Abstract
Background: As transaxillary (TAx) access has become the most common alternative to transfemoral (TF) transcatheter aortic valve replacement (TAVR), there is increasing use of a percutaneous approach.
Aims: This study sought to determine whether there are differences in outcomes using a percutaneous access versus cutdown for TAx TAVR.
Methods: Using data from the STS/ACC TVT Registry, consecutive patients undergoing TAx TAVR with balloon-expandable valves between July 2015 and December 2020 were included. Propensity score-based matching was performed to evaluate the association between method of TAx access and outcomes.
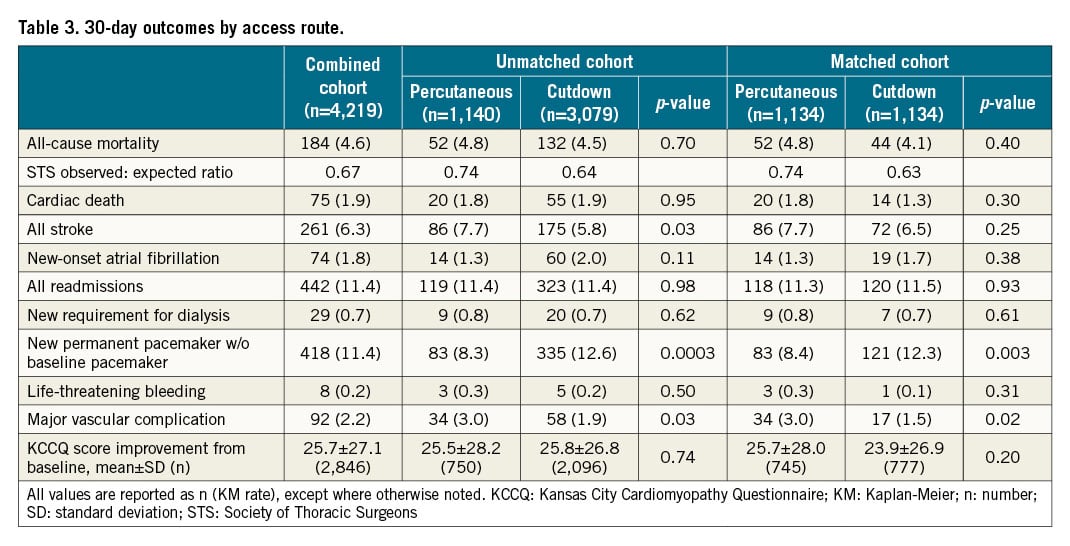
Results: Of 4,219 patients, 1,140 (27.0%) underwent percutaneous access and 3,079 (73.0%) had surgical cutdown for TAx TAVR, with the proportion of percutaneous cases increasing over time. After propensity matching, there were no significant baseline differences between patients undergoing TAx access by either approach. At 30 days, there were similar rates of all-cause mortality (4.8% in percutaneous patients vs 4.1% in surgical patients; p=0.40) and stroke (7.7% vs 6.5%; p=0.25). Those undergoing percutaneous TAx access were more likely to receive conscious sedation and have less need for the intensive care unit (ICU). Percutaneous access was associated with a higher rate of major vascular complication (3.0% vs 1.5% in surgical patients; p=0.02) but not life-threatening bleeding (0.3% vs 0.1%; p=0.31).
Conclusions: This study supports the safety and efficacy of percutaneous TAx TAVR compared to traditional surgical cutdown. Percutaneous access was associated with a shorter ICU stay and a higher rate of major vascular complication without an increase in life-threatening bleeding.
Introduction
Although transfemoral access remains the cornerstone of transcatheter aortic valve replacement (TAVR), severe iliofemoral tortuosity, atherosclerotic disease, and small vessel caliber preclude the safe application of this approach in certain patients with symptomatic aortic stenosis123. Since the introduction of TAVR in 2002, multiple access routes have been developed to enable more patients to experience the benefits of a less invasive alternative to open surgery. In the largest alternative access cohort previously studied, 5.7% of the 63,581 patients in the TVT Registry underwent non-transfemoral (TF) access with a SAPIEN 3 valve (Edwards Lifesciences) from June 2015 up to and including February 2018. Temporal trends in this study revealed that transaxillary (TAx) TAVR accounted for nearly half of non-TF access cases (49.0% in Q4 2017)4.
In contrast to transapical, transaortic and transcarotid access, which are primarily performed under general anaesthesia using surgical exposure, TAx access can be performed through direct percutaneous cannulation. Therefore, it more readily allows adherence to a minimalist periprocedural strategy56. Use of local anaesthesia and monitored anaesthesia care (MAC) with conscious sedation result in decreased length of stay in the intensive care unit (ICU), earlier mobilisation and discharge from the hospital, and significant cost savings7. Although the feasibility and safety of an entirely percutaneous TAx approach for TAVR have been described previously, prior studies have focused on single-centre experiences89, and surgical exposure remains the dominant method for attaining TAx access4. A recent multicentre, prospective study demonstrated no significant differences in procedural and 30-day outcomes between the 19 patients who underwent percutaneous access and the 54 who underwent surgical cutdown for TAx TAVR; however, the sample size was small and the study was underpowered10.
