
Abstract
Aims: We aimed to compare the long-term outcomes of transaortic (TAo-AVR) and transfemoral (TF-AVR) transcatheter aortic valve replacement.
Methods and results: Between January 2012 and December 2015, consecutive TAo-AVR and TF-AVR cases were compared using a propensity score-matching analysis. Primary endpoints were 30-day and one-year mortality; 644 TAVR patients were included (163 TAo-AVR and 481 TF-AVR). Peripheral artery disease (31.9% vs. 5%, p<0.001) and coronary artery disease (50.0% vs. 39.3%, p=0.009) were more frequent in TAo-AVR patients. The Society of Thoracic Surgeons scores were not different (6.9% vs. 6.5%, p=0.243). Propensity matching identified 124 well-matched patient pairs. Thirty-day and one-year mortality rates were similar in the overall population of TAo-AVR and TF-AVR patients (7.3% vs 7.6%, p=0.8 and 18.4% vs. 15.8%, p=0.6, respectively), and in the matched cohort (7.3% vs. 6.5%, p=0.8 and 15.3% vs. 16.1%, p=0.8, respectively). Transaortic access was associated with higher risk of new onset of atrial fibrillation (NOAF) (24.4% vs. 9.6%, p=0.012), life-threatening bleedings (6.5% vs. 0.8%, p=0.036) and transfusion (41% vs. 16.7%, p<0.001).
Conclusions: No significant differences were observed between the respective 30-day and one-year mortality rates of TAo-AVR and TF-AVR patients. The transaortic approach thus constitutes a valid alternative to TF-AVR, but is associated with higher rates of NOAF, bleedings, and transfusion.
Abbreviations
AA: aortic aneurysm
AF: atrial fibrillation
AKI: acute kidney injury
BAV: balloon aortic valvuloplasty
BMI: body mass index
CAD: coronary artery disease
eGFR: estimated glomerular filtration rate
EuroSCORE: European System for Cardiac Operative Risk Evaluation
LVEF: left ventricular ejection fraction
LOS: length of stay
MI: myocardial infarction
NOAF: new-onset atrial fibrillation
NYHA: New York Heart Association
PAD: peripheral artery disease
STS: Society of Thoracic Surgeons
TAo-AVR: transaortic transcatheter aortic valve replacement
TF-AVR: transfemoral transcatheter aortic valve replacement
TIA: transient ischaemic attack
Introduction
Since its first use in man in 2002, transcatheter aortic valve replacement (TAVR) has been widely adopted as a treatment of aortic stenosis for patients at high and intermediate surgical risk. It is currently being studied in a low-risk population. Smaller sheath delivery systems now allow transfemoral transcatheter aortic valve replacement (TF-AVR) to be performed in the vast majority of cases. Thus, transfemoral access has been adopted as the first-line approach for TAVR in many centres. However, TF access is still considered unsafe in a small proportion of patients, especially those with small, severely calcified or tortuous arteries. Therefore, an alternative access route has to be selected for this population1,2. Historically, the most commonly performed alternative approach is transapical (TAp-AVR), associated with specific issues such as myocardial damage, bleeding or respiratory complications, and resulting in an excess risk of mortality compared with TF access3. The safety and feasibility of the transaortic approach as an alternative route has been demonstrated in several retrospective studies with good short-term outcomes and also in the multicentre and multinational ROUTE registry4-8. Limited data are available regarding direct comparison between TF-AVR and TAo-AVR in high-volume centres7. The aim of the present study was to compare the long-term outcomes of TAo-AVR versus TF-AVR. We sought to identify differences in preprocedural characteristics in order to formulate a propensity score that would include confounding factors.
Methods
STUDY DESIGN
All patients treated consecutively with TAVR from 2008 were prospectively included in our database. In order to draw a contemporary comparison of transaortic and transfemoral outcomes, we reviewed patients with symptomatic severe aortic stenosis from January 2012 to December 2015 treated with TAo-AVR and TF-AVR, performed using either Edwards balloon-expandable (SAPIEN, SAPIEN XT; Edwards Lifesciences, Irvine, CA, USA) or Medtronic self-expanding (CoreValve®, Evolut™ R; Medtronic, Minneapolis, MN, USA) prostheses. The allocation strategy for TAo-AVR versus TF-AVR and valve selection were at the discretion of our local Heart Team, according to general and anatomical considerations. Written informed consent was obtained from all patients.
