Abstract
Aims: To evaluate: 1) the causes of emergency conversion from transcatheter aortic valve implantation (TAVI) to surgery, 2) procedural settings, and 3) short-term outcome of converted patients.
Methods and results: The prospective German TAVI registry was used to identify patients who underwent bail-out surgery during TAVI. Additionally, standardised questionnaires were developed and used to assess more detailed periprocedural and postprocedural data. Emergency conversion from TAVI to open cardiac surgery was required in 24 of 1,975 patients (1.2%). Primary conversion causes were aorto-valvular complications (i.e., aortic annulus rupture, aortic perforation, or thoracic aortic dissection). This was followed by prosthesis embolisation, myocardial perforation, severe aortic regurgitation, and coronary obstructions. The mean time interval between abortions of TAVI to surgery was 19 minutes (SD±17 min, range 5-80 min). Four of 24 patients (16.7%) died during the initial surgery, seven of 24 (29.2%) within the first 72 hours and the 30-day mortality was 45.8%. The highest mortality was observed in patients with aortic perforation or dissection (4/5, 80%). Mortality rates for other entities were: prosthesis embolisation 40% (2/5), myocardial perforation 50% (2/4), annulus rupture 67% (2/3), severe aortic regurgitation 33% (1/3), and coronary impairment 0% (0/3).
Conclusions: Emergency conversion from TAVI to surgery is a rare event carrying a mortality of around 45% after 30 days. Outcome of converted patients with prior injury of aortic, aorto-valvular, or myocardial tissue during TAVI was poor, whereas patients with severe aortic regurgitation and those with coronary complications had a more favourable outcome after 30 days. Collected procedural and outcome data demand on-site cardiac surgery as a prerequisite for TAVI and constant process optimisation efforts regarding such emergency scenarios.
Introduction
Emergency conversion from transcatheter aortic valve implantation (TAVI) to open heart surgery has been reported in 0.5 to 2.7% of patients1-5. Compared to the transapical method, there seems to be a trend so far towards a lower conversion rate in TAVI procedures performed via the femoral artery. Despite the relatively low incidence of surgical conversions, such an event obviously has a serious impact on patient outcome. This is underlined by a recent publication identifying surgical conversion as a strong predictor (OR 38.68) for an adverse patient outcome during short-term follow-up5. Detailed information on this serious event is currently very sparse; we sought to evaluate the German TAVI registry concerning: 1) the causes for emergency conversion from transcatheter aortic valve implantation to surgery, 2) procedural settings, and 3) the short-term outcome of converted patients.
Methods
The specifications of the German TAVI registry have been described elsewhere6. The prospective German TAVI registry was used to filter patients who underwent bail-out surgery during TAVI between January 2009 and July 2011. Emergent conversion from TAVI to surgery was defined as a TAVI-related, life-threatening complication, occurring strictly peri-interventionally, and making immediate open heart/aortic surgery indispensable. Thus, all complications arising after closure of the access site or complications that did not necessitate open heart/aortic surgery (e.g., pericardial centesis, peripheral vascular complications or life-threatening retroperitoneal bleeding) were excluded.
