Abstract
Aortic regurgitation (AR) is an important predictor of adverse prognosis after transcatheter aortic valve implantation (TAVI) by both self-expanding and balloon-expandable prostheses and is predominantly paravalvular (PV). The mounting evidence for moderate/severe PV AR as an independent predictor of mortality is discussed. Moreover, there is an unclear impact on prognosis of mild PV AR that is most likely the result of imperfect assessment of this complication, which currently remains semi-quantitative. The relevance of its accurate quantification to reliable prognostication is described, along with how this data might be used to guide intervention and optimise outcomes of patients with PV AR.
Introduction
Aortic regurgitation (AR) is an important predictor of adverse prognosis after transcatheter aortic valve implantation (TAVI) by both self-expanding and balloon-expandable prostheses and is predominantly paravalvular1-5. It occurs commonly, and is at least mild in around one half of patients or more. Although difficult to quantify, PV AR is significant (moderate/severe) in at least 10% of patients. Significant PV AR is not only associated with mortality but has been shown to be an independent predictor in multiple studies. The prognostic impact of PV AR after TAVI should be viewed in the context of the expected benefit of TAVI.
Prognosis of significant PV AR in context
Two-year analysis of survival in inoperable patients undergoing TAVI has demonstrated a hazard ratio (HR) for TAVI relative to standard therapy (ST) of 0.56 (95% CI, 0.43–0.73, p<0.001)6. Viewed conversely, the HR for ST relative to TAVI was 1.79 (95% CI, 1.37-2.32, p<0.001). In several multivariable analyses, significant PV AR carried a HR for all-cause mortality of between 1.66 and 3.79 (Table 1), similar or greater to the hazard of ST vs. TAVI in the inoperable arm of the PARTNER trial. This suggests that the occurrence of significant PV AR may negate the survival benefit of TAVI and render the procedure futile. It may even worsen the natural history of some patients with aortic stenosis. This emphasises the need for avoidance of this important complication with reliable prosthesis sizing and positioning or prompt treatment, should it occur.
The prognosis of lesser degrees of PV AR
Recent data from long-term follow-up of patients in the REVIVAL trial, who underwent TAVI and corelab echocardiographic analyses, has suggested that mild PV AR is common but follows a benign course with no increase in mortality7. This is in line with prior surgical data suggesting that small paraprosthetic leaks are benign during the first year after heart valve replacement8.
Against this is data from the operable (high-risk) arm of the US PARTNER trial which has suggested that even mild PV AR is associated with increased mortality5. Kodali et al, as part of the two-year follow-up of patients randomised to balloon-expandable TAVI stratified patients by grade of post-procedural PV AR, and found that patients with mild PV AR followed a similar clinical course to patients with moderate or severe PV AR, with a mortality greater than those with no or trivial AR. The stratification by total AR seems to show a dose response of AR, indicating that the total sum of PV and central AR may be most important (Figure 1). Importantly, although the echocardiograms were assessed in a core laboratory, this was not a multivariable analysis and it is conceivable that mild AR has important associations with baseline comorbidities that may influence prognosis. Moreover, even with a corelab analysis, the assessment of PV AR remains difficult and it is probable that many cases of mild PV AR are actually more than mild. Cases of mild PV AR are frequently observed that have some but not all the criteria of moderate AR as defined by the Valve Academic Research Consortium , lending support to an additional category of PV AR “mild/moderate”, and the concept of “more than mild” AR that is part of our own echo lab’s routine reporting.
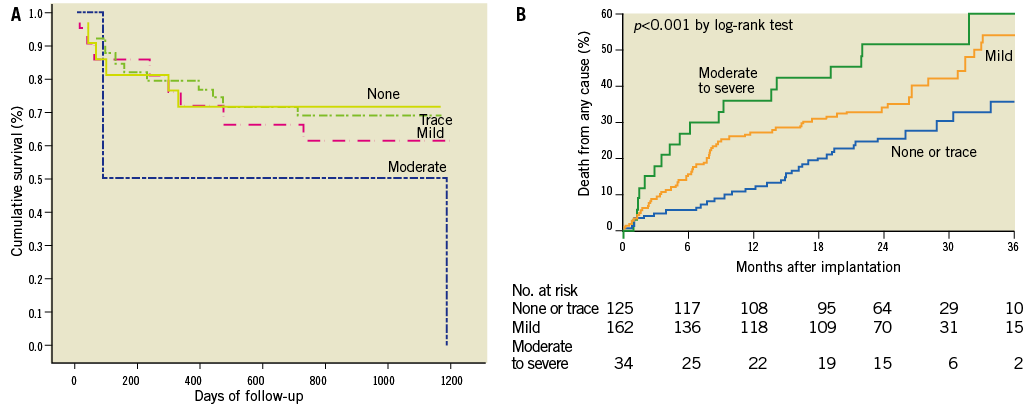
Figure 1. Relation of grades of total AR (central and PV AR, predominantly paravalvular) after balloon-expandable TAVI to (A) survival and (B) mortality (corelab analyses of post TAVI transthoracic echocardiograms). A) Cumulative survival in the REVIVAL trial7. B) All-cause mortality as an as-treated analysis of the US PARTNER trial (cohort A)5. Events were calculated with the use of Kaplan-Meier methods. Reproduced with permission.