PROCEDURAL DETAILS
The technical aspects of the TF approach have been largely described in previous reports9. A large majority of TF-AVR cases were performed without general anaesthesia, under conscious sedation. Closure of the femoral artery was performed using the Perclose ProGlide® closure device (Abbott Vascular, Santa Clara, CA, USA). The TAo approach was performed as previously described, using a short J-shaped manubriotomy down to the second intercostal space5. Reverse T-shaped manubriotomy was used in case of prior sternotomy. Direct aortic access was replaced by innominate artery access in May 2013. Aspirin was recommended prior to TAVR. The combined use of dual antiplatelet therapy with clopidogrel was systematic for patients with recent percutaneous coronary intervention (PCI), and was left to the discretion of the Heart Team for other patients. A bolus of heparin was administered at the beginning of the procedure to achieve an activated clotting time of 250 to 300 s. Protamine injection at the end of the procedure was routinely used in both accesses. Embolic protection devices were not used during the study period.
ENDPOINTS
Primary endpoints were 30-day and one-year mortality. Secondary endpoints were 30-day and one-year complication rates, according to the Valve Academic Research Consortium-2 definitions10.
STATISTICAL ANALYSIS
Qualitative data are presented as numbers and percentages and quantitative data as means±standard deviation or as median and interquartile range. Comparisons between the TAo-AVR and TF-AVR groups were performed using χ2 or Fisher’s exact tests for categorical data and Student’s t-tests or the Mann-Whitney non-parametric test (when skewed) for continuous data. For all-cause mortality, Kaplan-Meier survival analyses were used, and the TF-AVR and TAo-AVR groups were compared using log-rank tests. Results were considered as statistically significant when the p-value was less than 0.05. All data handling and analyses were performed using Stata Statistical Software, Stata SE version 10 (StataCorp LP, College Station, TX, USA).
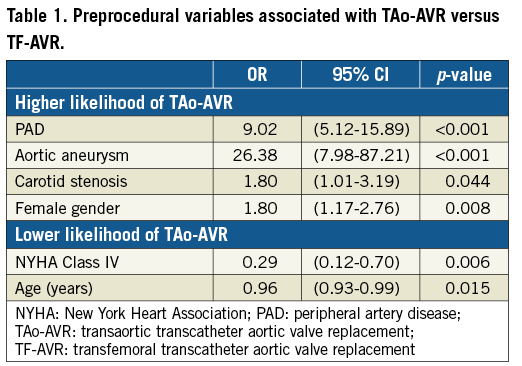
Propensity score matching was used to assess the relationships between access site and outcomes, regardless of baseline differences between TAo-AVR and TF-AVR patients. Preprocedural variables independently associated with transaortic access route selection were identified using stepwise forward logistic regression. The logistic equation obtained from the final model enabled the calculation of the probability of being allocated to the TAo-AVR group. The propensity score matching was performed in a 1:1 ratio, based on the probability of a random assignment to the TAo-AVR group, using the 1-nearest neighbour method: TAo-AVR cases with propensity scores that deviated >0.10 from the nearest neighbour were considered unmatched.
Results
A total of 644 patients underwent TAVR, performed with either Edwards balloon-expandable or Medtronic self-expanding prostheses during the study period: 163 of them were treated with the TAo approach (25.3%), and 481 were treated with the TF approach (74.7%). Within the same period, 20 patients were treated via the transapical approach, and 17 via the subclavian approach; these patients were not included in the final analysis. Preprocedural variables independently associated with the transaortic access route selection are summarised in Table 1. Among the 163 TAo-AVR patients initially included, 124 were propensity score matched in a 1:1 ratio with TF-AVR patients (76% of the potential matches), resulting in similar baseline characteristics between the groups (Table 2).
