
Abstract
Aims: In Germany, all transcatheter aortic valve implantations (TAVI) and surgical aortic valve replacements (sAVR) are registered within an obligatory quality assurance programme led by the independent AQUA Institute. We have summarised patient and procedural characteristics, complication and mortality rates as reported in the annual, German language AQUA quality reports, freely accessible online, in order to provide a comprehensive overview of developments between 2008 and 2014.
Methods and results: Since 2008, a total of 71,927 isolated sAVR and 48,353 TAVI procedures have been performed in Germany. The numbers of sAVR are steadily declining (2008: 11,205; 2014: 9,953). For TAVI, there has been a 20-fold increase since 2008, from 637 to 13,264 procedures in 2014, surpassing the annual numbers of isolated sAVR since 2013. The age profile of TAVI patients has remained unchanged over time (mean age: 80.9 years), with a recent trend towards lower-risk/intermediate-risk patients. TAVI complications are rapidly decreasing (2012: 9.4%; 2014: 3.9%); annular rupture, aortic dissection and coronary occlusions are rare (<0.3%), with fewer patients requiring surgical conversion to sternotomy (2012: 1.2%; 2014: 0.6%). In-hospital mortality after TAVI has halved in 2014 (4.2%) compared with 2008 (10.4%).
Conclusions: Real-world clinical data from the obligatory quality assurance programme document the rapid adoption of TAVI in Germany, shifting treatment of aortic valve stenosis in the elderly from surgery to a catheter-based approach. Since 2008, similar to what happened with PCIs, complications of TAVI have declined considerably along with the need for emergency cardiac surgery. Most importantly, in-hospital mortality has halved from 2008 to 2014, while mortality for sAVR has remained unchanged.
Introduction
In Germany, all surgical aortic valve replacements (sAVR) and transcatheter aortic valve implantation (TAVI) procedures are registered by the independent Institute for Applied Quality Improvement and Research in Health Care (AQUA, Göttingen, Germany), according to the statutory external quality assurance programme1,2. Participation is mandatory for all hospitals and is linked to reimbursement1. All events are defined in an elaborate form completion guide3 and self-adjudicated by the sites. All data are reported by the sites using standardised electronic data entry with no on-site monitoring. Data are pooled in a nationwide database. In case of inconsistencies or deviations from predefined quality benchmarks, a structured dialogue with the specific centre is initiated to trigger individual institution designed quality improvement measures2. Analyses of patient and procedure characteristics, including complications, in-hospital and 30-day mortality, are published in an annual, German language quality report, freely accessible online4.
Since rates of TAVI for the treatment of aortic stenosis worldwide are highest in Germany5 and clinical experience with this procedure is still sparse in many countries, we believe that these publicly available real-world quality assurance data may provide useful information for physicians involved in TAVI around the globe. Accordingly, we have summarised the official annual AQUA reports to provide a comprehensive overview of the development of TAVI relative to the standard surgical aortic valve replacement (sAVR) with respect to patient and procedural characteristics, and complication and mortality rates in Germany between 2008 and 20146-8. Due to the differences in baseline characteristics between the groups, no statistical analysis was performed.
Results
The AQUA reports show that the annual number of isolated sAVR procedures has declined, from 11,205 in 2008 (mean age: 69.8 years; 56.3% males) to 9,953 in 2014 (mean age: 68.5 years; 60.5% males)9,10. A similar trend was observed for combined sAVR plus coronary artery bypass grafting (CABG) (Figure 1). In contrast, TAVI procedures have increased 20-fold, from 637 in 2008 (mean age: 81.6 years; 39.5% males) to 13,264 in 2014 (mean age: 80.9 years; 47.6% males), and have surpassed the annual numbers of isolated sAVR since 2013 (Figure 1)11,12. While the number of transapical TAVI has been relatively constant, the main increase in overall TAVI numbers is related to the increase in endovascular (transfemoral) TAVI (2011: 4,567; 2014: 10,282) (Online Figure 1)12.
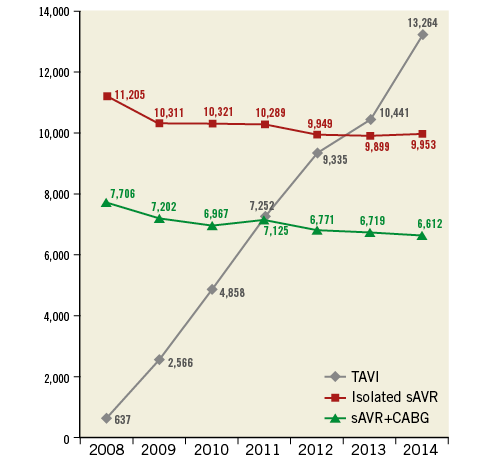
Figure 1. Trends in TAVI, isolated sAVR and sAVR plus CABG in Germany between 2008 and 2014.