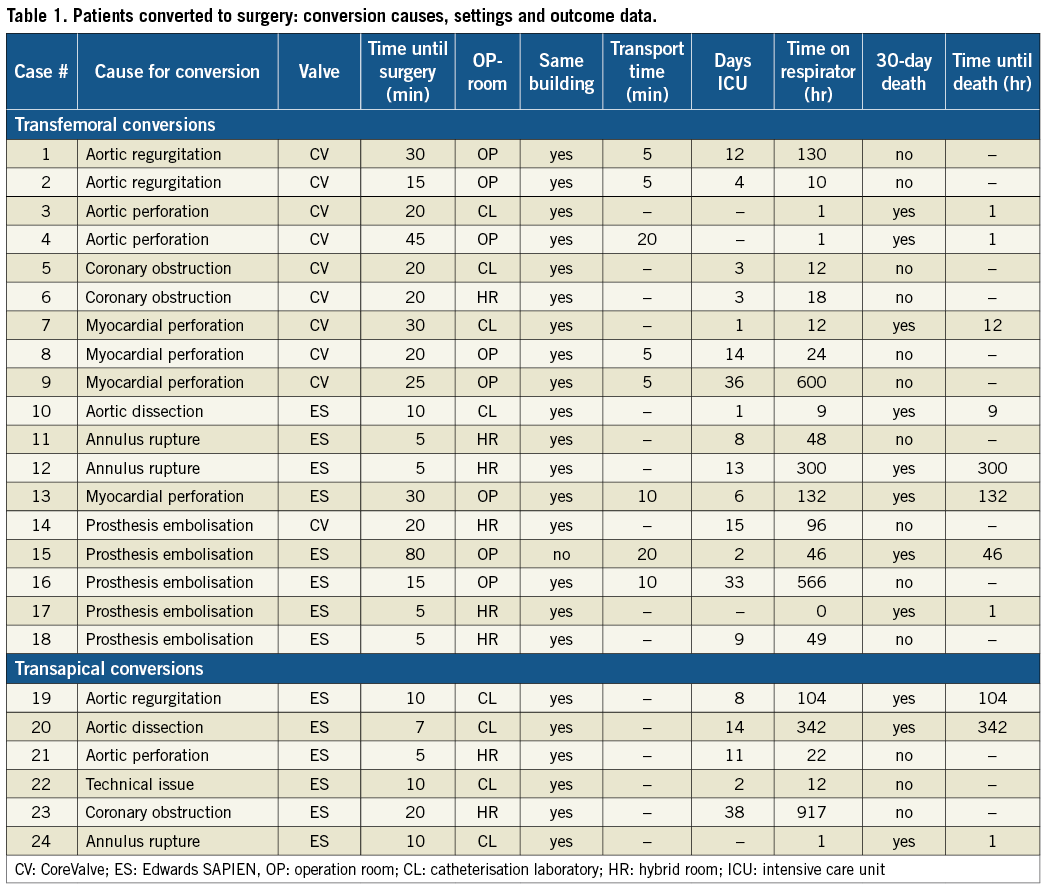
Of the original 28 registered conversion patients within the database, two patients were electively converted to surgery, and another two patients had been documented as converted by mistake, which led to their exclusion from the current analysis. Standardised questionnaires were developed for the remaining 24 patients and used to assess more detailed periprocedural and postprocedural data from the respective institution. The questionnaire items and results are displayed in Table 1. Additionally, it asked for complications during short-term follow-up.
Results
Twenty-four out of 1,975 (1.2%) patients were converted to surgery during initial transcatheter aortic valve implantation. The mean age of this population was 81.5±7.1 years, mean EuroSCORE 22±13%, 87.5% of the patients were in NYHA Functional Class III or IV, and 29.2% of male gender. Concerning the transfemoral access route, 18 of 1,720 patients (1.0%) underwent emergency conversion. Of these, ten patients were scheduled to receive a replacement of their native valve by a CoreValve (Medtronic, Minneapolis, MN, USA) prosthesis and eight of 18 by an Edwards prosthesis (Edwards Lifesciences, Irvine, CA, USA) (Table 1). Of 255 patients receiving transapical valve implantation with the Edwards prosthesis, six needed bail-out surgery (2.4%).
CAUSES FOR EMERGENT CONVERSION
In all patients, the cause for conversion could be identified and this information is shown in Table 1. The most frequent complications were aorto-valvular complications, encountered in eight of 24 patients. Entities summarised as aorto-valvular complications were aortic perforation (3/8), annulus rupture (3/8), and aortic dissection (2/8). The second most frequent cause was prosthesis embolisation, which was found in five patients. Four of five valve embolisations occurred with the Edwards prosthesis. Myocardial perforation was the cause of four of 24 conversions: three of them were CoreValve procedures. So far, conversions due to prosthesis embolisation and myocardial perforation have exclusively been found with transfemoral procedures. Acute, severe aortic regurgitation and coronary obstruction were found in three patients each.