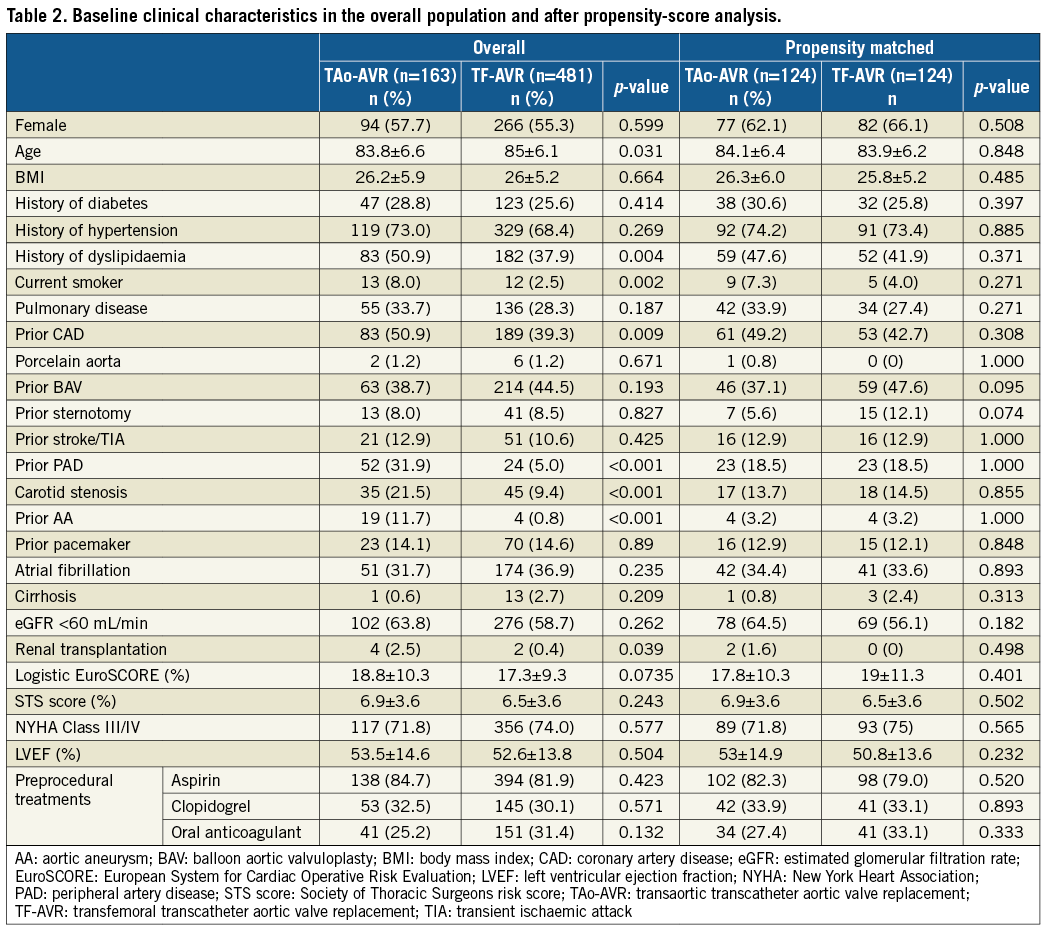
BASELINE CLINICAL CHARACTERISTICS
The main characteristics of the two groups, in the overall population and in the matched cohort, are summarised in Table 2. In the overall population, patients who underwent TAo were slightly younger (83.8 vs. 85.0 years, p=0.031), but more prone to vasculopathy such as peripheral artery disease (PAD) (31.9% vs. 5.0%, p<0.001), coronary artery disease (50.9% vs. 39.3%, p=0.009), carotid stenosis (21.5% vs. 9.4%, p<0.001) and aortic aneurysm (11.7% vs. 0.8%, p<0.001). STS scores were not statistically different between the groups (6.9% in the TAo-AVR group vs. 6.5% in the TF-AVR group, p=0.2). Baseline echocardiographic data were similar in both groups. Approximately one third of patients were treated with a dual antiplatelet therapy before the procedure, with no significant differences between the groups.
