 years. Eight patients had severe degenerative mitral stenosis. For 13 patients, valve dysfunction was secondary to severe intraprosthetic insufficiency. High-frequency DWP, through a SAFARI 2 (Boston Scientific) guidewire in all cases, was systematically applied to increase valve placement accuracy.
Technical success was achieved in all patients according to Mitral Valve Academic Research Consortium (MVARC) definitions without interference or damage to the existing mitral prosthesis. The pacing was consistently efficient without any loss of capture. None of the patients required temporary pacing after valve deployment. At discharge, the mean gradient was 4.08±1.20 mmHg, there was no severe intra- or paravalvular leakage, and no patient required permanent pacemaker implantation (Figure 1B).
Movement of the TMVR delivery catheter during adjustment may potentially displace the LV stimulation wire. However, unlike a temporary pacemaker that has a punctiform shape, the LV wire has a large pigtail shape that maintains contact with the endocardium without losing capture. Additionally, we did not observe any cases of LV perforation in our series, but caution must be taken when handling the LV guidewire to avoid this severe complication.
In the future, the incidence of symptomatic valve deterioration and MAC are expected to increase. TMVR with balloon-expandable valves, after careful screening, are a less invasive treatment option in highly selected patients presenting with a failing mitral valve bioprosthesis, failing mitral annuloplasty or presenting with severe MAC. Rapid ventricular pacing during TMVR allows for an accurate deployment and optimisation of valve positioning. Rapid pacing through a venous access with a temporary pacemaker needs an additional vascular access that may lead to haematoma, arterovenous fistula or thrombosis, in addition to the risk of right ventricle perforation. Also, temporary pacemakers and TMVR catheters can have deleterious interactions between them in the inferior vena cava or right atrium leading to pacing with loss of capture and valve dislodgment, for instance.
In our registry, TMVR with DWP seems to be as efficient as LV pacing during TAVR and so could contribute to simplifying TMVR interventions and may further decrease complications, procedural time, cost and radiation.
Conflict of interest statement
B. Faurie is afounder and shareholder of Electroducer. The other authors have no conflicts of interest to declare.