PROCEDURAL SETTINGS
On-site cardiac surgery was available in 12 of 13 institutions. Table 1 displays information on procedural settings including time elapsed until surgery, transport time, and location of surgery. Bail-out surgery was performed in the same room as TAVI in 16 of 24 conversion cases (66.7%). Mean transport time to the operation room for the remaining eight patients was 10 minutes (range 5 to 20 minutes). One institution had no on-site cardiac surgery facility. Thus, transportation to an external department was necessary (Table 1, case 15). Mean time from abortion of TAVI to thoracotomy was 19 minutes (range 5-80 minutes): 10 minutes for transapical and 22 minutes for transfemoral procedures. Eight of 24 (33.3%) surgical procedures took place in an operating theatre, the others in a catheterisation laboratory (8/24) or hybrid room (8/24).
IMMEDIATE AND SHORT-TERM PATIENT OUTCOME
Four of 24 patients (16.7%) died during the initial surgery: two of them were due to aortic perforations, one because of prosthesis embolisation and one following annulus rupture. During the first 72 hours, another three patients died following either surgical repair of aortic dissection, myocardial perforation, or prosthesis embolisation, respectively. This resulted in an immediate procedural mortality of 29.2% (7/24). The 30-day mortality was 45.8% (11/24). Of these, four patients died after the first 72 hours. The causes of these four deaths were: 1) intestinal ischaemia followed by multi-organ failure due to severe sepsis after prior repair of annulus rupture; 2) prolonged cardiogenic shock with peripheral embolisation after prior repair of myocardial perforation; 3) sepsis after prior repair of aortic dissection; 4) non-specified cardiovascular death (unsuccessful reanimation efforts, no autopsy) after prior repair of severe aortic regurgitation.
Concerning the causes for conversion, the highest acute mortality was observed in patients with aortic perforation (67%, 2/3). One patient survived after repair of aortic perforation in a hybrid room (latency until surgery: five minutes). Acute annulus rupture was successfully managed by the surgeon in two of three patients. Despite this initial surgical success, one patient died from intestinal ischaemia and sepsis 13 days after the procedure; the other patient survived, but sustained a stroke during short-term follow-up. Similarly, aortic dissection was successfully operated in both patients. However, one patient died nine hours after surgery (refractory cardiogenic shock on mechanical assist device), and the other one died after 14 days due to sepsis.
In summary, the short-term (30-day) mortality rates – subdivided into complication types – were: aortic perforation or dissection 80% (4/5), prosthesis embolisation 40% (2/5), myocardial perforation 50% (2/4), annulus rupture 67% (2/3), severe aortic regurgitation 33% (1/3), and coronary obstruction 0% (0/3). Furthermore, two patients with prior surgical correction of myocardial perforation suffered from stroke within the first 30 days. The percentage of patients free from death, myocardial infarction, peripheral embolic event, life-threatening or disabling bleeding and stroke was 33.3% (8/24). In one patient scheduled for transapical valve implantation, who had received mechanical mitral valve replacement in the past, the Edwards prosthesis got stuck in the mechanical prosthesis leading to urgent surgical conversion. Finally, aortic valve replacement was successfully performed, and the patient survived. Mortality after 30 days was highest among surgical procedures performed in the catheterisation laboratory (6/8) compared to the other locations, i.e., hybrid room (2/8) and operating theatre (3/8).
On average, patients spent 11.7 days on the intensive care unit (range 1 to 38 days), with a mean time of 144±237 minutes on the respirator.
Discussion
In the current literature, there are only sparse data on bail-out surgery during TAVI. A conversion rate of 1.0% was found in the German TAVI registry for transfemoral and 2.4% for transapical TAVI, which is well within the range of other registry data that have been published so far (Table 2)1-5.
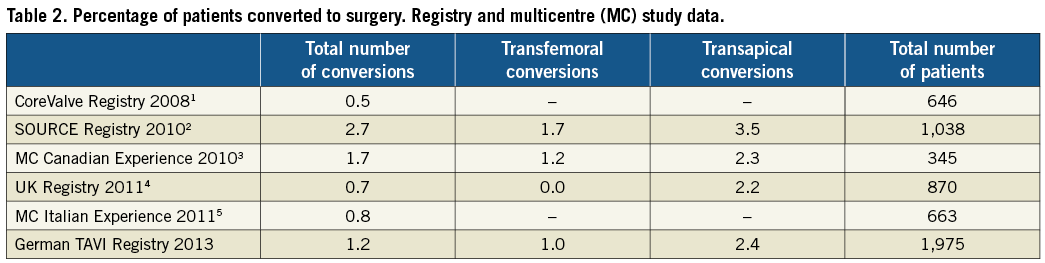
Apparently, transapical valve implantation is accompanied by a slightly higher rate of conversions compared to transfemoral procedures. It is debatable whether this might be the result of more patient comorbidities and/or a more “surgical setting” with preparations made for thoracotomy and a cardiac surgeon performing the transapical procedure as primary operator. In the current analysis, elapsed time from TAVI abortion until surgery was markedly reduced within the transapical group, as expected. Nonetheless, mortality was – with respect to patient comorbidity – about 50% after 30 days, at the same level as transfemoral procedures.
