Transcatheter aortic valve implantation (TAVI) has not been around as long as golf but is already the standard of care for patients with severe aortic stenosis at high surgical risk and is at least as good as surgical aortic valve replacement (SAVR) in lower-risk groups. TAVI procedural volume now exceeds that of SAVR in many centres. Further expansion seems inevitable in response to patient preference and as ongoing trials and improved devices emerge. All procedures have a learning curve, with data from the United States Transcatheter Valve Therapy (TVT) registry showing that TAVI complication rates are significantly higher in the first 100 procedures and that they fall with increasing experience1. While this information clearly demonstrates the operator learning curve associated with all complex procedures, the more politically charged question concerning the institutional volume required to achieve optimal clinical outcomes remains unexplored. Unlike golf, TAVI is a team sport, with multiple factors responsible for overall success.
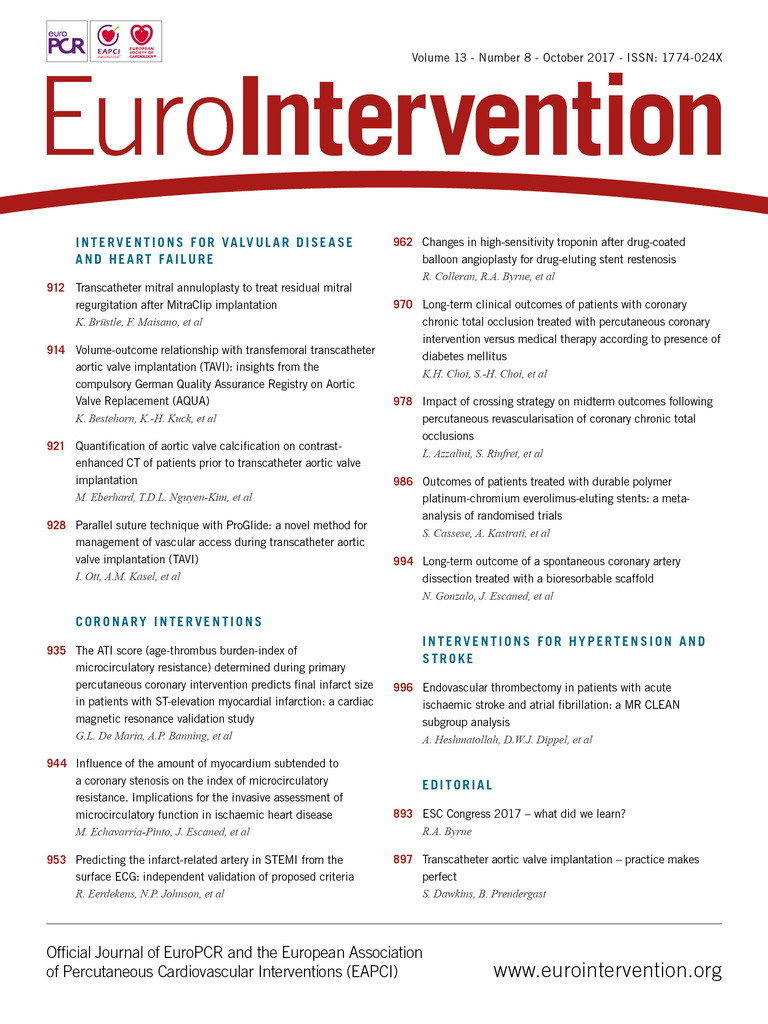
In this issue of EuroIntervention, Bestehorn et al2 present volume-outcome analysis of all non-emergency transfemoral TAVI procedures performed in Germany in 2014 using the resources of the national Quality Assurance Registry (AQUA), which mandates collection of procedural and outcome data concerning all TAVI and SAVR procedures.
After exclusion of hospitals performing ≤10 procedures (10 hospitals, 45 TAVI procedures) and 330 patients who underwent emergency procedures, the analysis included 9,924 patients undergoing TAVI at 87 hospitals – 46 (53%) hospitals performed ≥100 (average 171, range 102-415) procedures per year (80% of national volume) and <100 (average 51, range 11-92) procedures per year were performed in the remainder.