The aim of the current study was to determine whether there are differences in outcomes between TAx TAVR cases with the latest-generation balloon-expandable transcatheter heart valves performed through direct percutaneous access and surgical cutdown using data from the Society of Thoracic Surgeons/American College of Cardiology (STS/ACC) TVT Registry. As prior studies have shown important differences in baseline characteristics between patients chosen for percutaneous and surgical access for TAVR411, we evaluated the safety and efficacy of percutaneous access compared with surgical cutdown using propensity score-based matching. Furthermore, we performed a sensitivity analysis using instrumental variable analysis (IVA), which controls for both measured and unmeasured confounding, enabling causal inferences using observational data.
Methods
STUDY POPULATION
The STS/ACC TVT Registry (TVT Registry) is a collaborative national clinical registry programme developed by the STS and the ACC in response to the centres for Medicare and Medicaid Services requirement for national registry participation of all US TAVR centres. Participating centres use standardised definitions to report data on patient demographics, comorbidities, and outcomes for nearly all TAVR procedures performed in the USA using commercially approved devices. The TVT Registry protocol was granted a waiver of informed consent by Advarra and Duke University institutional review boards. No additional institutional review board approval was required based on the retrospective and de-identified nature of the data set.
This retrospective analysis includes all consecutive patients reported in the TVT Registry who underwent TAx and transsubclavian TAVR using either percutaneous access or surgical cutdown with the SAPIEN 3 and SAPIEN 3 Ultra valves (Edwards Lifesciences) between July 2015 and December 2020. The majority of cases reported as “transsubclavian” are actually misclassified as they are most often performed from an infraclavicular approach, and thus technically involve access of the axillary artery12. Concordant with existing literature, in which “transsubclavian” and “transaxillary” access are grouped together13, we use the term “transaxillary” throughout this paper to encompass cases reported as having utilised either transaxillary or transsubclavian access.
We examined temporal trends in access method at TAVR centres performing any type of TAx access, as well as variations in the proportion of these cases performed using percutaneous access throughout the study period.
STATISTICAL ANALYSIS
The Kolmogorov-Smirnov test was used to determine normal distribution. For unadjusted analyses, continuous variables are presented as mean±SD when normally distributed and as median (interquartile range [IQR]) when not normally distributed and compared between groups using the two-sample Student’s t-test or Wilcoxon rank-sum test. Categorical variables are expressed as frequencies and percentages and compared using Fisher’s exact or chi-square tests. Thirty-day mortality, stroke, and other adverse events are based on Kaplan-Meier estimates and all comparisons are made using the log-rank test.
Propensity score-based matching of all TAx TAVR patients was performed to minimise the impact of selection bias and other confounders. Propensity scores were calculated using a logistic regression model based on 34 relevant baseline patient characteristics (covariates) with the access method as the dependent variable. The covariates included in the model were age, sex, body mass index, prior percutaneous coronary intervention, prior coronary artery bypass grafting, prior stroke, carotid stenosis, peripheral arterial disease, hypertension, diabetes, chronic lung disease, porcelain aorta, atrial fibrillation, immunocompromised status, creatinine ≥2 mg/dL, glomerular filtration rate, haemoglobin, left ventricular ejection fraction, mean transaortic gradient, aortic regurgitation, mitral regurgitation, tricuspid regurgitation, New York Heart Association (NYHA) Functional Class, five-metre walk test, Kansas City Cardiomyopathy Questionnaire (KCCQ) overall summary score, Society of Thoracic Surgery (STS) risk score, current dialysis, cardiogenic shock within 24 hours, hostile chest, permanent pacemaker, heart failure within two weeks, annular size, current or recent smoker and previous implantable cardioverter defibrillator.
Missing baseline values were imputed using the Markov chain Monte Carlo method prior to modelling. Imputation was only performed for baseline variables used in propensity score matching. Using the propensity score, cases performed by percutaneous TAx access were matched 1:1 to those performed through surgical cutdown using a greedy matching strategy, producing two balanced groups. Balance between the cohorts was ensured by calculating standardised differences and using a cut-off of a difference less than 0.10 to define favourable balance. Imputed values were not used in subsequent analyses of outcomes. All statistical analyses were performed on complete data sets. The LOVE plot (Supplementary Figure 1) and histogram of propensity score before and after matching (Supplementary Figure 2) are included in the supplementary data.
