Abstract
Aims: The goal of the present post hoc analysis of the CLIMA registry was to establish the relationship between calcified nodules (CNs) with (CND) or without (CNWD) disruption of the superficial intimal fibrous layer and one-year occurrence of target lesion myocardial infarction (MI) and/or cardiac death.
Methods and results: CND and CNWD were identified based on the presence or absence of superficial irregularities indicative of disruption of the intimal fibrous layer, with possible overlying local thrombus. In total, 222 CNs were found in the 1,776 non-culprit LAD plaques. CND had larger maximum calcific arc and smaller lumen area. Cardiac death and MI occurred in 20% of patients in the CND group versus 2.7% in the CNWD group and 3.3% in the group without CN (p<0.001). This figure was mainly due to the 13.3% incidence of cardiac death in the CND group versus 2.0% in the CNWD group and versus 2.2% in the group without CN (p<0.001). The presence of CND was confirmed as an independent predictor of events (HR 6.58, 95% CI: 2.7-15.8, p<0.001).
Conclusions: The presence of CND was associated with a high one-year incidence of cardiac death and/or target lesion MI.
Introduction
The presence of calcified nodules (CNs) is an established feature of plaque vulnerability in the coronary region. Based on histology data, over 5% of acute coronary syndromes (ACS) are caused by acute thrombosis occurring at the site of CN1.
CNs are appreciated on optical coherence tomography (OCT) as intraluminal protrusion of calcific components with or without disruption of the intimal fibrous layer. CNs with disruption of the intimal fibrous layer (CND) show an irregular surface on OCT, probably due to overlying thrombus, whilst CNs without disruption of the intimal fibrous layer (CNWD) have a smooth regular surface2,3,4,5,6,7,8. Based on previous OCT reports, CNs may have superficial thrombus apposition, with this feature being more common in the presence of ACS8.
In the CLIMA study, a large prospective registry on plaque vulnerability assessed by means of OCT, patients with CNs tended to develop hard cardiac events more frequently, including acute myocardial infarction (MI) and/or cardiac death, although the difference was not significant9.
The goal of the present post hoc analysis of the CLIMA registry was to study the relationship between calcified nodules with or without disruption of the intimal fibrous layer and the long-term occurrence of hard events (target lesion MI and/or cardiac death).
Methods
AIM AND STUDY DESIGN
The CLIMA study was a prospective observational, multicentre registry recruiting all consecutive patients undergoing assessment of the proximal left anterior descending artery segment by OCT in the context of clinically indicated coronary angiography. The CLIMA study aimed to explore criteria of plaque vulnerability that included minimum lumen area (MLA), fibrous cap thickness (FCT), lipid arc circumferential extension, presence of cluster of macrophages, cholesterol crystals, calcified nodules, intimal vasculature and intraplaque layered tissue.
Outcomes of the CLIMA study were defined according to the Academic Research Consortium guidelines and adjudicated blindly by a clinical events committee; any adverse event or hospitalisation during the follow-up was adjudicated accessing the relative source documents10. The project was approved by the local ethics board and registered in the ClinicalTrials.gov registry (ClinicalTrials.gov identifier: NCT02883088). All patients provided written informed consent for the index procedure, follow-up, and anonymous data management. This work was supported by the Centro per la Lotta contro l’Infarto – Fondazione Onlus (CLI Foundation, Rome, Italy) and the authors were solely responsible for the design, conduct, and final contents of this study.
IMAGING ACQUISITION AND DEFINITION
Coronary angiographies were performed according to the standard techniques and OCT images were acquired by means of the FD C7XR™ system or the OPTIS™ system (both St. Jude Medical, St. Paul, MN, USA) with a non-occlusive technique4,5. The acquired OCT coronary images were analysed off-line using a proprietary OCT console (St. Jude Medical) at an independent imaging core laboratory (Euroimage, Rome, Italy) by blinded expert readers. Only OCT pullbacks allowing accurate measurement of the lumen (continuous arc of at least 270° around the centre of the lumen) and qualitative definition of the superficial plaque components were considered eligible and included in the final analyses. A mandatory inclusion criterion was the adequate OCT assessment of at least 30 mm of naïve proximal segment of left anterior descending artery free from significant stenosis on angiography.