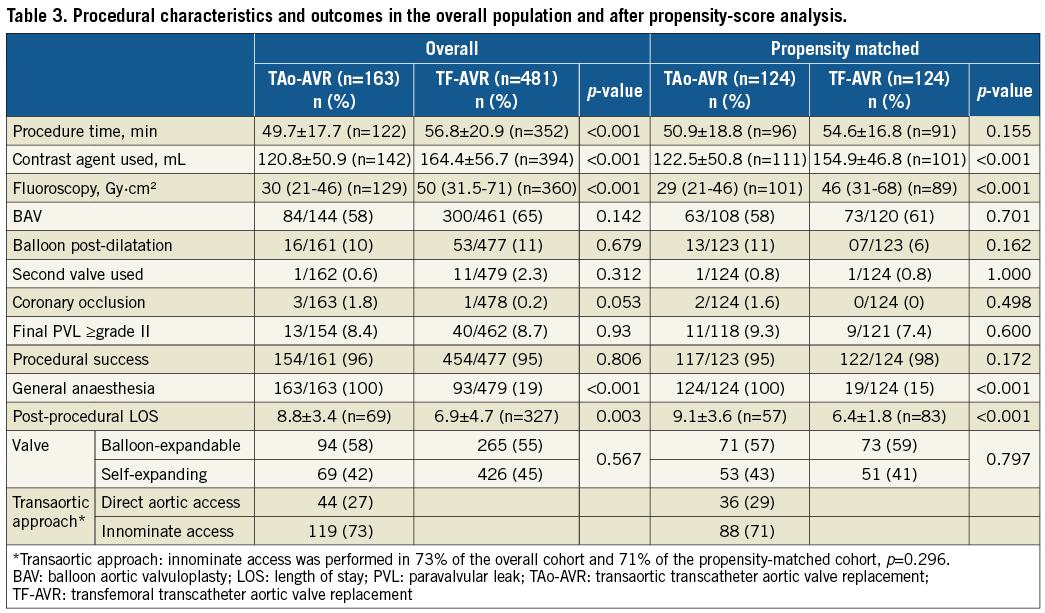
PROCEDURAL CHARACTERISTICS
The main procedural and post-procedural outcomes are summarised in Table 3. Balloon-expandable and self-expanding prostheses were used in similar proportions in both groups, with a predominance of balloon-expandable prostheses in the overall population. Procedural time was shorter in the TAo-AVR group (49.7 vs. 56.8 min, p<0.001). Contrast agent (120.8±50.9 vs. 164.4±56.7 mL, p<0.001) and radiation (30 [21-46] vs. 50 [31.5-71] Gy·cm², p<0.001) were reduced in the TAo-AVR group. Balloon aortic valvuloplasty prior to aortic valve implantation was performed in 58% of TAo-AVR patients and in 65% of TF-AVR patients (p=0.142). The rate of balloon post-dilatation and the frequency of need for a second valve were similar. Only 19% of the TF-AVR procedures were performed under general anaesthesia. The rate of procedural coronary occlusion was numerically higher in the TAo-AVR group, without reaching statistical significance (1.8% vs. 0.2%, p=0.057). Procedural success was similar between the groups (96% vs. 95%, p=0.8). No differences were observed regarding paravalvular leak at the end of the procedure (PVL ≥grade II: 8.4% vs. 8.6%, p=0.93). Importantly, post-procedural length of stay was significantly shorter in the TF-AVR group (6.9±4.7 vs. 8.8±3.4 days, p<0.001).
MORTALITY AND CARDIOVASCULAR EVENTS
Short- and long-term clinical outcomes are summarised in Table 4. The thirty-day mortality rates of TAo-AVR and TF-AVR patients were not different in the overall population, or after propensity-score analysis (7.3% vs. 7.6%, p=0.8 and 7.3% vs. 6.5%, p=0.8, respectively). Although non-significant, the one-year mortality rate in the overall population tended to be higher in the TAo-AVR group (18.4% vs. 15.8%, p=0.6), while one-year mortality rates following propensity-score analysis were similar (15.3% vs. 16.1%, p=0.8) (Figure 1, Table 4).