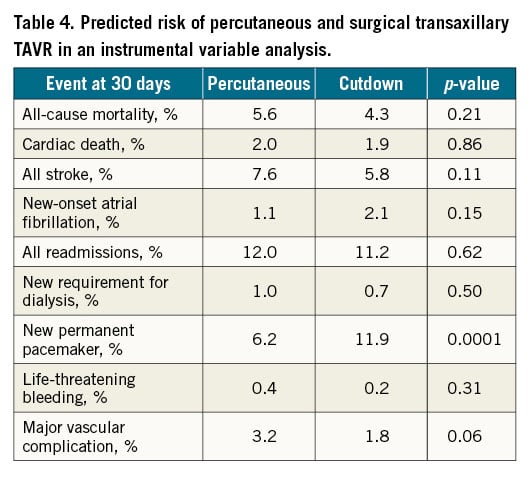
Additionally, we performed a sensitivity analysis using IVA to evaluate further the effect of TAx access method on outcomes in the presence of unmeasured/unknown confounders14. To perform the IVA, the two-stage least square regression method was used with each individual patient as an observation. First, the probability of percutaneous TAx access was modelled as a function of a hospital’s proportion of percutaneous TAx access method (the IV) using logistic regression. Second, clinical endpoints were modelled as a function of predicted probability of percutaneous TAx access (from the first stage model). Absolute risk estimates in percutaneous versus surgical groups were calculated based on the patient with percutaneous TAx access probability of 1 versus 0 in the outcome Cox regression model, with bootstrap resampling (1,000 samples) used to calculate hazard ratios and the associated 95% confidence intervals.
To investigate the relationship between hospital volume of TAx TAVR procedures and clinical outcomes, a cut-off of >10 cases performed during the study period was used to stratify high (>10 cases) and low (≤10 cases) volume centres. We then examined differences in baseline patient characteristics and the clinical outcomes of patients selected to undergo percutaneous access compared to surgical cutdown at centres of varying volume.
All statistical analyses were performed using SAS version 9.4 SAS Institute). Edwards Lifesciences provided statistical support but did not develop the analysis plan or participate in the drafting or editing of this manuscript.
Results