Definitions and cut-offs for OCT parameters were derived from available consensus documents and from the main intravascular ultrasound (IVUS) and OCT studies4,5,11.
Calcium was defined as a signal-poor or heterogeneous region with a sharply delineated outer border. On the basis of criteria established in the OCT consensus document5, CNs were adjudicated in the presence of single or multiple regions of calcium that protruded into the lumen, frequently forming sharp, jutting angles.
Two subgroups of CNs (CND and CNWD) were identified based on the presence or absence of superficial irregularities indicative of disruption of the intimal fibrous layer with possible overlying tissue protrusion indicative of local thrombus4,5,8 (Figure 1).
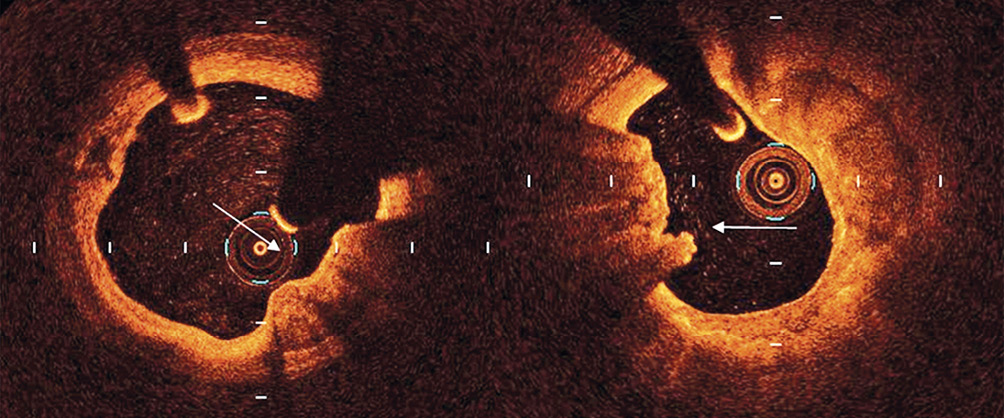
Figure 1. An example of calcified nodule without fibrous layer disruption (arrow in the left panel) and with fibrous layer disruption plus thrombus (arrow in right panel).
Along the selected plaques we analysed plaque morphology applying the definitions utilised in the CLIMA study9. These included: 1) MLA <3.5 mm2, 2) minimum FCT <75 µm, defined as a signal-rich homogeneous band overlying a lipid core and measured at the thinnest portion; 3) lipid plaque (LP) with lipid arc extension >180°, defined as a signal-poor region diffusely bordered by overlying signal-rich bands corresponding to an FC, and 4) presence of macrophage clusters defined on visual estimation as signal-rich, distinct, or confluent punctate regions that exceed the intensity of background speckle noise12.