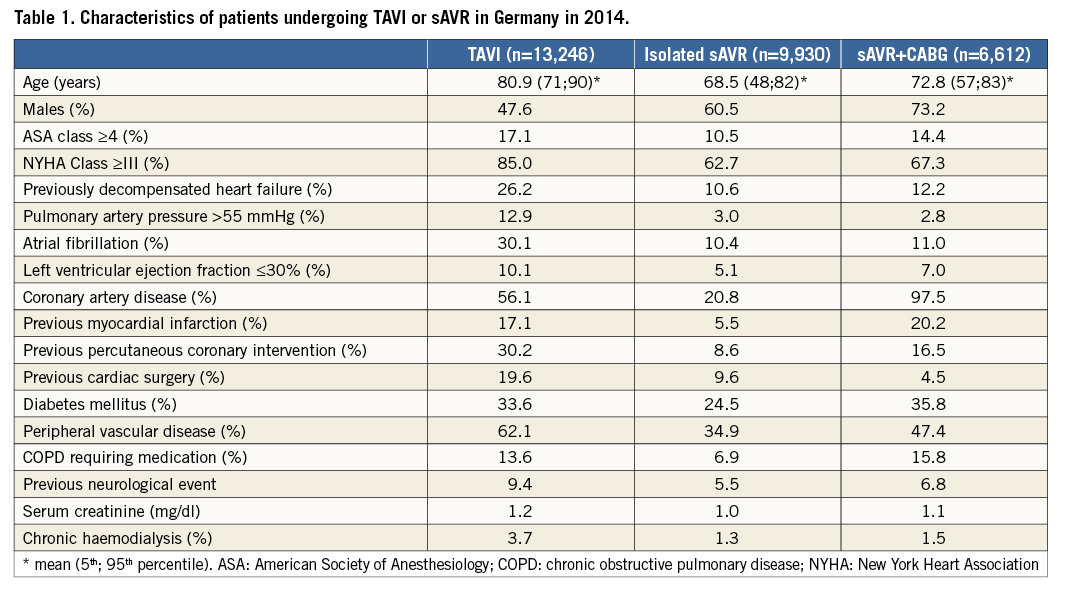
As expected, TAVI patients were older and had more comorbidities than patients undergoing sAVR (Table 1). In 2014, 77.2% of all patients undergoing TAVI in Germany were >75 years and had a logistic EuroSCORE >20%, or had contraindications (porcelain aorta, severe frailty, patient wish, advanced cancer or other prognosis-limiting comorbidities) against sAVR (2013: 74.8%)12. Age distribution of TAVI patients has remained unchanged since 2008: >95% of TAVI patients were 70 years or older (Online Figure 2). For sAVR, there has been a trend towards younger patients undergoing this procedure, from 62.2% being >70 years in 2009 to 56.8% in 2014 (Online Figure 2). With respect to the logistic EuroSCORE, there has been a recent trend towards TAVI being performed in lower-risk/intermediate-risk patients (Online Figure 3). Older age was the most frequent reason for the local Heart Team to for select TAVI over sAVR (2014: 70.2% versus 2013: 63.8%). Additionally, high-risk procedure, as defined by a logistic EuroSCORE >20% or STS score >10%, patients’ wish (2013: 20.6%; 2014: 27.6%) and frailty (2013: 42.9%; 2014: 46.5%), have evolved as increasingly important reasons for selecting TAVI (Online Figure 4)12.
Intraprocedural complications during TAVI have declined from 9.4% in 2012 to 3.9% in 2014 (Table 2)11-13. Severe TAVI complications such as annular rupture, aortic dissection or coronary occlusion occurred in <0.3% of patients (Online Figure 5)12. The rate of conversion to sternotomy during TAVI has declined from 1.2% in 2012 to 0.6% in 2014 (Online Figure 5, Table 2)12.