Among 193,940 patients in the TVT Registry who underwent TAVR with the balloon-expandable SAPIEN 3 and SAPIEN 3 Ultra valves from July 2015 up to and including December 2020, 4,396 cases were performed via the TAx route, accounting for 42.7% of alternative access TAVR cases and 2.3% of all TAVR cases. There were data available on whether percutaneous access or cutdown was used in 4,219 cases, which were then included in subsequent analyses. The 177 cases that were excluded were performed using mini-sternotomy, mini-thoracotomy, other or unknown valve sheath access methods, had been performed less than 30 days from the data extraction date or had a primary indication of aortic regurgitation. Of the cohort of 4,219 patients, 1,140 (27.0%) underwent percutaneous access and 3,079 (73.0%) had surgical cutdown for TAx TAVR. The percentage of TAx cases performed percutaneously increased significantly over the study period (6.7% in quarter 3 of 2015 vs 36.2% in quarter 3 of 2020) (Figure 1). A total of 493 centres in the USA performed TAx TAVR during the study period, with 364 centres performing 10 or fewer cases.
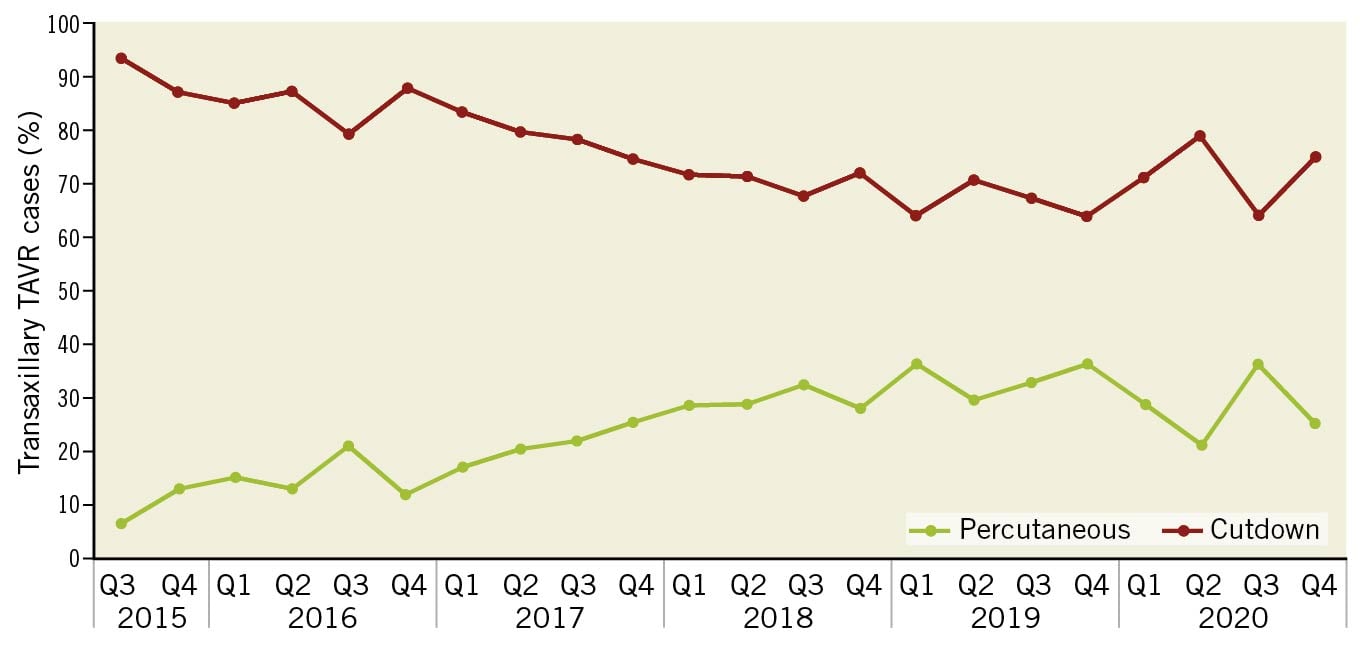
Figure 1. Temporal trends in the use of percutaneous access versus surgical cutdown in transaxillary TAVR. This graph shows the proportion of centres performing percutaneous and surgical access for TAx TAVR using balloon-expandable valves from quarter 3 of 2015 to quarter 4 of 2020. TAx TAVR: transaxillary transcatheter aortic valve replacement
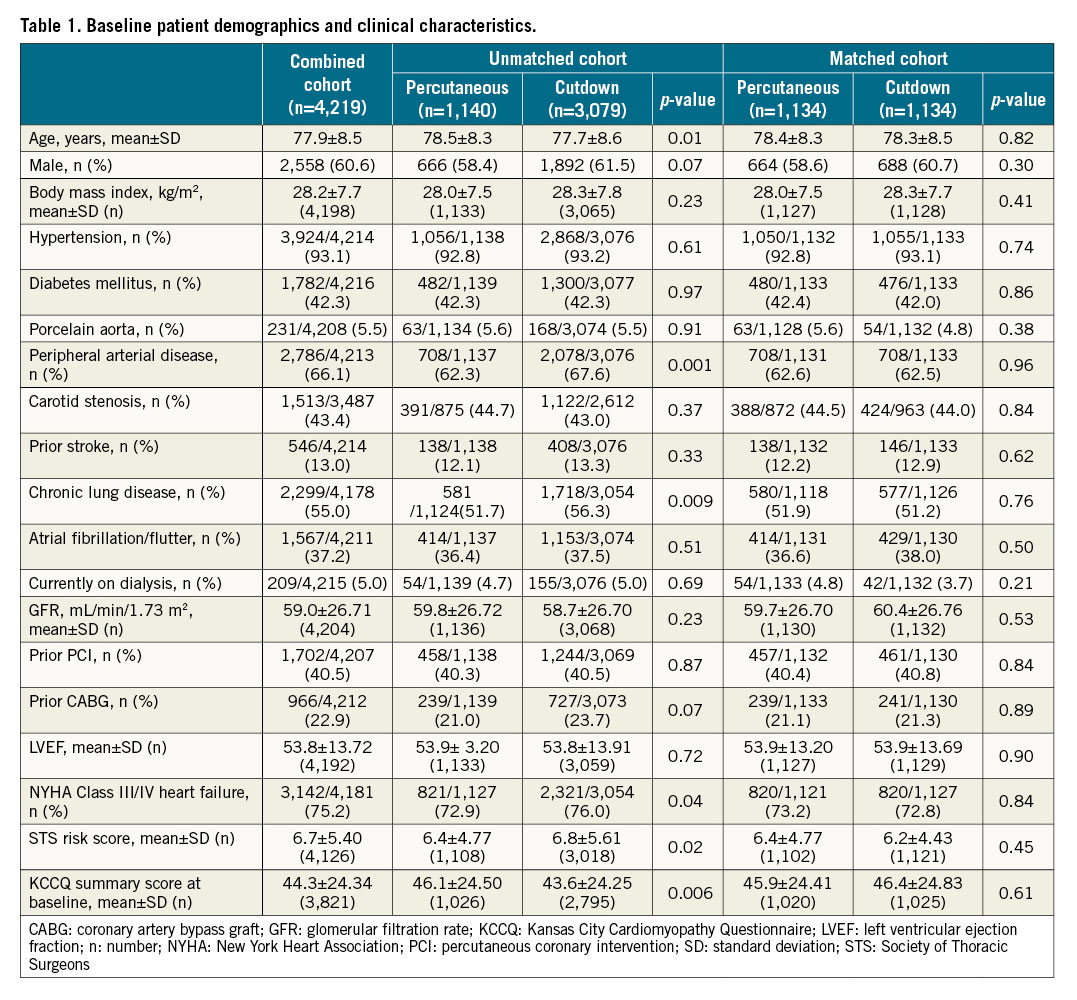
PATIENT DEMOGRAPHICS AND CLINICAL CHARACTERISTICS
Baseline demographic and clinical characteristics of patients undergoing TAx TAVR are shown in Table 1. Patients undergoing TAx TAVR were generally elderly, male, and had a high prevalence of comorbidities such as chronic lung disease, atrial fibrillation and/or flutter, hypertension, and diabetes. Two-thirds of patients had peripheral arterial disease. After propensity score-based matching, there were no significant baseline differences between patients undergoing TAx access by either a percutaneous or surgical approach, including body mass index and prevalence of peripheral arterial disease.
