Transcatheter aortic valve replacement (TAVR) has been shown to be non-inferior to surgical aortic valve replacement (SAVR) in multiple randomised trials in high- and intermediate-risk patients1-5. Most patients studied in these randomised trials were elderly, being for the most part in their late seventies and early eighties in age. Two trials in lower-risk patients which have recently completed enrolment in the USA presumably include younger patients. However, the results of those trials will not be available until mid 2019.
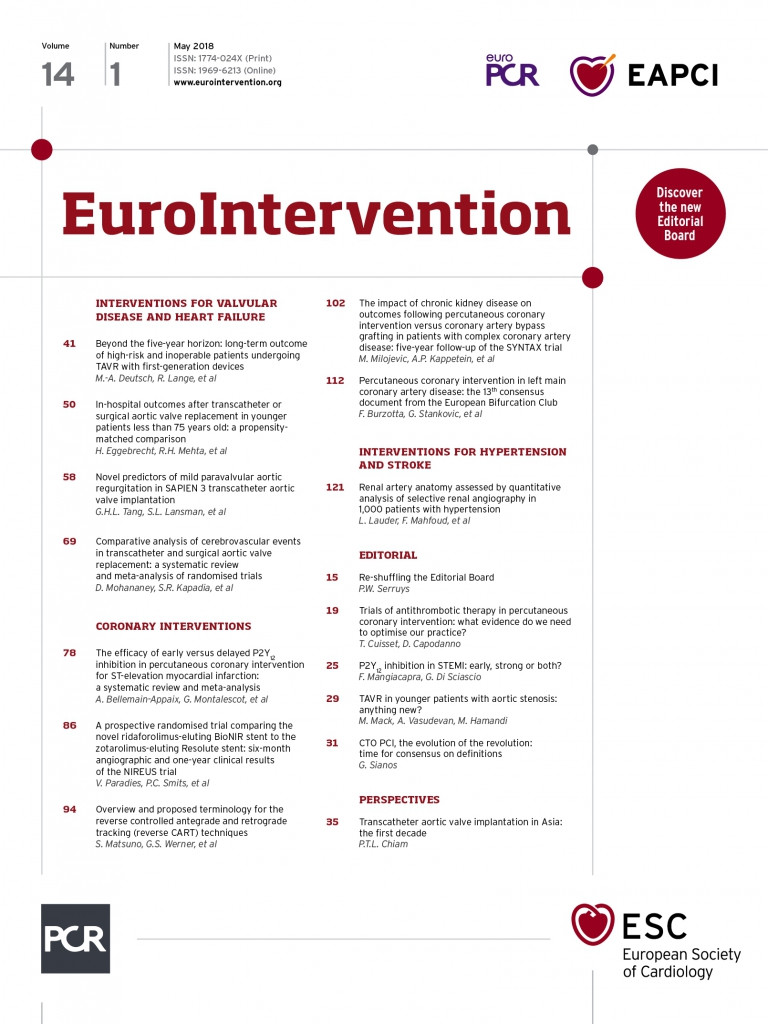
In this issue of EuroIntervention, Eggebrecht and colleagues have attempted to shed some light on the outcomes of TAVR compared with SAVR in younger patients prior to the availability of those trial reports6.
The investigators queried an administrative claims database in Germany, the Applied Quality Improvement and Research in Health Care (AQUA), now replaced by the Federal Institute for Quality and Transparency in Health Care (IQTIG), to determine in-hospital outcomes of TAVR and SAVR in patients between the ages of 65 and 74. There were 6,970 patients in this age group treated in the years 2013 and 2014 who served as the study cohort. Of the patients treated, 5,708 (82.4%) underwent SAVR with the remaining 1,268 (17.6%) undergoing TAVR. They determined that in-hospital outcomes showed a survival advantage for SAVR with a mortality of 1.3% versus 3.2% for TAVR. There was no difference in neurological outcomes but a fourfold higher need for permanent pacemaker after TAVR and a higher rate of delirium and discharge to a facility other than home with SAVR6.