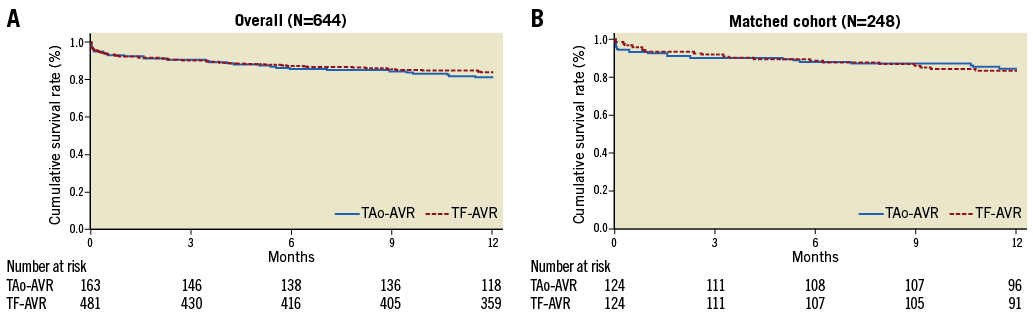
Figure 1. Kaplan-Meier survival curves obtained from a stratified approach in the overall population and in the matched cohort. A) Overall population. B) Matched cohort. Survival rates were calculated using Kaplan-Meier methods and compared using the log-rank test. Although non-significant, the one-year mortality rate in the overall population tended to be higher in the transaortic (TAo-AVR) group (log-rank p=0.461). One-year mortality rates were comparable between the TAo-AVR and transfemoral (TF-AVR) groups (log-rank p=0.866) following propensity-score analysis.
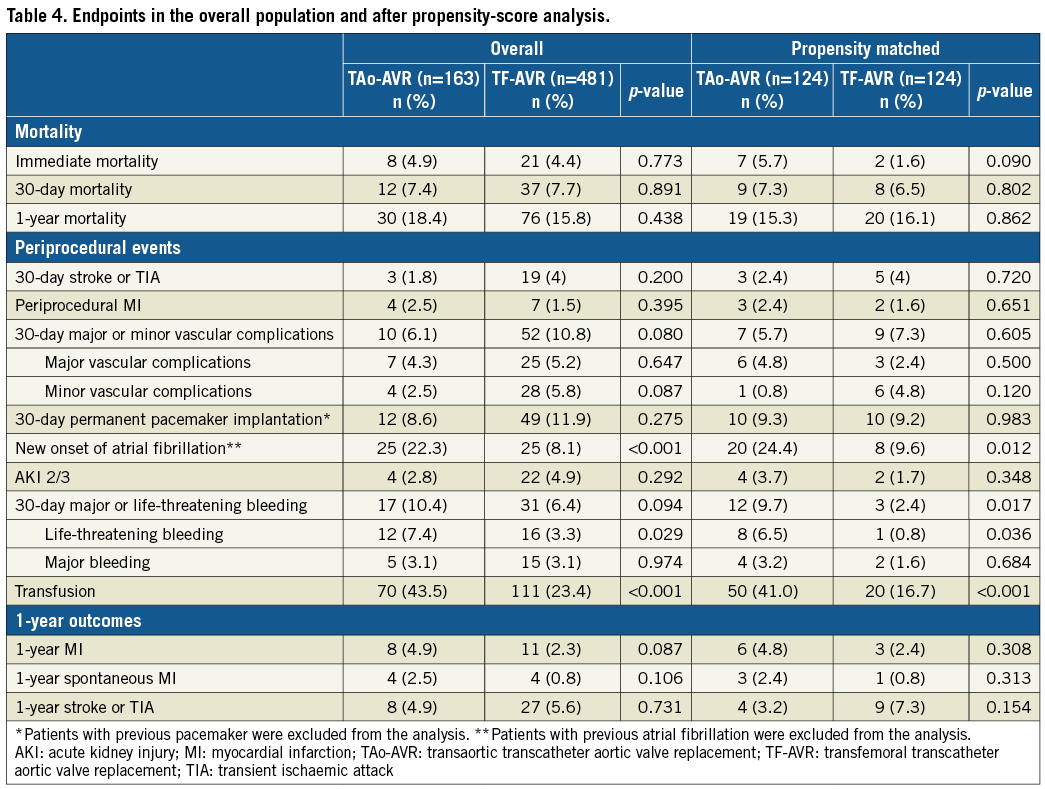
In the matched cohort, transaortic access was associated with a higher risk of new-onset atrial fibrillation (NOAF) (24.4% vs. 9.6%, p=0.012), life-threatening bleedings (6.5% vs. 0.8%, p=0.036) and transfusion (41% vs. 16.7%, p<0.001).