PROCEDURAL CHARACTERISTICS AND PERIOPERATIVE OUTCOMES
In the analysis of propensity score-matched cohorts, patients undergoing percutaneous TAx access were significantly more likely to receive conscious sedation than those undergoing surgical cutdown (279/1,132 [24.7%] percutaneous patients vs 63/1,130 [5.6%] surgical patients; p<0.001). The overall rate of successful device implantation was high in both groups (98.9% in percutaneous patients vs 99.5% in surgical patients, p=0.11). There was no significant difference in procedure duration; however, percutaneous cases had longer fluoroscopy time and greater use of contrast (Table 2).
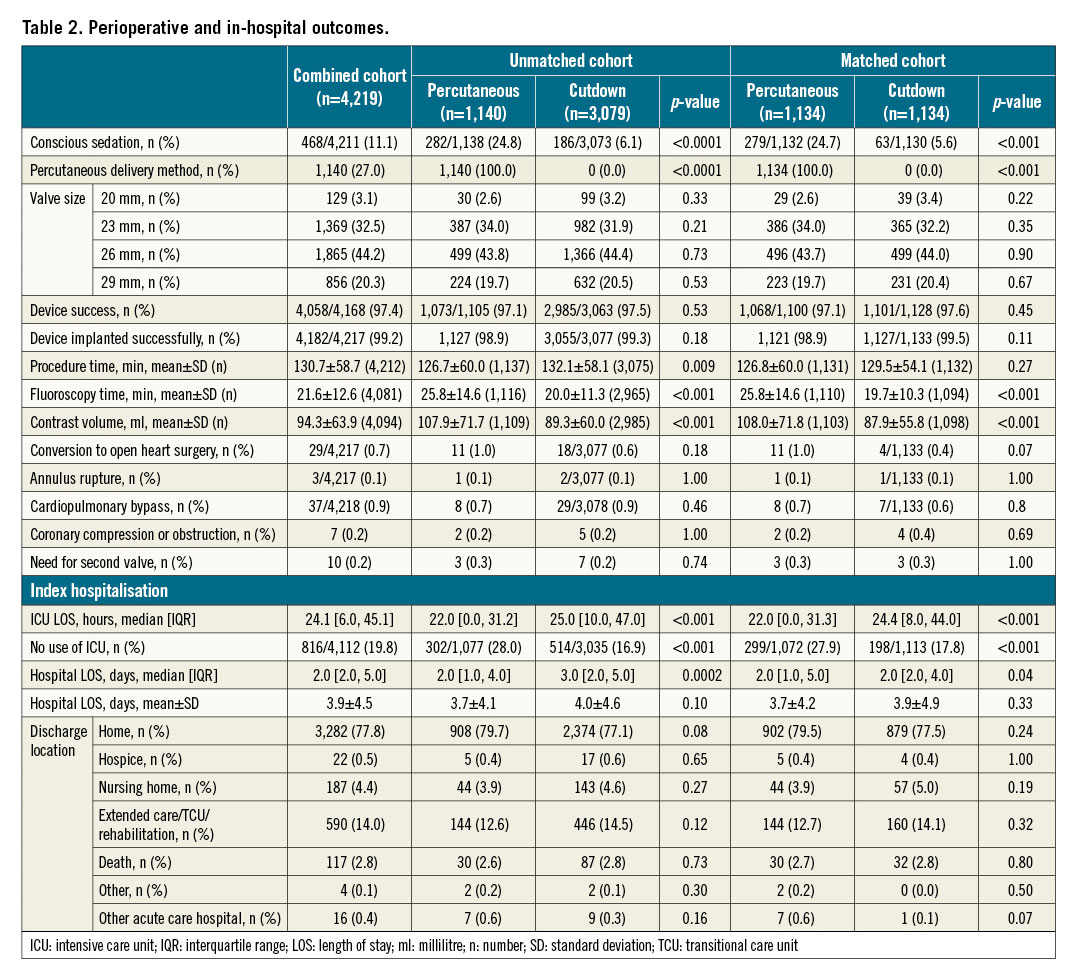
Additionally, percutaneous TAx access was associated with less utilisation of the intensive care unit (ICU) (median 22.0 [IQR 0.0, 31.3] hours vs 24.4 [8.0, 44.0]; p<0.001) and greater likelihood of bypassing the ICU altogether (299/1,072 [27.9%] vs 198/1,113 [17.8%] of patients with no use of the ICU; p<0.001) compared to surgical TAx access. Overall length of hospital stay was similar in those undergoing percutaneous access (median 2.0 [IQR 1.0, 5.0] days vs 2.0 [2.0, 4.0]; p=0.04) (Table 2).