Because these were different patient cohorts, the authors then performed propensity matching of patients who underwent transfemoral (TF) TAVR to patients receiving SAVR using the components of the EuroSCORE II. They were able to match one half of the TAVR patients (694) to an equal number of SAVR patients who represented about 12% of the surgical cohort. After matching, they found that the groups were well matched except for logistic EuroSCORE. In the matched cohorts, the in-hospital mortality was the same after both procedures, as was the incidence of stroke. There was still a higher incidence of delirium in the surgical group and a fourfold higher need for pacemaker (13.3% versus 3.5%) in patients receiving TAVR. The authors concluded that “younger patients <75 years undergoing TF-TAVR or SAVR had similar outcomes with the exception of more frequent need for new pacemaker implantation and less frequent incidence of postoperative dialysis and delirium in TF-TAVR patients”.
So, can we learn anything from this analysis that would be helpful to clinicians in managing younger patients with aortic stenosis prior to the randomised trial data due to become available? Unfortunately, there are a number of significant concerns regarding this study that render the findings fairly uninformative and cause them to be interpreted with significant caution. First, these are relatively old data, from 2013-2014, which are not really reflective of current clinical practice. Five years ago, when these patients were treated, younger patients underwent TAVR for extenuating comorbid conditions such as porcelain aorta and previous chest irradiation. Although these conditions are still treated with TAVR, they represent only a small proportion of patients under 75 currently treated with TAVR. The authors acknowledge that the study population was dated but that was the latest information that was available for analysis. However, that does not change the fact that the study population was probably different from patients treated currently and therefore the findings are not relevant to current practice.
Second, the information in the study was obtained from an administrative claims database, the AQUA registry, which is a voluntary, limited data submission made for insurance payment. There was no auditing and the only outcomes reported are in-hospital. These are insufficient outcomes data by today’s standards when reporting outcomes and performing comparative effectiveness research. There is another registry in Germany, the German Aortic Valve Registry (GARY), administered by the German Society of Cardiology and the German Society of Cardiothoracic Surgery, that captured more robust outcomes data on the same patients during that same time period. The GARY registry is audited and reports a fuller data set of clinical outcomes, including 30-day and one-year mortality rather than solely in-hospital data. One wonders why the investigators did not use this database for their study as it would have provided us with more meaningful 30-day and one-year outcomes on a more current cohort of patients.
Why is reporting 30-day outcomes rather than just in-hospital mortality and morbidity important? A significant number of procedure-related deaths occur outside the hospital but before 30 days. For this reason, surgical databases reporting outcomes of SAVR report only 30-day outcomes. It is for that same reason that randomised trials use 30-day outcomes at a minimum as endpoints. The shortcoming of reporting only in-hospital outcomes (as was done in this study) has been highlighted by recent reports from the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy (STS/ACC TVT) Registry in the USA (STS/ACC TVT Registry. Report to Stakeholder Advisory Group, Washington, DC, USA, 22 February 2018. Personal communication). In the latest reporting period, which is 2017, the in-hospital mortality after TAVR was 1.74% but the 30-day mortality was 3.05%, meaning that 43% of the procedure-related deaths occurred after discharge and therefore would not have been captured by a registry that captures only in-hospital outcomes as this study did. To illustrate the point further, data from the TVT Registry in 2014, the same time period as this study, reported an in-hospital mortality of 4.11% and 30-day mortality of 6.01%, demonstrating that 32% of the deaths are missed when in-hospital mortality only is reported. As one can clearly see, using in-hospital reported outcomes underreports true procedural mortality. We are at the stage of current practice of TAVR that a minimum of 30-day outcomes and optimally one-year outcomes are the only ones reported as being truly reflective of procedural risks.
Third, there are also concerns about how the propensity matching in this study was performed. Because these were different patient groups that were treated with TAVR and SAVR, an attempt was made to compare like patient groups more accurately using propensity matching. The study authors used the components of the EuroSCORE II when performing the match. Calculating the propensity scores using a logistic regression model utilising all the patient variables would be more appropriate than choosing only the components of EuroSCORE II. The imbalance between cases and controls for the EuroSCORE II (standardised difference of 0.787) may not have been evident if the model was constructed in the traditional way. It is important to state explicitly the type of matching employed (with or without replacement) and also the basis of choosing the caliper interval.
In summary, there is little if any new information obtained in this study that helps to inform clinical practice. The cardiology and cardiac surgery community would be better off waiting for the outcomes of randomised trials in lower-risk and presumably younger patients before changing current practice in younger patients. Despite the efforts of the study investigators, there is nothing new here to inform the clinician.
Conflict of interest statement
M. Mack is co-principal investigator of the PARTNER 3 trial and is sponsored, uncompensated, by Edwards Lifesciences. The other authors have no conflicts of interest to declare.