The occurrence of acute kidney injury (3.7% vs. 1.7%, p=0.3), 30-day pacemaker implantation (9.3% vs. 9.2%, p=0.9), and major or minor vascular complications (5.7% vs. 7.3%, p=0.6) was comparable between the groups. No differences were observed for one-year myocardial infarction rates (4.8% vs. 2.4%, p=0.3). Thirty-day and one-year stroke occurrence was numerically lower in the TAo-AVR group but did not reach statistical significance (2.4% vs. 4%, p=0.7 and 3.2% vs. 7.3%, p=0.2, respectively) (Figure 2).
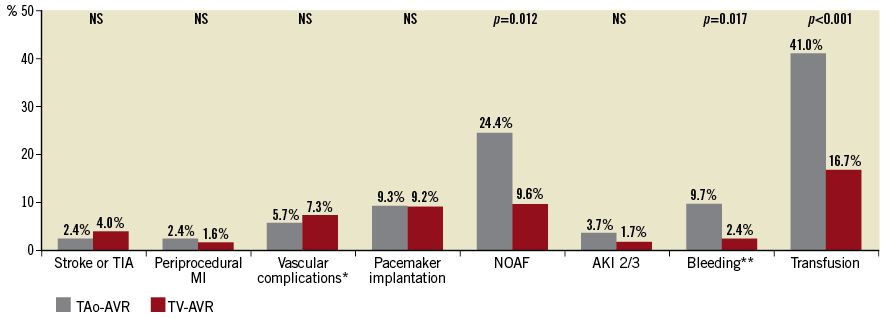
Figure 2. Periprocedural events according to vascular access in the propensity-matched population. *Vascular complications: 30-day major or minor vascular complications. **Bleeding: 30-day major or life-threatening bleeding. AKI: acute kidney injury; MI: myocardial infarction; TAo-AVR: transaortic transcatheter aortic valve replacement; TF-AVR: transfemoral transcatheter aortic valve replacement; TIA: transient ischaemic attack
Discussion
We report herein the first propensity-matched comparison of long-term outcomes between TAo-AVR and TF-AVR in a high-volume centre. We observed differences in baseline characteristics between the two groups, with a “vascular” pattern of patients from the TAo group that could be responsible for bias in estimating outcomes. After propensity-score analysis, no significant differences were found regarding 30-day and one-year mortality between TAo-AVR and TF-AVR.
The development of smaller sheath delivery systems has led to a decrease in the proportion of non-transfemoral procedures. The results of the FRANCE TAVI registry showed that an alternative access route was still used in 17% of TAVR patients between 2013 and 201511. In our centre, transaortic access was selected as the first alternative access route, representing approximatively one fourth of TAVR cases. A recent Society of Thoracic Surgeons/American College of Cardiology TVT Registry experience showed that transapical and transaortic approaches are employed almost equally in the USA1. In a significant proportion of patients with unsafe transfemoral access, the question of the best alternative access route remains under debate.
TAo access offers several advantages over other alternative routes, such as a high feasibility, with direct and stable access to the aortic valve. Furthermore, in case of haemodynamic collapse during the procedure, TAo access enables rapid conversion to full sternotomy and rapid control of major complications such as ventricular perforation. The upper ministernotomy incision required for TAo-AVR is typically well tolerated with less postoperative pain and fewer effects on respiratory function than a left lateral thoracotomy. Transaortic access provides a direct control of valve positioning during deployment. Axial alignment in the aortic annulus might be challenging with self-expanding prostheses. In the present study, we did not find differences regarding procedural success, paravalvular leak and mortality between balloon-expandable and self-expanding prostheses in TAo-AVR patients (data not shown).