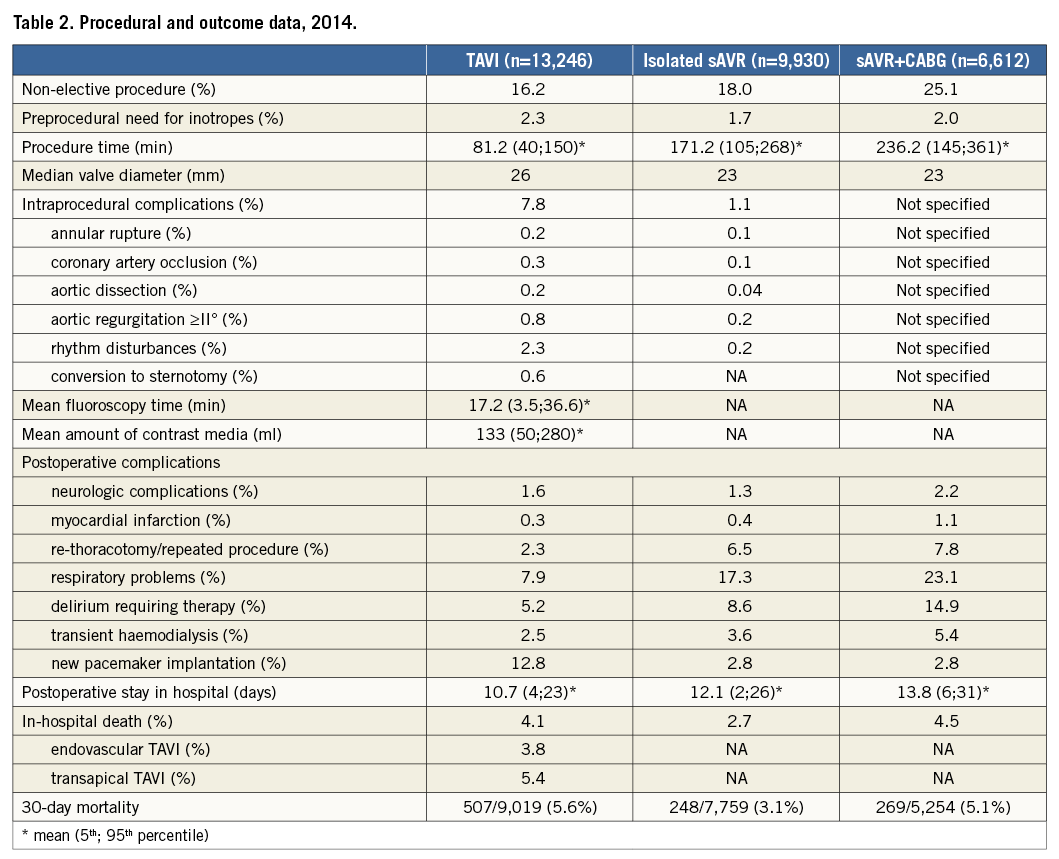
Similarly, vascular complications have declined from 8.5% in 2013 to 6.5% in 201412. In-hospital stroke rates (relevant neurological deficit lasting >24 hours, Rankin score ≥2) were comparable between TAVI (2014: 1.4%) and sAVR (2014: isolated sAVR: 1.1%; sAVR+CABG: 2.0%), despite differences in baseline characteristics (Figure 2)11-13. Rates of new pacemaker implantation have remained relatively stable over time: 14.9% in 2008 and 12.8% more recently (Online Figure 6). The need for dialysis after TAVI has decreased considerably from 8.3% in 2008 to 2.6% in 2014, eventually to fall below the rates of dialysis after sAVR (isolated sAVR: 3.6%; sAVR+CABG: 5.4%) (Online Figure 7)11-13.
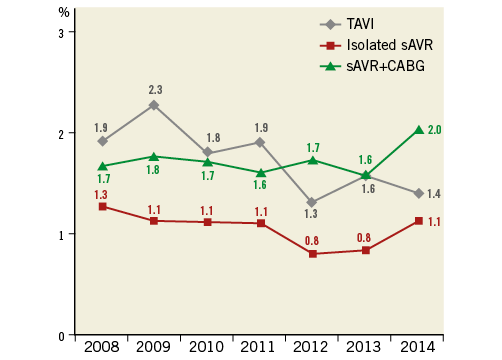
Figure 2. Trends in neurologic complications after TAVI, isolated sAVR and sAVR plus CABG over time.
Most importantly, in-hospital mortality after TAVI declined from 10.4% in 2008 to 4.2% in 2014 (Figure 3)10-12. As expected, patients in the lowest risk group had the lowest 30-day mortality rate of only 2.0%12. Mortality was lower among those undergoing endovascular TAVI versus transapical TAVI, showing a decline for both over time (Table 2, Online Figure 8). Mortality of patients undergoing sAVR+CABG has remained consistently higher compared with isolated sAVR over time (2014: 4.5% and 2.7%, respectively), and –although much lower in 2008– similar to that of TAVI in recent years9,10. Length of in-hospital stay has remained unchanged for sAVR, but decreased for TAVI over time (Online Figure 9).