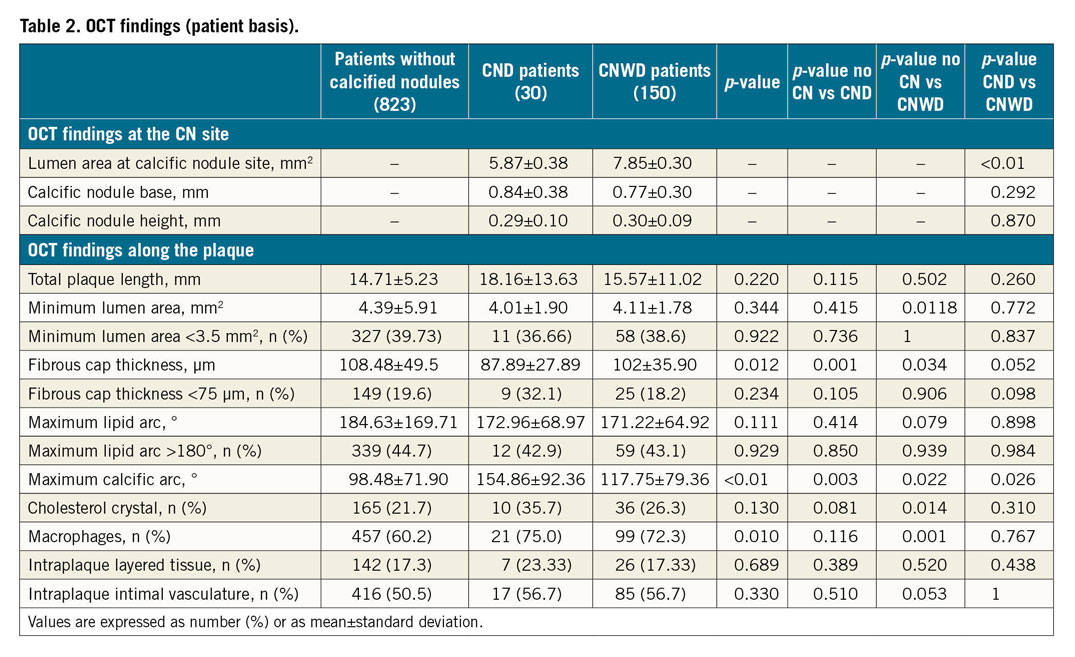
In the presence of CNs the following additional analyses were obtained: 1) lumen area (LA) at the CN site; 2) maximum arc of target lesion calcium measured in degrees with a protractor centred on the lumen at the CN site; 3) measurements of base and height, assuming for CN a trapezoid geometric shape.
STATISTICAL ANALYSIS
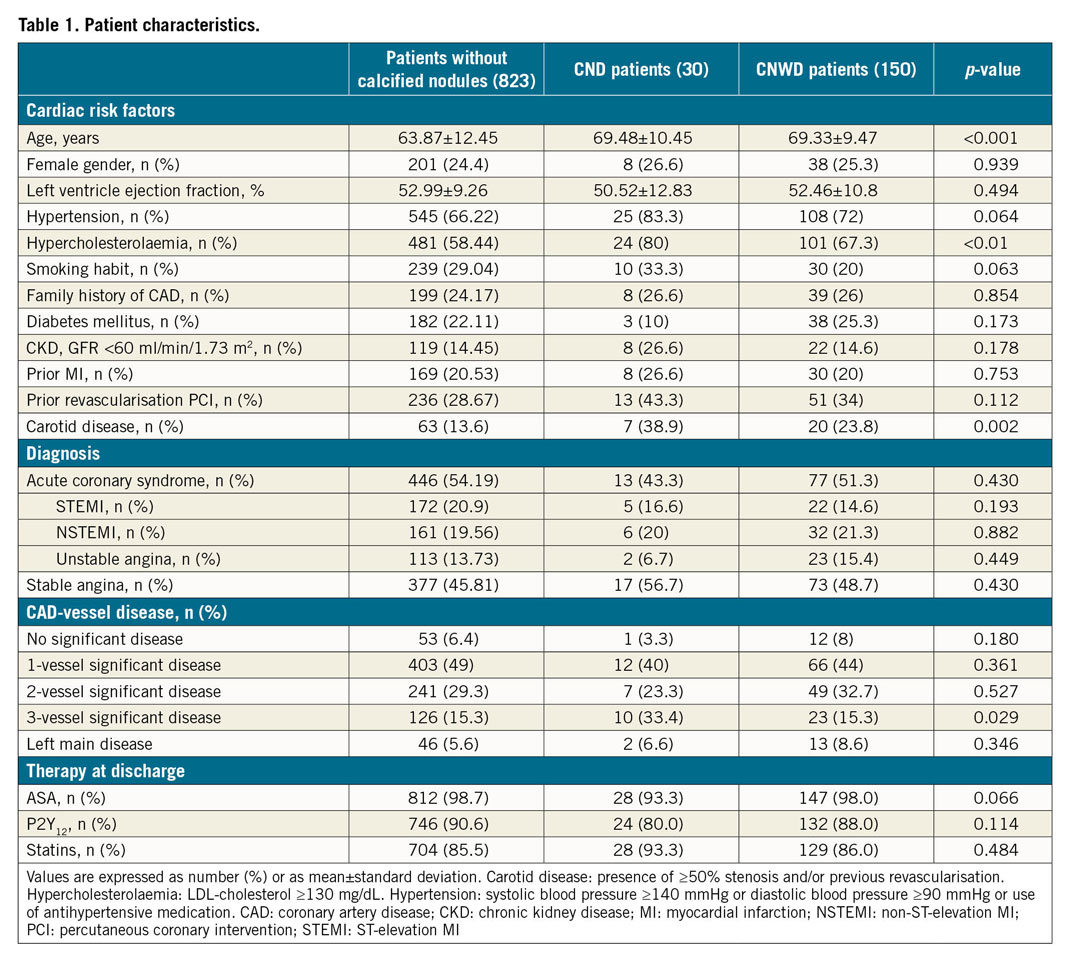
Numbers and percentages were used to report discrete variables, while mean (±standard deviation) was used to describe continuous variables in case of skewed or normal distribution, respectively. The Student’s t-test, Mann-Whitney U test and χ² test were applied for bivariate analyses when appropriate. Clinical endpoints (cardiac death and target lesion anterior MI) were evaluated on a per-patient hierarchical basis, compared with the log-rank test, and summarised as Kaplan-Meier estimates. All variables reported in Table 1 and Table 2 were tested for bivariate association with the composite clinical endpoint and, if nominally significant (p<0.05), were simultaneously forced into a Cox regression model to identify independent outcome predictors and to calculate their adjusted hazard ratios (HRs). Statistical analyses were carried out using SPSS, Version 22.0 (IBM Corp., Armonk, NY, USA), adopting a two-tailed p-value <0.05 for statistical significance.
Results
OCT showed CNs in 180 patients out of 1,003 (17.9%). Thirty patients (3.0%) had at least one CND, 150 (14.9 %) had CNWD, whilst the remaining 823 cases (82.0%) had no CNs.