In general, evaluation of existing publications mentioning “conversion rates” is complicated by heterogeneous definitions. This makes it difficult to separate real bail-out conversions during TAVI from subacute conversions due to complications shortly after TAVI or elective periprocedural conversions (e.g., access site problems). A specific definition has recently been released in the second report from the Valve Academic Research Consortium (VARC-2)7. Additionally, all surgical aorto-valvular procedures due to complications after TAVI might be termed early (<30 days), late (>30 days and <12 months), or very late (>12 months) surgical (re-)operations, analogous to, e.g., the ARC definitions for stent thrombosis8.
CAUSES FOR CONVERSION
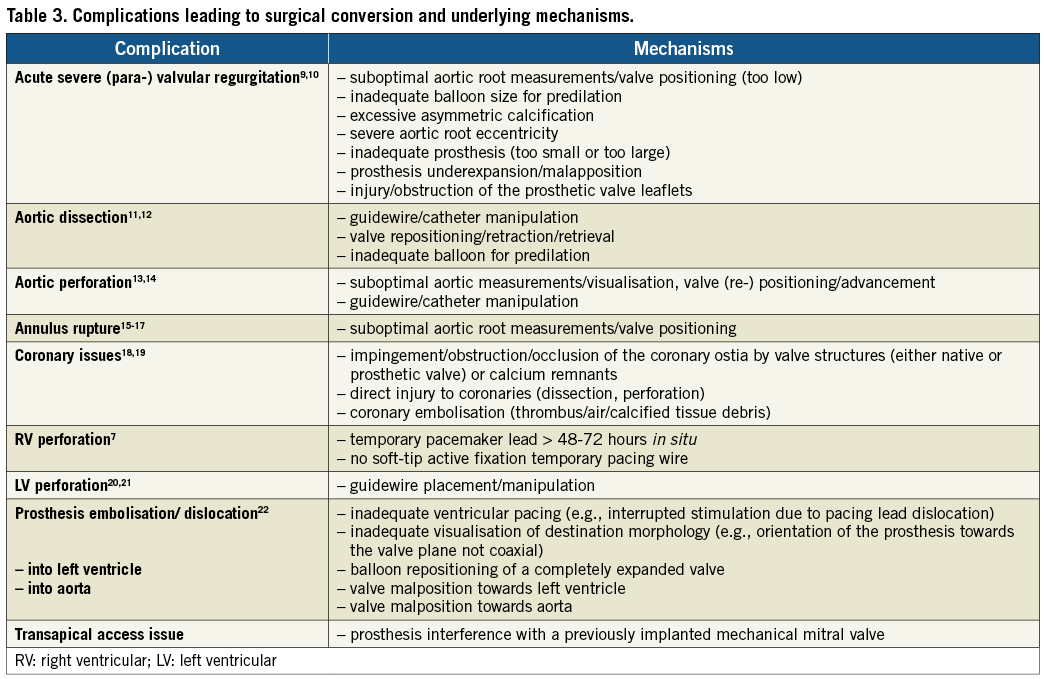
Recognising complications necessitating bail-out surgery during TAVI is of utmost importance for immediate reaction if they occur. Table 3 summarises the current literature and the authors’ experience on causes and mechanisms for emergency surgical conversion.
