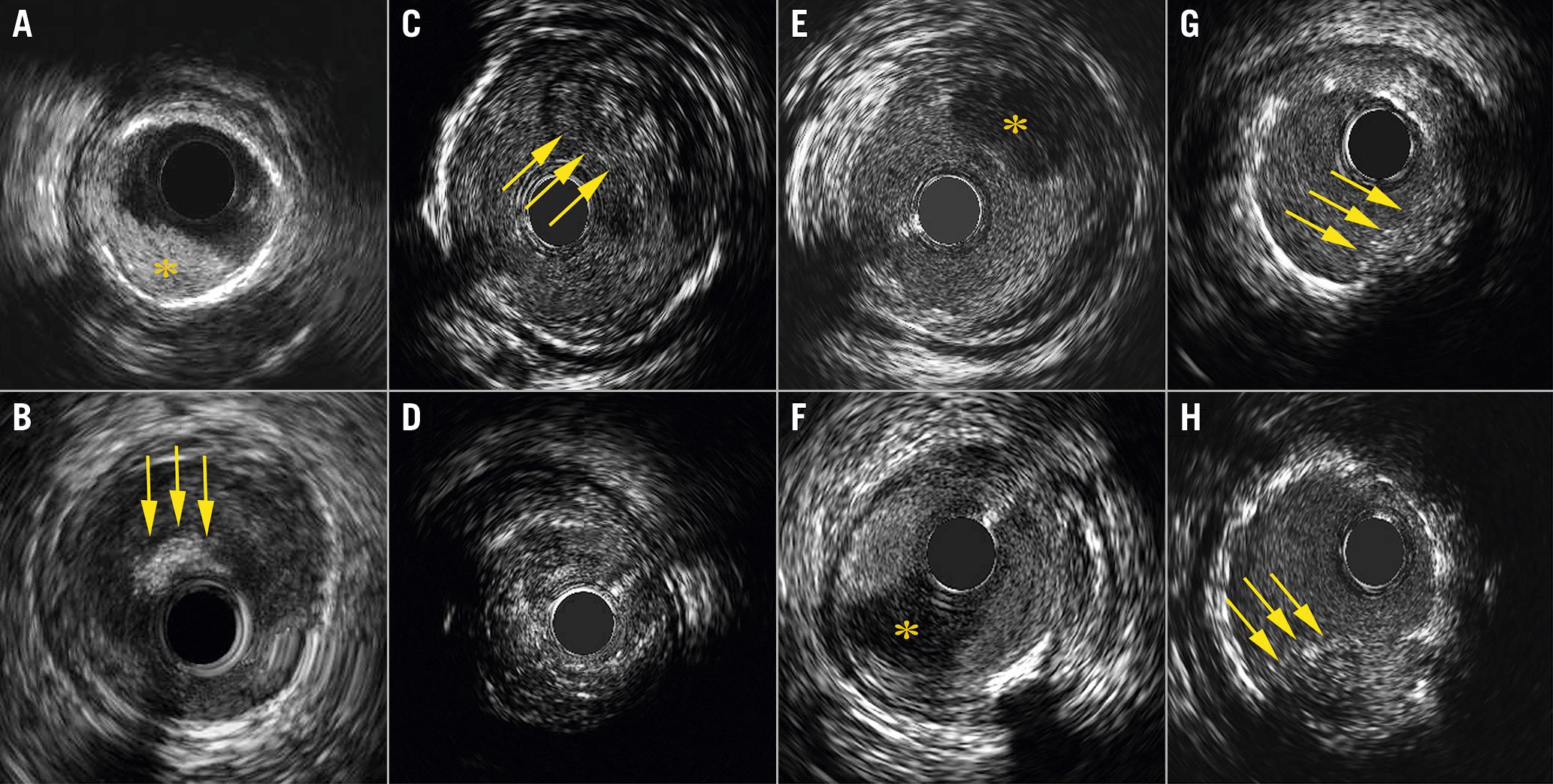
Figure 1. A showcase of different types of intracoronary thrombi visualised with high-definition intravascular ultrasound. A) Acute thrombus (asterisk) with a bright appearance, sharp delineation and no signal attenuation. B) Acute thrombus on the tip of the intravascular ultrasound (IVUS) catheter (arrows). C) Subacute thrombus with a light to dark grey appearance, white speckles and less clear delineation (arrows). D) 360 degrees of subacute thrombus with severe signal attenuation. E-F) Organised thrombus (asterisks) with a homogeneous dark appearance starting from the lumen wall, sharp delineation and in some cases mild signal attenuation. G-H) Thrombus protrusion (arrows) visualised as a lobulated light to dark grey appearance protruding into the lumen and covering multiple stent struts.
