Introduction
Following the pioneering work by Alain Cribier1, Germany has been leading the clinical adoption of transcatheter aortic valve implantation (TAVI) in Europe2 and worldwide. Since 2008, all surgical aortic valve replacements (SAVR) and all TAVI procedures are registered within a nationwide quality assurance programme providing unique insights into the development of the treatment of aortic valve stenosis since the advent of TAVI. This short report updates our previous summary (2008-2014) of the annual quality reports until 20173.
Methods
The design of the German Quality Assurance Programme on Aortic Valve Replacement has been described previously3. Most importantly, participation is mandatory for all sites performing TAVI and/or SAVR procedures. Official quality reports are published annually in the German language and are freely accessible online4.
Results
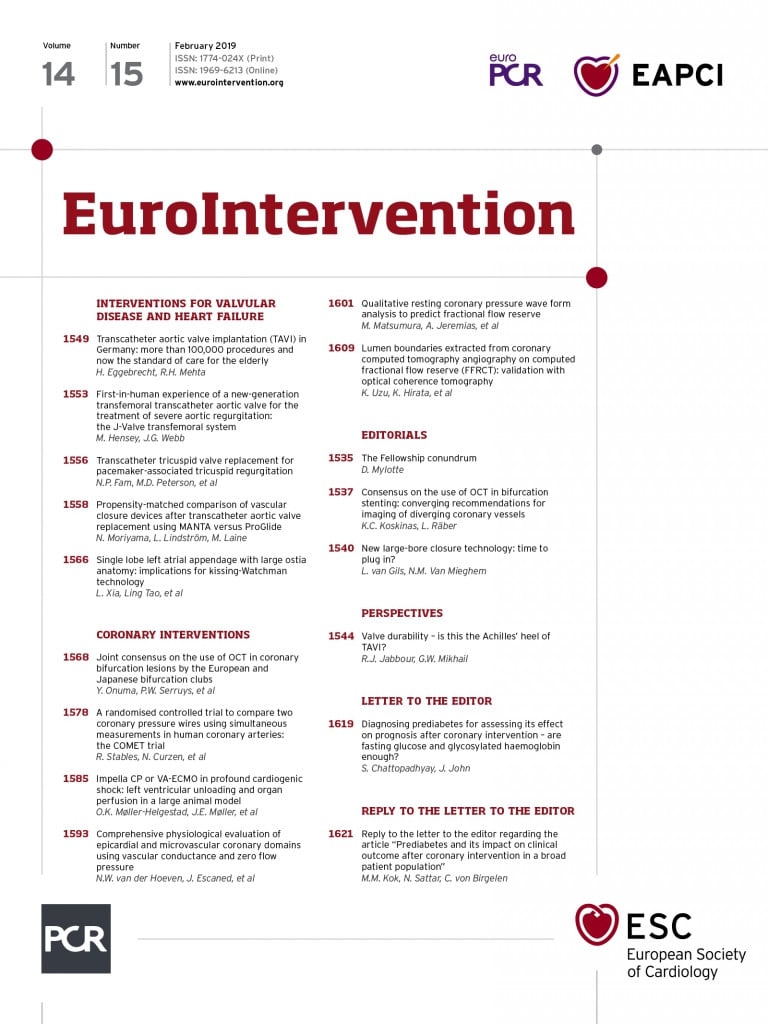
Since 2008, a total of 100,817 TAVI and 166,643 SAVR procedures have been performed in Germany. The rapid increase in annual TAVI procedures seen between 2008 and 2014 has continued (Figure 1). In 2017, a total of 19,752 TAVI procedures were performed, representing a thirtyfold increase compared with 2008 (n=637) and an almost 50% increase compared with 2014 (n=13,246). The vast majority (2017: 91%) of TAVI procedures were performed via the endovascular route, while the proportion of transapical TAVI procedures is constantly decreasing (2011: 37%; 2017: 9%) (Supplementary Figure 1). The main increase in annual TAVI procedures has resulted from increasing numbers of very elderly patients >80 years undergoing this procedure (Supplementary Figure 2). In contrast, annual numbers of SAVR have declined by 23% since 2008 (isolated SAVR: 11,205 in 2008 to 9,011 in 2017; SAVR plus coronary artery bypass grafting [CABG]: 7,706 to 5,539) (Figure 1).