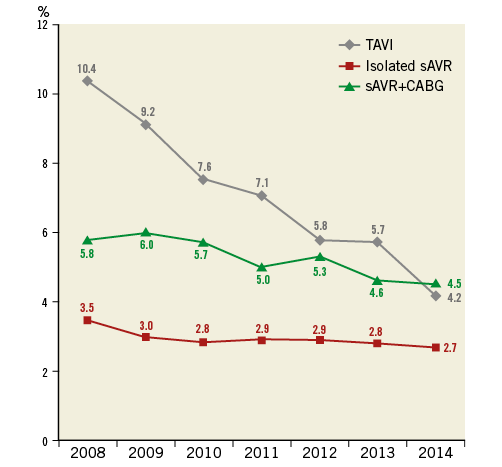
Figure 3. Trends in unadjusted in-hospital mortality rates after TAVI, isolated sAVR and sAVR plus CABG.
Conclusions
In conclusion, TAVI has overtaken sAVR for the treatment of aortic valve stenosis in Germany. Despite dramatically increasing annual TAVI numbers (>20-fold since 2008), the age profile of TAVI patients has remained unchanged. Recent data suggest a trend towards lower-risk/intermediate-risk patients as a result of an increasing desire among patients to have TAVI instead of sAVR. Importantly, complication rates of TAVI are rapidly declining and are comparable (for stroke) or even better (need for dialysis) than sAVR, despite the older age and higher comorbidities of TAVI patients relative to the sAVR cohort (TAVI: 12.4 years older). Severe TAVI-specific complications (e.g., annular rupture) are becoming rarer (<0.3%), with fewer patients (0.6%) requiring emergency cardiac surgery. Even more impressive is the rapid decline in the in-hospital mortality after TAVI which has halved in 2014 as compared to 2008 (closing in on that of lower-risk patients undergoing sAVR). This increase in volume and its related decline in procedural complications and mortality can be attributed to a multitude of factors that include improvement in technology, operator experience and the growing number of patients with low/intermediate risk undergoing TAVI. Future registry efforts need to be directed at following patients long term after TAVI to provide valuable insights into the association with long-term patient morbidity and mortality, quality of life and the cost of this shift from sAVR to TAVI in Germany.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
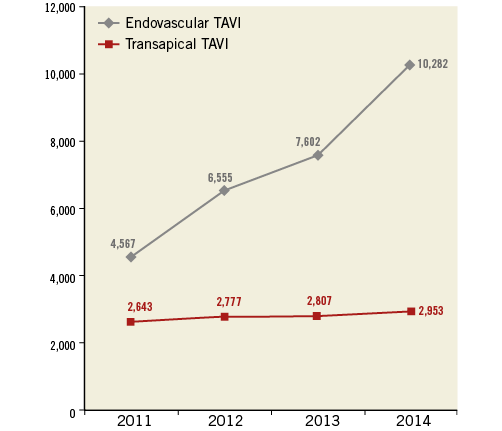
Online Figure 1. Distribution of endovascular versus transapical TAVI over time.
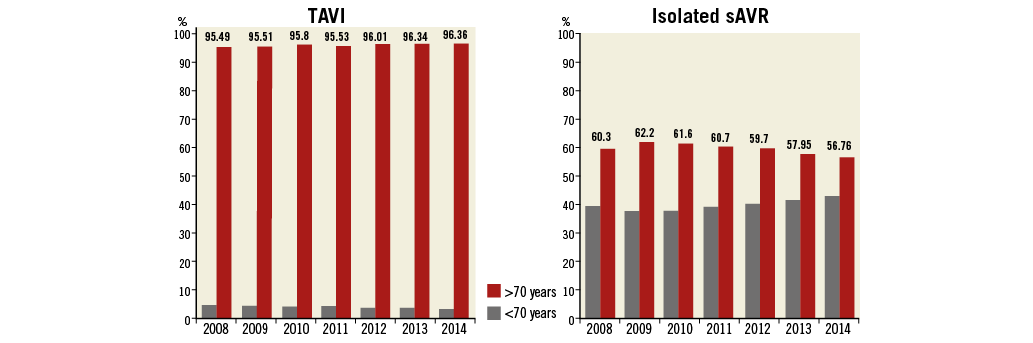
Online Figure 2. Age distributions among patients undergoing TAVI or isolated sAVR.