Intracoronary thrombosis plays a critical role in the aetiology and subsequent prognosis of patients presenting with acute coronary syndrome and in patients with ST-segment elevation myocardial infarction (STEMI) in particular. Although thrombi can be recognised with conventional coronary angiography, they can be better appreciated with intravascular ultrasound (IVUS). In the IVUS expert consensus document (2001), a thrombus was defined as an intraluminal mass, often with a layered, lobulated or pedunculated aspect and a relatively echolucent appearance or a more variable grey scale with speckling or scintillation1. It stated that its diagnosis by IVUS should always be considered presumptive1.
With the introduction of higher frequency IVUS systems, the ability to visualise thrombi has increased substantially. However, IVUS definitions for thrombus types are lacking.
Examples showcased in this Interventional Flashlight are derived from the currently ongoing prospective observational “Tissue Characterization and Primary Percutaneous Coronary Intervention Guidance Using Intravascular Ultrasound’’ SPECTRUM study (Clinicaltrials.gov: NCT05007535), in which protocolised pre- and post-intervention IVUS pullbacks are performed in 200 STEMI patients with a 40-60 MHz high-definition IVUS catheter (Kodama; ACIST Medical Systems, Inc.).
Thrombi were categorised into three main IVUS defined types: acute thrombus (AT), subacute thrombus (ST) and organised thrombus (OT)2.
We define AT (platelet aggregation) on IVUS as an acoustic inhomogeneous bright “spontaneous contrast” appearance with sharp delineation and no signal attenuation (Figure 1A, Figure 1B, Moving image 1, Moving image 2). Although rarely encountered, AT may be visible during periprocedural imaging due to intimal disruption (following balloon dilatation) or on the tip of the IVUS catheter (often linked to low platelet-activating clotting time).
Subacute thrombus is the most common form of thrombus that can be appreciated by IVUS. Its acoustic appearance is more homogeneous as compared to AT and thus ST appears darker. We define ST as a light to dark grey layered appearance with white speckles and a less clear delineation (Figure 1C, Figure 1D, Moving image 3, Moving image 4). Moderate to severe signal attenuation (SA) may also be observed, which is probably due to deviation or absorption of ultrasound waves by ST or underlying soft (necrotic) tissue.
The most acoustic homogeneous type of thrombus is OT (granulation), which we define as having a homogeneous dark appearance, clearly starting from the lumen wall with sharp delineation and in some cases mild SA (Figure 1E, Figure 1F, Moving image 5, Moving image 6). Finally, post-stenting thrombus protrusion can be observed with IVUS, defined as a lobulated, light to dark grey layered appearance that protrudes in the lumen and covers multiple stent struts (Figure 1G, Figure 1H, Moving image 7, Moving image 8).
Different thrombus types may require different treatment strategies. An AT on the IVUS catheter is often due to insufficient anticoagulation. Operators should consider the administration of additional heparin and/or removal of the respective material in order to avoid complications. If a large amount of ST is found, operators may opt for a strategy including aspiration thrombectomy and/or administration of glycoprotein IIb/IIIa antagonists. Conversely, in case of OT (attached to vessel wall) or no thrombus at all, these treatment strategies might not be sufficient. Finally, operators should act carefully in case of extensive thrombus protrusion, as additional post-dilatation hypothetically may lead to more distal embolisation, which is associated with no-reflow. Nevertheless, future research is needed to confirm these hypotheses.
The present work challenges the earlier presumptive statement on IVUS-detected thrombi but supports the ability to assess thrombi with a high level of certainty when using current-generation, high-definition IVUS systems.
In conclusion, the thrombus types and IVUS definitions as presented in this Interventional Flashlight may help operators in recognising different types of thrombus and provide guidance in choosing specific treatment strategies or thrombus classification in scientific proceedings.
Conflict of interest statement
J. Daemen received institutional grant/research support from AstraZeneca, Abbott Vascular, Boston Scientific, ACIST Medical, Medtronic, MicroPort, Pie Medical, and ReCor Medical. J. Ligthart received speaking fees from Boston Scientific, Philips Volcano, ACIST Medical, Abbott Vascular and Pie Medical. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Acute thrombus (arrow) with a bright appearance, sharp delineation and no signal attenuation.
Moving image 2. Acute thrombus (arrow) on the tip of the intravascular ultrasound catheter.
Moving image 3. Subacute thrombus (arrow) with a light to dark grey appearance, white speckles and less clear delineation.
Moving image 4. Subacute thrombus with severe signal attenuation.
Moving images 5. Organised thrombus (arrow) with a homogeneous dark appearance and clearly starting from the lumen wall with sharp delineation.
Moving images 6. Organised thrombus (arrow) with a homogeneous dark appearance and clearly starting from the lumen wall with sharp delineation.
Moving images 7. Thrombus protrusion (arrow) visualised as a lobulated light to dark grey appearance protruding into the lumen and covering multiple stent struts.
Moving images 8. Thrombus protrusion (arrow) visualised as a lobulated light to dark grey appearance protruding into the lumen and covering multiple stent struts.