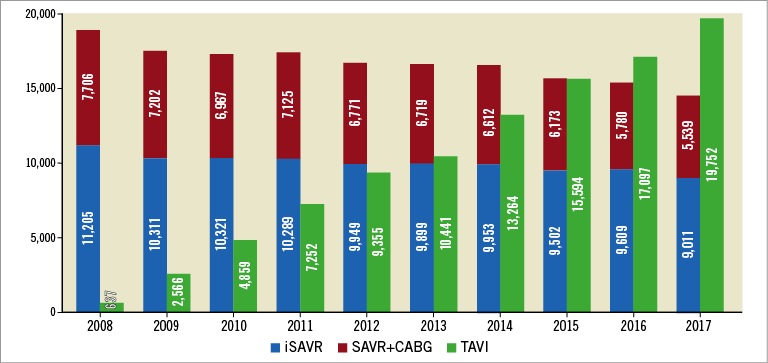
Figure 1. Annual procedure numbers for TAVI, isolated SAVR and SAVR plus CABG in Germany between 2008 and 2017.
While the mean age of TAVI patients has remained stable over time (81.0 years, 50.4% female), the mean age of patients undergoing isolated SAVR has declined from 69.8 years in 2008 and 68.5 years in 2014 to 67.2 years in 2017. Older age was the most frequent reason for the local Heart Team to select TAVI over SAVR (2017: 75% versus 2014: 70%). In fact, 12,851 of 13,532 (95%) patients aged >80 years subjected to invasive treatment for aortic valve stenosis underwent TAVI (Figure 2). In the age group 90+, only four patients in the whole of Germany underwent SAVR, while 1,067 received TAVI (99.6%).
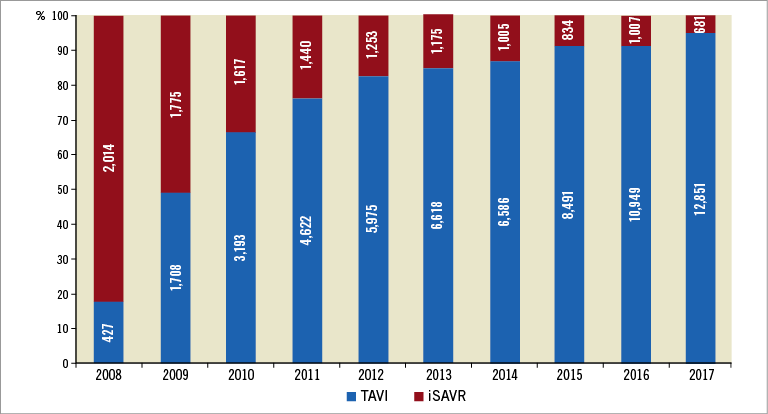
Figure 2. Proportions of patients aged >80 years undergoing TAVI or isolated SAVR between 2008 and 2017.
At baseline, TAVI patients still had more comorbidities than SAVR patients (Supplementary Table 1). However, among TAVI patients the proportion of high-risk (logistic EuroSCORE I >20%) patients has been constantly diminishing over time (2011: 46%, 2014: 36%; 2017: 35%) towards more lower-risk (EuroSCORE ≤10%) patients (2011: 19%; 2014: 26%, 2017: 29%) (Supplementary Figure 3). The clinical estimation of patient risk – in combination with age – appears to become more important for selection of TAVI versus SAVR. After age, frailty was the second most important reason to select the less invasive treatment (2017: 58%). Interestingly, one third of patients wished to be treated with TAVI (2017: 31% versus 2011: 20% versus 2014: 28%).