Arai et al recently published similar results in a direct comparison between TF-AVR (n=467) and TAo-AVR (n=289). The 30-day mortality and one-year survival rates were similar among TF-AVR and TAo-AVR patients, with a trend in favour of the TF approach7. This trend was also observed in our overall population for the one-year survival rate, but it disappeared after propensity-score analysis, indicating that it was probably related to baseline differences between the two populations.
Interestingly, these long-term results obtained with the TAo approach were observed despite a significant proportion of patients with prior sternotomy (8% in the TAo-AVR group). Internal mammary artery injury is a dramatic event that may occur during manubriotomy. The feasibility of the manubriotomy in the context of TAo-AVR was confirmed on preprocedural CT scan data. Similarly, a hostile ascending aorta has been suggested as a strong contraindication for TAo-AVR because of the excessive stroke risk from atheroembolism. The presence of a calcification-free zone on the diseased aorta or innominate artery puncture could contribute to a decrease in thrombotic events.
Other alternative access sites have been developed with good short-term results such as the transcarotid, trans-subclavian or, more recently, the transcaval route. If subclavian access has recently been shown to have similar one-year outcomes using a self-expanding prosthesis in comparison with the transfemoral approach12, further scientific data are needed to determine the ideal alternative access strategy. Finally, there is a large heterogeneity of practices among the different TAVR centres when facing a patient with challenging iliofemoral anatomy. Making treatment decisions, or the choice of an alternative access route, is highly variable and depends on several factors such as local TAVR experience, or the habits of the surgical teams involved in the TAVR programme.
These data show that TAo-AVR and TF-AVR have similar long-term outcomes. This highlights the safety and interest of the transaortic approach as an alternative access for TAVR in patients with severe PAD or challenging iliofemoral anatomies. However, this also outlines a number of advantages of performing TF-AVR rather than TAo-AVR, especially less NOAF, bleedings, transfusion, and reduced length of hospital stay.
Several studies have suggested a relation between NOAF and an excess risk of stroke and mortality following TAVR13. Despite higher NOAF, there was a non-significant trend towards a lower one-year stroke risk in the TAo-AVR group (3.2% vs. 7.3%, p=0.154). This could be explained by the procedural advantages of the TAo procedure, in particular because it avoids crossing the aortic arch, or the possible “postoperative AF” type of NOAF following TAo-AVR, with potentially less recurrence and fewer thromboembolic consequences. Although these are only hypothetical explanations, they are supported by low stroke rates in other TAo-AVR studies (one-month stroke risk of 1.6% in the ROUTE registry8, and 0.9% in the meta-analysis of Dunne et al14). Further studies are needed to confirm this possible lower intrinsic stroke risk in TAo procedures.
Based on our results, we suggest that the TF access should remain the first access route to be considered when planning TAVR. However, when facing a difficult iliofemoral anatomy, Heart Teams should consider these comparable long-term outcomes following TAo-AVR in order to determine the best access site for their patients15.
Study limitations
This retrospective, observational study was conducted at a single centre. Some degree of observation bias cannot be ruled out despite the extra care taken in data collection and VARC-2 endpoint definitions. Other important factors related to access decision or outcomes, such as frailty, were not included. Finally, the particular reason that led to the decision for the patient to undergo TF-AVR or TAo-AVR was not mentioned, and a comparison with other alternative accesses was not possible due to the low number of procedures in our centre.
Conclusions
TAo-AVR and TF-AVR show similar long-term outcomes after investigation of the differences between the two populations. The TAo approach can be considered as a valid alternative access route in patients referred to TAVR. TAo-AVR is associated with higher NOAF, bleeding, transfusion and prolonged length of hospital stay.
| Impact on daily practice The TF approach is the preferred access route for TAVR, but an alternative route is required in patients with challenging anatomies. After accounting for baseline differences, patients treated with TAo-AVR have similar long-term outcomes compared with TF-AVR patients. Transaortic access is associated with an excess risk of new-onset atrial fibrillation, bleedings, transfusion and prolonged length of hospital stay. |
Conflict of interest statement
B. Marcheix reports personal fees from Edwards Lifesciences and Medtronic, outside the submitted work. T. Lhermusier reports personal fees from Edwards Lifesciences, Medtronic, and Abbott Vascular, outside the submitted work. The other authors have no conflicts of interest to declare.

