“Trust not too much to appearances” - Virgil
Paravalvular aortic regurgitation (PAR) is an important determinant of outcome following transcatheter aortic valve implantation (TAVI); patients with significant PAR remain more symptomatic and have reduced life expectancy compared to those with little/no paravalvular leak1. Quantification of PAR, however, remains a considerable challenge despite the development of echocardiographic, angiographic, and haemodynamic assessment algorithms2. Two-dimensional echocardiography (2D-echo) is recommended to determine the location (trans- or paravalvular), mechanism, and severity of PAR2. By extension, 2D-echo determines the requirement for and likely success of additional bail-out interventions to treat significant PAR. Unfortunately, 2D-echo may not be sufficiently sensitive to quantify PAR accurately in a sizeable proportion of patients. Colour flow Doppler can be difficult to interpret due to the eccentric nature of the regurgitant jets and fluctuating intraoperative haemodynamics, and semi-quantitative measures require further validation in TAVI cohorts3.
Multislice computed tomography-based TAVI sizing4, operator experience5, and novel transcatheter heart valve designs have impacted considerably on the incidence of significant PAR (≥grade 2)6. The reported incidence of moderate to severe PAR is <3% among patients treated with Lotus™ (Boston Scientific, Marlborough, MA, USA), CoreValve® Evolut™ R (Medtronic, Minneapolis, MN, USA) or SAPIEN 3 (Edwards Lifesciences, Irvine, CA, USA) prostheses. When PAR does occur, it can be managed by post-implant balloon dilatation, transcatheter valve repositioning, implantation of a second transcatheter valve, or device-mediated leak closure7. These bail-out strategies can moderate or completely resolve PAR, but have also been associated with important morbidity and mortality7. Hence, such manoeuvres are used only when the volume of PAR is sufficient to impact on clinical outcome. Intuitively, greater regurgitant volumes should yield worse clinical outcomes; thus, it is somewhat puzzling that mild and moderate PAR have been associated with equivalent morbidity and mortality1. Perhaps mild and moderate PAR are equally detrimental to the hypertrophied aortic stenosis ventricle? A more likely explanation, however, is the erroneous categorisation of patients with moderate PAR as mild, and vice versa. While no/trivial or severe PAR can be reliably and reproducibly determined by echocardiographic or angiographic means, the categorisation of mild or moderate PAR remains largely “in the eye of the beholder”. Thus, misclassification can result in patients being subjected to unnecessary bail-out interventions or worse, left with prognosis-altering PAR.
Given this diagnostic conundrum, there is a considerable need for a reliable, reproducible, and validated measure of PAR that can be applied during the index intervention. In 2012, Sinning and colleagues described the aortic regurgitation index (ARi) using the following formula: ([Diastolic BP – Left Ventricular End Diastolic Pressure (LVEDP)]/Systolic BP)×100, and illustrated the utility of this score to categorise PAR further8. When dichotomised according to an ARi < or ≥25, patients with an ARi <25 had increased one-year mortality. The reliability of this index, however, can depend on a variety of factors, including heart rate and pre-existing loading conditions. Indeed, an ARi <25 can occur in patients with little or no PAR, thereby limiting its application in isolation. Consequently, Sinning and colleagues from Bonn have recently suggested a composite aortic insufficiency (CAI) score. This algorithm filters patients with echocardiographic or angiographic no/trivial PAR (CAI 0) or moderate/severe (CAI 3) PAR, and then recommends the use of the ARi in those with mild PAR to decipher “real” mild (CAI 1) from moderate (CAI 2) PAR.
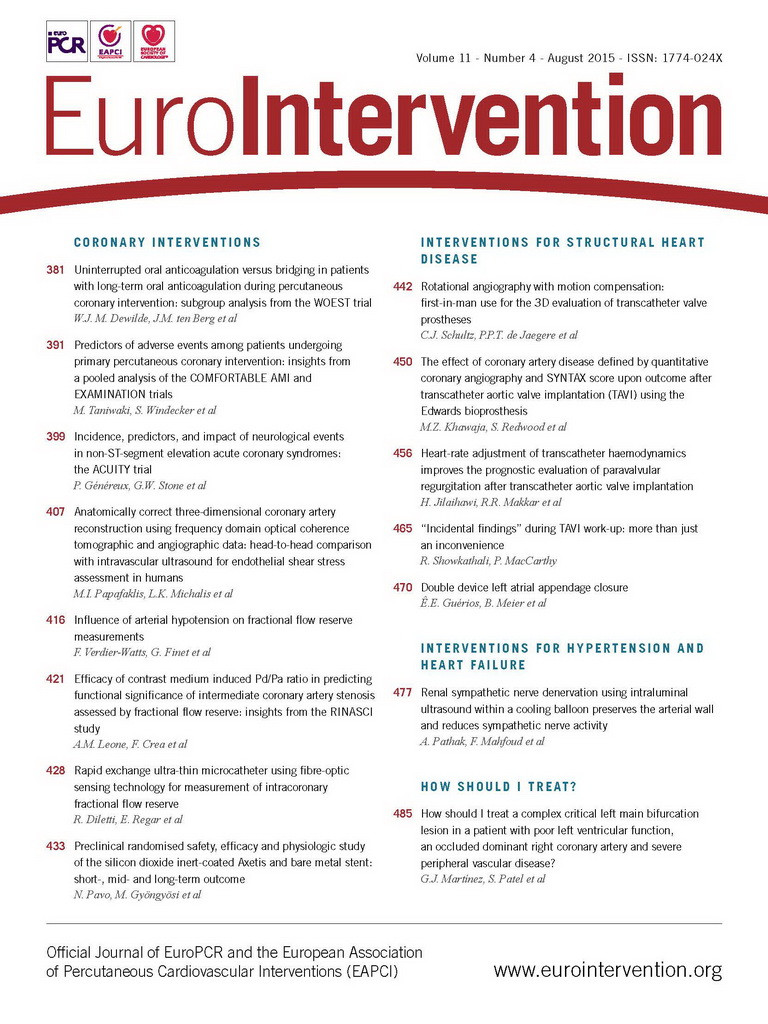
In this issue of EuroIntervention, Jilaihawi and colleagues present the heart rate-adjusted haemodynamic-echocardiographic aortic insufficiency (CHAI) score9. Similar to the Bonn CAI score, this index filters patients with no/trivial (CHAI 0) or severe (CHAI 3) PAR (with 2D transoesophageal echocardiography [TOE]), and then combines mild or moderate PAR as an intermediate PAR group. This latter group is then stratified according to the heart rate-adjusted diastolic delta: (Diastolic BP – LVEDP)/heart rate×80. Using a CHAI score cut point of 25 (>25=CHAI 1; ≤25=CHAI 2), this index outperformed TOE alone and the Bonn CAI score for stratification of one-year mortality among patients with intermediate PAR. The CHAI score therefore appears to add incremental value in the immediate assessment of patients with mild to moderate (intermediate) PAR post TAVI, by identifying those patients with less favourable long-term outcomes.
Jilaihawi and colleagues should be congratulated for the refinement of the ARi. Further study is required, however, to determine whether additional intervention based on the CHAI score improves clinical outcome. As we treat younger and lower-risk patients with transcatheter technologies, there is an onus on the community to minimise the proportion of patients with residual significant PAR. Much progress has been made in this respect and the CHAI score represents another step in the right direction.
Conflict of interest statement
N. Piazza is a consultant for Medtronic and MicroPort. D. Mylotte is a consultant for Medtronic and MicroPort. H. Makki has no conflicts of interest to declare.