ACUTE RESULTS AFTER SURGICAL CONVERSION
Though the number of patients observed was small, some compelling findings may be noted. First, immediate (within 72 hours after surgery) procedural mortality was not as high as one would have expected (29.2%, 7/24). Second, aortic perforation and aortic dissection were high mortality events, as expected. Third, annulus rupture is not necessarily a high mortality event (one patient died during surgery, one patient survived, one patient died due to a non-cardiac reason two weeks after surgery), potentially as a result of the short time interval between abortion of TAVI until surgery (five to 10 minutes) and absence of transportation time (hybrid room in both survivors of the acute phase). Fourth, severe regurgitation and coronary issues were successfully treated surgically with favourable immediate patient outcome (0% mortality) and acceptable outcome after 30 days (one patient sustained a sudden cardiac death). Fifth, outcome after surgical intervention for myocardial perforation and valve embolisation was moderate to poor (50% and 40% mortality at 30 days, respectively).
PROCEDURAL SETTING
Recently, reports on successful non-surgical management of acute aortic regurgitation, aortic dissection, coronary issues, and prosthesis embolisation have also accumulated. Some examples are the valve-in-valve concept for treatment of severe regurgitation/dissection, withdrawal of the valve to a segment of the aorta with a similar diameter in case of embolisation (alternatively stent deployment within the valve), or periprocedural catheterisation of the coronary ostia combined with ostial stenting in case of valve overlap23,24. With growing experience, these rescue strategies will undoubtedly further improve patient outcome in the near future. This expectation and the low rate of bail-out conversions today (around 1 to 2%) raise the question as to whether the availability of on-site heart surgery is mandatory for all cases, for example in patients with absolute contraindication to (re-)operation (e.g., internal mammary artery graft crossing the midline of the sternum, or severe adhesions due to multiple reoperations, or heavy circumferential calcification of the aorta precluding cross-clamping). Nonetheless, the overall acceptable (except for patients with aortic perforation and dissection) outcome of some high surgical risk patients in the current analysis not only supports the presence of an on-site cardiac surgeon (as requested by current guidelines on valvular heart disease), but also seems to be a strong incentive for the implementation of hybrid rooms which offer the highest level of safety for TAVI as standard25.
Putting the above-mentioned findings into context with a very recently published meta-analysis on TAVI conversions, several findings may be noted26. First, a unifying definition for “conversion to surgery” was not provided. This might have led to inclusion of non-emergent conversions (found in two of the patients within the German TAVI registry retrospectively). Second, conversion rates for both transarterial and transapical procedures were slightly lower in the meta-analysis (1.9±1.7% for transarterial vs. 0.6±0.9% for transapical procedures). Missing data in 14% of the total patient collective have to be acknowledged. Third, the most frequent cause for conversion was prosthesis embolisation in that meta-analysis, whereas aorto-valvular complications (i.e., combination of aortic annulus rupture, aortic perforation, or thoracic aortic dissection) were the leading causes for conversion in the German TAVI registry. In the current analysis, it was decided to summarise all aorto-valvular complications due to potential complication overlap, e.g., aortic dissection leading to aortic rupture. Fourth, average mortality of converted patients was considerably higher in the meta-analysis (67.1%), taking a standard deviation of ±37.9% into account. Potential reasons for that might be site or operator-dependent. The timely decision to convert a patient to surgery might be a further reason in addition to institute-specific experience, spatial requirements, patient comorbidity, etc.
Limitations
Although registry data are susceptible to selection bias, which might mask the actual proportion of conversions and distort patient outcome, they are currently the only available source of information since data from randomised controlled trials on this issue are missing. Although the German Transcatheter Aortic Valve Interventions Registry is – except for follow-up calls – a non-monitored registry, information used in this article has been assured and relevant additional data have been gained from the above-mentioned questionnaire.
Conclusions
Emergency conversion from TAVI to surgery is a rare phenomenon and results in patient mortality as high as 45% after 30 days. Whilst mortality in patients with prior injury of aortic, aorto-valvular, or myocardial tissue during TAVI was high, acute aortic regurgitation and coronary complications had favourable outcomes after 30 days. The procedural and outcome data of this registry underscore both the importance of an on-site cardiac surgical team as a prerequisite for TAVI, and constant process optimisation efforts regarding such emergency scenarios. In order to prevent surgical conversion, recognition of potential TAVI-associated complications and knowledge of their underlying mechanisms are mandatory for interpretation of preprocedural and periprocedural imaging and immediate decision making regarding specific treatment modalities.
Conflict of interest statement
The authors have no conflicts of interest to declare.