CLINICAL OUTCOMES
In the matched analysis, there was no significant difference in rates of all-cause mortality or stroke at 30 days in patients undergoing either percutaneous or surgical access. Patients undergoing percutaneous TAx TAVR had a significantly higher rate of major vascular complication (3.0% vs 1.5% in surgical patients; p=0.02) (Table 3). Furthermore, there was a significantly higher rate of new permanent pacemaker implantation in those undergoing surgical cutdown (Table 3, Central illustration).
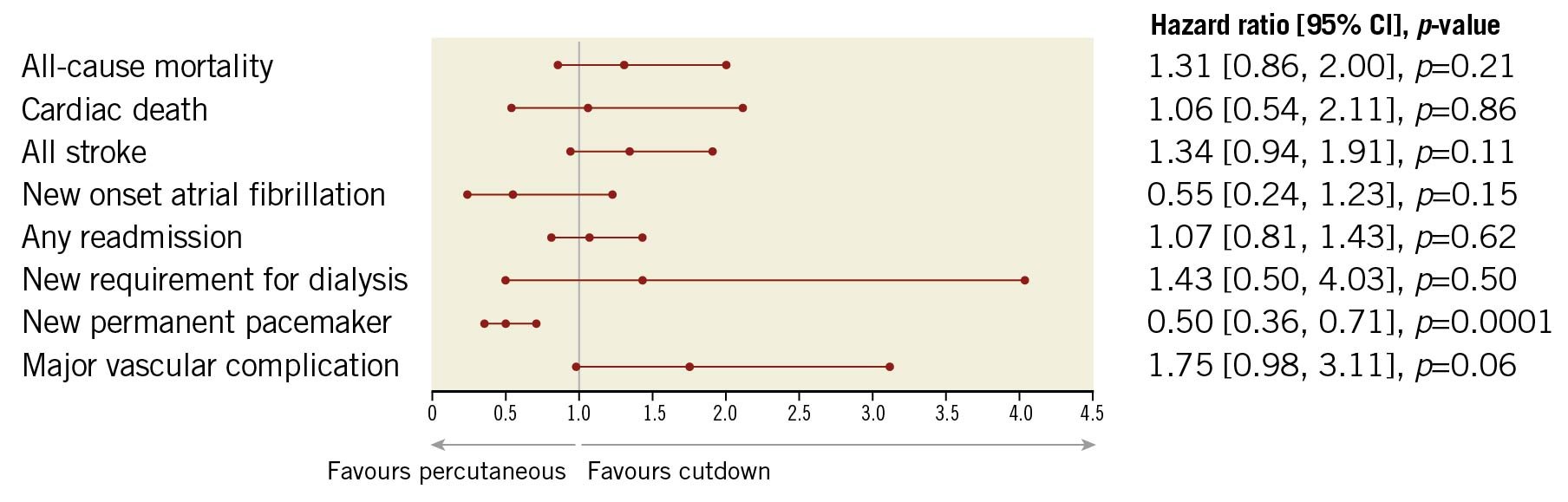
Central illustration. Forest plot of 30-day outcomes of patients undergoing percutaneous or surgical transaxillary access in propensity-matched analysis. This forest plot shows clinical outcomes at 30 days after transaxillary TAVR by either percutaneous or surgical access in patients who have undergone propensity score-based matching to account for baseline differences.
In the sensitivity analysis, percutaneous TAx access was associated with a marginally higher rate of major vascular complications, whereas surgical cutdown was associated with a significantly higher rate of implantation of a new permanent pacemaker (Table 4).
OUTCOMES ACCORDING TO CENTRE VOLUME OF TRANSAXILLARY TAVR CASES
Outcomes according to centre volume are reported in Supplementary Table 1 and Supplementary Table 2. There was no difference in 30-day outcomes including all-cause mortality, stroke, life-threatening bleeding, or new requirement for dialysis seen in patients undergoing percutaneous TAx TAVR at centres with variable experience (Supplementary Table 1). Patients undergoing surgical cutdown experienced more variability in outcomes according to centre volume, with those treated at lower volume centres experiencing significantly higher rates of all-cause mortality, cardiac death, and new dialysis requirement (Supplementary Table 2).