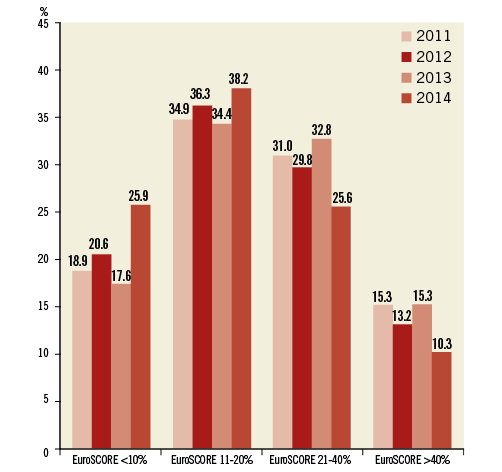
Online Figure 3. Trends in logistic EuroSCORE of TAVI patients between 2012 and 2014.
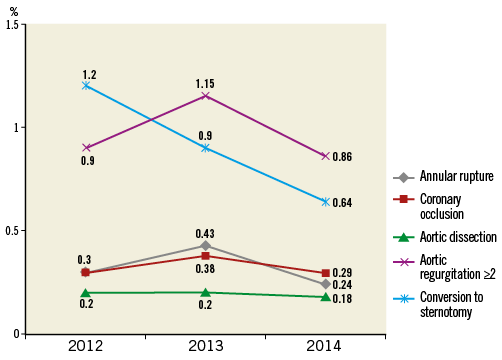
Online Figure 5. Rates of severe intraprocedural complications and need for sternotomy after TAVI over time.
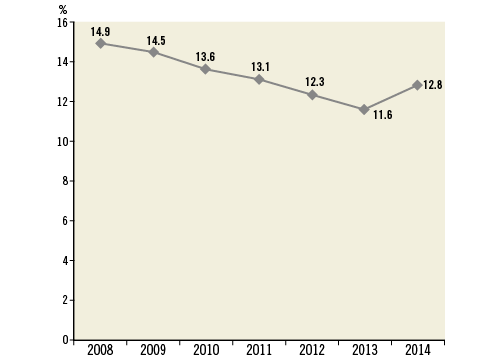
Online Figure 6. Rates of new pacemaker implantation after TAVI over time.
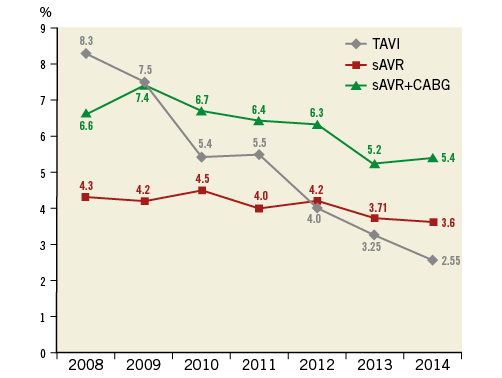
Online Figure 7. Rates of need for dialysis after TAVI, isolated sAVR and sAVR plus CABG over time.
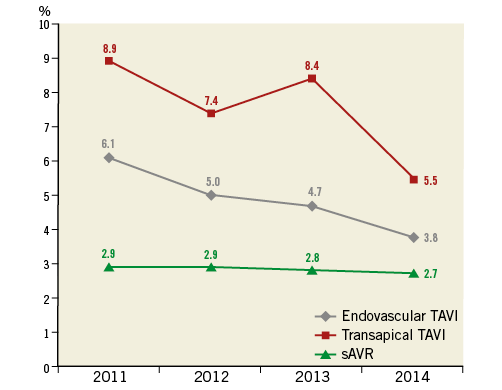
Online Figure 8. Unadjusted mortality rates after endovascular TAVI, transapical TAVI and isolated sAVR over time.
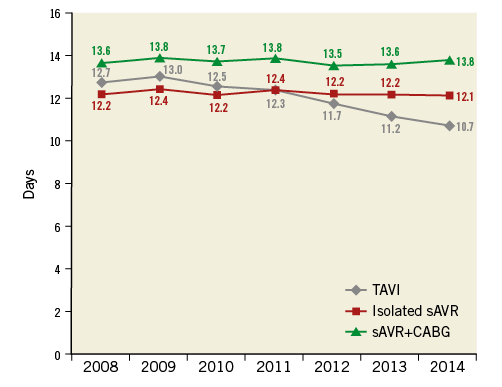
Online Figure 9. Mean in-hospital stay after TAVI, isolated sAVR and sAVR plus CABG over time.