In-hospital mortality rates after TAVI declined considerably over time (2017: 3.1% versus 10.4% in 2008 and 4.2% in 2014) almost to match (despite older age and higher risk profiles) the observed mortality after isolated SAVR (2017: 2.7%) (Figure 3). Patient status at 30 days was reported for 79% of SAVR patients and 72% of TAVI patients. Mortality at 30 days was 3.05% for SAVR patients and 3.49% for TAVI patients with known status. Endovascular TAVI was associated with lower mortality than transapical TAVI (2017: 2.7% vs. 6.1%). In-hospital stroke rates (relevant neurological deficit lasting >24 hours, Rankin score ≥2) were comparable between TAVI (2017: 0.7%) and SAVR (2017: isolated SAVR: 0.7%; SAVR+CABG: 1.3%), despite lower comorbidities in SAVR patients (Supplementary Figure 4). Severe intraprocedural TAVI complications such as annular rupture (2017: 0.20%), aortic dissection (0.12%) or coronary occlusion (0.17%) remained rare (Supplementary Figure 5). The need for conversion to sternotomy during TAVI declined to become increasingly rare (1.2% in 2013 versus 0.48% in 2017). Rates of new pacemaker implantation also decreased over time (14.9%, 12.8% and 9.2% in 2008, 2014 and 2017, respectively). Nonetheless, this complication rate in 2017 still remained about threefold higher compared with that for isolated SAVR (2.7%).
Figure 3. Trends of in-hospital mortality (%) after TAVI, isolated SAVR and SAVR plus CABG over time.
Two thirds of patients after TAVI were discharged directly home compared with less than half after SAVR (65% vs. 43%). After isolated SAVR, more patients were transferred to another hospital (21% vs. 15% after TAVI) for additional treatment or to a rehabilitation unit (31% vs. 14% after TAVI).
Discussion
Since its introduction into contemporary clinical practice, >100,000 TAVI procedures have been performed in Germany. The thirtyfold increase in annual TAVI numbers has been driven mainly by more elderly patients undergoing this procedure. In fact, TAVI has become the standard of care and preferred procedure for patients >80 years, with 95% of patients undergoing invasive treatment for aortic valve stenosis receiving TAVI. The average age of TAVI patients has remained constant at 81 years, while risk profiles have decreased towards more lower-risk patients. The increased trend in the use of TAVI was also associated with more favourable trends in the in-hospital mortality and complications of patients undergoing this procedure. The improvement in technology and experience along with robust evidence from clinical trials and registries has certainly contributed to the growing enthusiasm for its use and better outcomes in patients undergoing this procedure. As technology evolves further and more data in lower-risk patients (particularly longer-term outcomes data) become available, it remains to be seen whether TAVI will become the preferred procedure for all patients irrespective of their age or risk, reserving SAVR for a minority (as observed currently for those over 80 years) in future.
Limitations
The data from this nationwide Quality Assurance Registry are restricted to the in-hospital period, while midterm follow-up is lacking. All events are self-reported by the sites and not adjudicated. Within the registry outcomes are not differentiated for different TAVI valve types.
Conclusion
With more than 100,000 procedures performed, TAVI has become the standard of care for elderly patients >80 years.
| Impact on daily practice Transcatheter aortic valve implantation (TAVI) has become the standard of care and preferred treatment for elderly patients with symptomatic aortic valve stenosis. Age >80 years appears to be the most important reason to select TAVI over conventional surgery. Improvements in techniques and patient selection have resulted in a dramatic reduction of in-hospital mortality, which is now very similar to that after isolated surgery of the aortic valve. |
Conflict of interest statement
The authors have no conflicts of interest to declare with regard to the subject matter of this article.
Supplementary data
Supplementary Figure 1. Distribution of endovascular versus transapical TAVI over time.
Supplementary Figure 2. Trends in annual procedure volumes for TAVI and isolated TAVI stratified by patient age group.
Supplementary Figure 3. Trends in distribution of logistic EuroSCORE I of TAVI patients between 2011 and 2017.
Supplementary Figure 4. Trends in clinical stroke rates (%) for TAVI and SAVR over time.
Supplementary Figure 5. Rates of severe intraprocedural TAVI complications and need for sternotomy over time.
Supplementary Table 1. Baseline characteristics of patients undergoing TAVI or SAVR in Germany in 2017 versus 2014.
To read the full content of this article, please download the PDF.