Additionally, there were no baseline differences in the mean STS scores of patients selected to undergo TAx TAVR by either percutaneous or surgical access at high-volume compared to low-volume centres (Supplementary Table 3). Finally, in an effort to elucidate why patients undergoing surgical TAx access were more likely to receive a permanent pacemaker, we examined the rate of pacemaker implantation in the broader population of patients undergoing transfemoral TAVR at centres performing TAx access exclusively by either a percutaneous or surgical approach. Patients undergoing transfemoral TAVR at centres that perform TAx access solely by surgical cutdown had a slightly higher mean STS score at baseline and were significantly more likely to receive a permanent pacemaker (Supplementary Table 4). Subgroup analysis of both the percutaneous and surgical cohorts segregated by observation period from 2015 to 2017 and from 2018 to 2020 was performed. Although pacemaker rates during the index hospitalisation declined significantly over time for patients undergoing percutaneous access (11.4% from 2015-2017 vs 5.9% from 2018-2020; p=0.004), this trend was not seen in patients undergoing surgical cutdown (12.0% vs 10.3%; p=0.17). These trends remained stable at 30 days, with declining rates of pacemaker implantation in patients undergoing percutaneous TAx TAVR over time (12.0% from 2015-2017 vs 7.2% from 2018-2020; p=0.02); however, no change was seen in patients undergoing surgical access (13.6% from 2015-2017 vs 12.0% from 2018-2020; p=0.22) (Supplementary Table 5, Supplementary Table 6).
Discussion
Our analysis using the ACC/STS TVT Registry data is the largest to date to compare outcomes between percutaneous and surgical access for TAx TAVR using balloon-expandable valves. The principal findings of this study are: (i) the proportion of centres performing percutaneous rather than surgical access for TAx TAVR using balloon-expandable valves has increased nearly sixfold over the past few years; (ii) percutaneous TAx access is safe and feasible with no difference in procedural success, all-cause mortality and stroke at 30 days compared to surgical cutdown; (iii) percutaneous TAx TAVR is associated with greater use of conscious sedation and lower ICU utilisation; and (iv) major vascular complication was more common in patients undergoing percutaneous access whereas rates of permanent pacemaker implantation were higher following surgical cutdown.
In the early 2000s, the intial alternative access was transthoracic through either a transapical or transaortic approach; however, patients undergoing transthoracic TAVR had worse outcomes, including higher mortality, than patients undergoing femoral access15. Since then, TAx access has become the most commonly used alternative approach for TAVR. Our data show that an increasing proportion of these cases are being performed through a percutaneous, rather than a surgical, approach. One of the potential benefits of an entirely percutaneous approach may be that it facilitates adherence to a minimalist strategy, including avoidance of general anaesthesia. The use of conscious sedation during TAVR has been associated with lower in-hospital and 30-day mortality, as well as decreased ICU utilisation and length of hospital stay1617. It is likely that patients who undergo TAVR through surgical cutdown, regardless of access site, are more often admitted to the ICU to undergo closer monitoring. Although numbers of patients in the current study were too small to enable meaningful subgroup analyses, it would be interesting to explore whether there are differences in outcomes in patients undergoing percutaneous TAx TAVR using conscious sedation versus general anaesthesia. Prior work by our group demonstrated favourable outcomes following TAx TAVR, with a procedural success rate of 97.4% and a vascular complication rate of 2.5%, even though most centres had performed less than five cases4. The current, much larger study demonstrates that the rate of successful device implantation during TAx TAVR remains high at 99.2% and major vascular complication remains low at 2.2%, despite increasing utilisation of this approach at a larger number of centres across the USA. The mean procedure duration in both groups was similar at around two hours, and this likely reflects the early learning curve for many operators. There was a trend towards a greater likelihood of conversion to open surgery seen in the percutaneous access group (11/1,134 cases vs 4/1,133 cases in the surgical group, p=0.07). However, there were no differences in rates of procedural complications such as annular rupture, ventricular rupture, valve embolisation, aortic dissection or coronary obstruction for which open surgery may have been necessary.
In general, lower volume TAVR programmes have demonstrated higher mortality in patients undergoing both transfemoral and non-transfemoral access18, so we expected to find an association between centre volume and outcomes for a low frequency procedure such as alternative access TAVR. Interestingly, there was no association between centre volume and outcomes for percutaneous TAx TAVR, but there was significantly higher mortality in patients undergoing surgical cutdown at lower volume centres. One possible explanation is that centres early in their experience with TAx access may start out using a surgical rather than a percutaneous approach, and the worse outcomes reflect the initial steep rise in the learning curve inherent in the adoption of a new access method. In contrast, percutaneous TAx access may be favoured by more experienced operators, leading to lower variability in outcomes.
Although there was a higher rate of major vascular complications seen with percutaneous access, it remained low at 3.0%, comparing favourably to the rate of 9.3% recently reported in patients from the TVT Registry undergoing transfemoral TAVR19. Furthermore, the overall incidence of life-threatening bleeding was low, with 8 events in the entire cohort of 4,219 patients; 3 events occurred in those undergoing percutaneous TAx access and 5 events occurred in the surgical group (p=0.50). Data on how vascular complications were managed are not collected in the TVT Registry, but the low rate of life-threatening bleeding suggests that standard techniques such as manual compression, balloon tamponade, and placement of covered stents, when necessary, are being successfully employed.