The importance of the reliable quantification of post TAVI AR to its prognostication
The methodology of quantification of aortic regurgitation after TAVI is fundamental to its prognostication and has been addressed earlier in the review of this topic. There is an absence of a clear gold standard and there may also be important differences in the imaging modality used to assess this complication. The assessment of PV AR is still at best semi-quantitative rather than truly quantitative, which is important to the reliable evaluation of prognosis by this complication. Sinning et al recently made important progress in this regard, quantifying post TAVI AR using a diastolic transcatheter pressure gradient-derived “AR index” (Figure 2)1. They demonstrated that the AR index was not only highly correlated to PV AR but also had incremental prognostic value in multivariable analysis (Table 1).
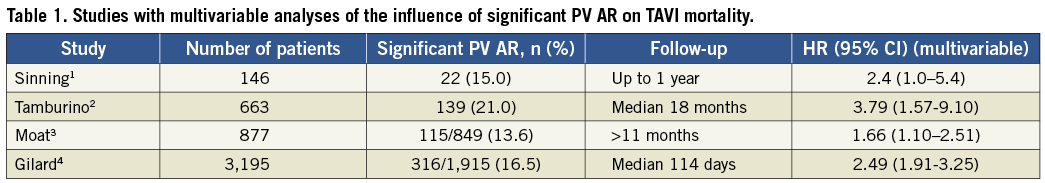
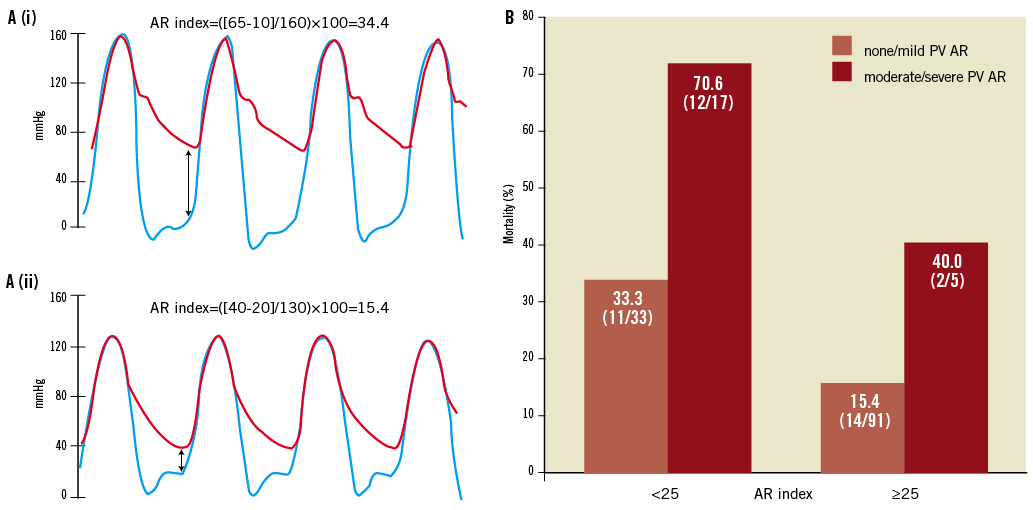
Figure 2. The AR index. A) Simultaneous determination of left ventricular end-diastolic pressure (LVEDP) (blue line) and diastolic blood pressure (DBP) in the aorta (red line) (i) in a patient without PV AR and (ii) in a patient with moderate PV AR. AR index=([DBP-LVEDP]/SBP) ×100. B) One-year all-cause mortality (%) stratified by significant PV AR and AR index ≥25, showing their interaction. Reproduced with permission1.
Conclusions
Paravalvular aortic regurgitation is common after TAVI. It is one of the most important complications of the procedure, clearly demonstrated to be an independent predictor of mortality in several multivariable analyses. Its reliable quantification in the context of outcomes is fundamental to its refinement as a prognosticator, and to guiding the TAVI operator as to when further intervention is required.
Conflict of interest statement
R.R. Makkar is a consultant to Abbott Vascular, Cordis Corporation and Medtronic. He is a speaker for Eli Lilly, receives a grant from Edwards Lifesciences and St. Jude Medical, and is a stockholder of Entourage Medical. H. Jilaihawi is a consultant to Edwards Lifesciences and St. Jude Medical and Venus Medtech.