The observed in-hospital mortality across the entire cohort was 4.3%, and significantly higher in low-volume (<50 procedures/year) than high-volume (≥200 procedures) hospitals (5.6 vs. 2.4%, p<0.001). This difference remained significant after adjustment for baseline patient characteristics, with a lower observed to expected mortality ratio – derived using the German Aortic Valve Score (2.0) – in high-volume centres3. Rates of emergency cardiac surgery, stroke and vascular complications did not differ according to hospital procedural volume although procedural time and length of stay were longer in low-volume centres.
National registries provide a rich source of information which is complementary to that provided by randomised controlled trials, and are particularly valuable when hard endpoints such as mortality are used, since these are recorded with a high degree of accuracy. The lack of on-site adjudication confers a risk of underreporting of clinical events (especially minor procedural complications), and exclusion of emergency and non-femoral TAVI procedures in the present analysis might, if anything, have diluted the striking volume-outcome relationship.
The cardiac surgical literature has already clearly demonstrated an inverse relationship between institutional and individual operator volume and outcomes following SAVR and mitral valve repair4-11. As the use of TAVI expands worldwide to new centres and lower-risk patients, it is vital that the excellent outcomes obtained to date in specialist centres are maintained, and that minimum procedural numbers are defined by national and international specialist societies. The authors of the present study have demonstrated a near-linear relationship between procedural volume and outcome, with most variability in outcome occurring in centres performing fewer than 100 TAVIs per year. Although outcomes were good in many lower-volume centres, variability in outcome was much greater in this setting, consistent with previous studies12,13. Individual operator and hospital volumes are unlikely to be perfect surrogates for outcome data and the ability to demonstrate good results is more important than working to volume targets. Nevertheless, institutional volumes of >50 TAVI procedures/year are recommended in France and the UK (>75 procedures/year in the Netherlands), and a robust approach to minimum volume recommendations has been encouraged in a recent position statement concerning the standards required for designated “Heart Valve Centres”14. Similar standards are currently under consideration in the United States.
The ProGlide® suture (Abbott Vascular, Santa Clara, CA, USA) is a percutaneous vascular closure device widely used for patients undergoing TAVI15. The standard method of deployment uses two devices placed at 10 and 2 o’clock prior to sheath delivery and is effective at closing the femoral arterial puncture site. In this issue of EuroIntervention, Ott et al16 present a novel “parallel suture technique” using two sutures deployed parallel to the vessel by moving the ProGlide first medial then lateral (rather than using a rotational movement).
Retrospective analysis demonstrated a higher rate of unplanned endovascular intervention (4% vs. 15%, p=0.02) and major bleeding (13% vs. 3%, p=0.009) in the 100 patients undergoing SAPIEN XT implantation compared with the 100 patients receiving the SAPIEN S3 device (both Edwards Lifesciences, Irvine, CA, USA) – unsurprising given that a larger sheath is required for the XT valve. They also reported a lower rate of VARC-2 major vascular complications compared with the results of a recently published meta-analysis17. The major weakness of this study is the lack of a direct control group; however, the results are promising and the technique warrants further evaluation.
The degree of aortic valve calcification measured using non-enhanced computed tomography correlates strongly with the severity of aortic stenosis and is an independent risk factor for poor TAVI outcome18. Patients undergoing TAVI usually undergo contrast-enhanced CT as an integral component of procedural planning, and measurement of AVC is not currently validated using contrast-enhanced scans. In this issue, Eberhard et al19 describe a technique to determine the degree of aortic valve calcification from a contrast-enhanced CT scan with high levels of accuracy, using a formula developed in training and validation cohorts of patients undergoing both modalities of CT imaging (correlation coefficient 0.897, p<0.001).
This elegant technique could help to reduce the number of CT scans required by TAVI patients, with associated reduction in radiation exposure and overall cost. Several TAVI trials for patients with asymptomatic aortic stenosis are underway – if positive, this technique could prove useful in identifying asymptomatic patients at highest risk who may benefit most from pre-emptive TAVI.
So, TAVI is set for worldwide expansion. Adequate institutional procedural numbers, careful technique to reduce complications and detailed preprocedural planning will be vital to ensure that the excellent results to date are maintained and provide a new par for the course.
Conflict of interest statement
The authors have no conflicts of interest to declare.