Stable outcomes were also seen with regard to stroke at 30 days, with a 6.3% unadjusted rate in the entire cohort, similar to a 6.3% rate seen in our previous analysis of earlier data from the TVT Registry4. In contrast, recent meta-analyses have demonstrated a 30-day stroke rate of approximately 2-4% in transfemoral TAVR with both balloon-expandable and self-expanding valves202122. There are patient factors likely contributing to a higher stroke rate in the population undergoing TAx rather than transfemoral TAVR, such as an increased burden of atherosclerotic disease (thus precluding use of femoral access) and vessel diameter, which affects the risk of vertebral artery occlusion with sheath insertion. However, potentially modifiable procedural factors may also play a role, such as left- or right-sided access and the pathway taken by the valve delivery system as it crosses the cerebral vessels. In the only study to examine specifically the association between incidence of stroke and access side during TAx TAVR, all 6 strokes occurred in patients with left-sided access (3 via a percutaneous axillary access and 3 via a subclavian cutdown); however, there was insufficient power to determine whether this was a statistically significant difference10. Although they have not been shown to reduce the rate of ischaemic cerebral lesions in broader populations of patients undergoing TAVR2324, it would be beneficial to study the routine use of cerebral embolic protection devices in this particular cohort at increased risk of stroke.
The significantly higher rate of pacemaker insertion in patients undergoing surgical cutdown in the propensity-matched as well as the instrumental variable analysis is puzzling. The decline in pacemaker implantation rates in patients undergoing percutaneous TAx TAVR in the later observation period from 2018 to 2020 suggests that programmes favouring percutaneous access changed their procedural approach to decrease valve implant depth over time, whereas those favouring surgical cutdown did not. Analysis of the broader patient population undergoing transfemoral TAVR at hospitals performing TAx access solely by surgical cutdown showed a persistently higher rate of permanent pacemaker implantation at 30 days, which may reflect systematic differences in implant technique at these centres. Another potential explanation is that surgical cutdown for TAx access may inadvertently lower the operator’s threshold for immediate implantation of a pacemaker in those who develop intraoperative complete heart block25.
Limitations
This study has several limitations. These findings are derived from observational registry data with procedural and outcome data that have not undergone central adjudication. Since sites voluntarily report outcomes to the registry on a quarterly basis, data extracted from November 2020 up to and including February 2021 may not yet include information from all participating sites. Additionally, TVT Registry data do not include certain technical details that may impact on procedural outcomes, such as differentiation between the use of the right as compared to the left axillary artery. Given the generally less favourable angle of take-off between the aorta and the right subclavian/axillary artery, there may be lower procedural success and possibly higher stroke rates associated with use of the right side. Finally, in an effort to isolate the relationship between method of TAx access and outcomes, the scope of this analysis was restricted to the SAPIEN 3 and SAPIEN 3 Ultra valves since they represent the majority of the transcatheter heart valves currently being implanted in the USA.
Conclusions
With increasing use of the axillary artery for alternative access in patients who are not candidates for TF TAVR, there has been increasing application of a percutaneous access strategy. The current study supports the relative safety and efficacy of both a percutaneous and a surgical approach for TAx TAVR. Potential benefits of percutaneous TAx TAVR may include greater use of conscious sedation and less need for the ICU. Further study will refine our understanding of the procedural factors impacting on stroke risk, and can both guide decision making over which alternative access route to utilise, as well as modification of procedural details to minimise that risk to the greatest extent possible. In the absence of a randomised controlled trial of different alternative access methods, the best approach may be for Heart Teams to adopt one alternative access strategy that is best suited to existing technical expertise and to focus on optimising outcomes with that method in these inherently higher risk patients.
Impact on daily practice
Transaxillary access has become the most commonly used alternative access for TAVR in patients with hostile iliofemoral anatomy, with increasing use of an entirely percutaneous approach despite limited data regarding its safety and efficacy compared to traditional surgical cutdown. After propensity score-based matching, rates of all-cause mortality and stroke were similar in patients undergoing percutaneous and surgical access for transaxillary TAVR. Percutaneous access was associated with greater use of conscious sedation, less need for the ICU, and a higher rate of major vascular complications but not life-threatening bleeding.
Acknowledgements
We thank Ke Xu, PhD, James Mun, PhD, and Lynn Griffin, PhD, of Edwards Lifesciences for their editorial and statistical support.
Conflict of interest statement
T. Kaneko, R. Tayal, T. Dahle and J. McCabe report having received consulting honoraria from Edwards Lifesciences. The other author has no conflicts of interest to declare. Statistical analyses were performed by employees of Edwards Lifesciences. The views or opinions presented here do not represent those of the Society of Thoracic Surgeons, the American College of Cardiology, or the STS/ACC TVT Registry.
Supplementary data
To read the full content of this article, please download the PDF.