Transcatheter aortic valve implantation (TAVI) has revolutionised the treatment of aortic valve stenosis and has set the stage for a broad array of interventional options in patients with valvular heart disease. One of the main reasons why TAVI has matured in a relatively short period of time has been the early recognition of procedural drawbacks coupled with technical and technological improvements that overcome these limitations. A striking example is paravalvular regurgitation (PVR). Since the early recognition of the deleterious association of PVR with mortality after TAVI1, numerous studies have addressed its exact causes, predictors, its evolution over time, and -most importantly- its standardised assessment. With careful refinement of technique (predominantly through routine application of 3D computed tomography for valve sizing and selection) and technology (including repositionability and the introduction of sealing skirts), the incidence of post-TAVI PVR has markedly decreased2. Accordingly, the focus has shifted towards other limitations of the technology, and the interest in PVR has steadily declined. Nevertheless, the incidence of PVR remains higher after TAVI compared to surgery2, and several questions in this context remain unanswered.
With this background, the study by Chau et al, published in this issue of the journal, is an important contribution to the available literature on post-TAVI PVR, as it provides answers to a variety of unsettled issues3. The authors did a post hoc analysis of 1,947 intermediate risk patients receiving TAVI in the PARTNER 2A randomised trial (n=947) and the PARTNER S3 intermediate risk registry (n=1,027). Overall, 40% had mild or more post-TAVI PVR, and 6% had more than mild PVR. The latter was more common in the randomised trial, which is most probably related to the use of an older generation device and the lack of systematic preprocedural computed tomography. At two years, all-cause and cardiovascular mortality were both significantly higher in patients with moderate or more PVR, but not in those with mild PVR. Rehospitalisation rates (largely heart-failure related) and reinterventions were also more common in patients with moderate or more PVR. These patients had larger left ventricular (LV) dimensions and volumes and a lower LV ejection fraction compared to baseline, and LV mass regression was almost absent. An important strength of this analysis lies in the rigorous assessment of PVR in a core laboratory at all time points, as well as the classification of the degree of PVR according to a well-established multiparametric approach. In addition, statistical adjustment was performed by both multivariable and propensity score adjusted models. Furthermore, a landmark analysis to assess the impact of PVR on clinical outcomes between one and two years was performed, with additional adjustment to changes in LV dimensions and function between baseline and one year.
The study robustly confirms the strong association of moderate or more PVR and mortality up to two years after TAVI. However, the impact of untreated residual PVR beyond two years remains debatable and cannot be assessed from the current analysis. In the German TAVI registry, residual PVR remained an important prognostic factor at five years4. In the United Kingdom TAVI registry, the survival curves of patients with moderate or severe PVR and those with mild or no PVR separated early but remained parallel from two to seven years5. Data on the impact of corrective measures on outcome and whether this is time sensitive or not are unavailable. Thus, longer-term analyses from this and other datasets are required to assess whether the deleterious effect of PVR extends beyond two years, and whether corrective measures are able to revert its adverse prognostic impact.
An interesting observation in this study is that all clinical and echocardiographic outcome measures seem to point to a plausible causal association between moderate or more PVR and outcome. Therefore, the study adds important mechanistic insights on the pathophysiological effect of post-TAVI PVR. In a previous small study using post-TAVI cardiac magnetic resonance imaging (CMR), we observed a significant correlation between the CMR-derived regurgitant fraction after TAVI and changes in the end diastolic volume (EDV) at six months. Significant changes of LV ejection fraction, EDV and LV mass only occurred in patients with no or mild PVR post-TAVI, whereas those parameters remained unchanged in patients with ≥moderate PVR6. These findings have now been confirmed and extended to a much larger patient group using echocardiography up to two years after TAVI. The changes in LV dimensions and volumes and the blunted remodelling process together with the higher heart-failure-related rehospitalisation rates and reinterventions strongly point to a causal relationship between PVR and mortality.
Although the study does not show an important association between mild PVR and outcome, defining mild PVR remains a clinical challenge. In the study by Chau et al, the degree of PVR was meticulously assessed by a dedicated echocardiographic core laboratory using multiple (more than 10) different parameters3. However, Hahn et al reported that in the PARTNER 2 trial cohort, evaluation by a core laboratory and a consortium of echocardiographers revealed a low reproducibility in PVR evaluation using multiple quantitative parameters7. In a clinical setting, accurate graduation of PVR is even more challenging, and often requires integration of clinical, laboratory and other imaging-based findings. Thus, although the graduation of PVR in this study appears to be clearly of prognostic relevance, extending these observations to a real-world population with “mild” PVR and granting them automatically a good prognosis may be problematic, as the cohorts with mild post-TAVI PVR are considerably heterogeneous. On the other hand, identification of patients with prognostically relevant PVR may be facilitated by the temporal assessment of LV structural and functional recovery as suggested from this study.
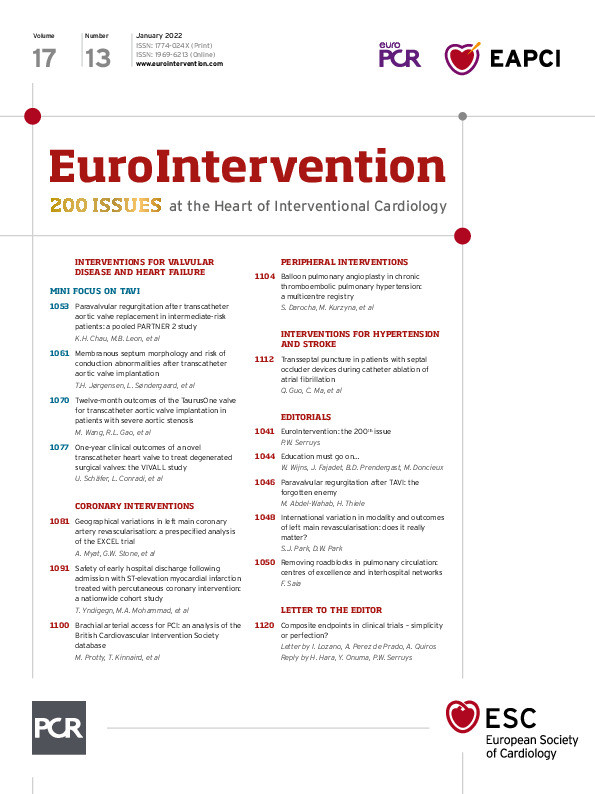
Chau et al should be congratulated for reminding the interventional community of an enemy that has been at least partially forgotten. As TAVI is exponentially expanding to lower-risk and younger patients, relevant post-procedural PVR with its deleterious prognostic impact should not be accepted to begin with and needs to be eliminated completely.
Conflict of interest statement
M. Abdel-Wahab reports that his hospital receives consulting fees and/or honoraria on his behalf from Boston Scientific and Medtronic. H. Thiele has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.