In total, 222 CNs were found in the 1,776 analysed non-culprit LAD plaques (12.5%). In 146 patients out of 1,003 (14.5%), OCT showed only 1 CN along the analysed LAD segment; in 29 patients (0.3%) OCT identified 2 CNs and in 4 patients (2.7%) 3 CNs. In one case OCT analyses demonstrated 4 CNs. Table 1 shows the demographic and clinical characteristics of the three groups. Patients without CNs were younger, whilst patients with CND were more frequently hypercholesterolaemic.
Regarding the OCT plaque vulnerability criteria tested in the CLIMA study, CND lesions showed a thinner FCT as compared to the CNWD group and the group without CN (87.89±27.89 µm vs 102±35.90 µm vs 108.48±49.5 µm, respectively, p=0.012). Furthermore, plaques with CND showed a significantly smaller lumen area at the CN site, compared to CNWD (5.87±0.38 mm2 vs 7.85±0.30 mm2, p<0.01). This may in part be due to the presence of thrombus that, together with the calcified component, accounts for luminal reduction. No difference in terms of geometric measurements (base and height) was observed between CND and CNWD (Table 2).
The composite incidence of cardiac death and/or target lesion MI occurred in 20% of patients in the CND group versus 2.7% in the CNWD group and 3.3% in the group without CN (p<0.001). This figure was mainly due to the 13.3% incidence of cardiac death in the CND group versus 2.0% in the CNWD group and versus 2.2% in the group without CN (p<0.001) (Table 3).
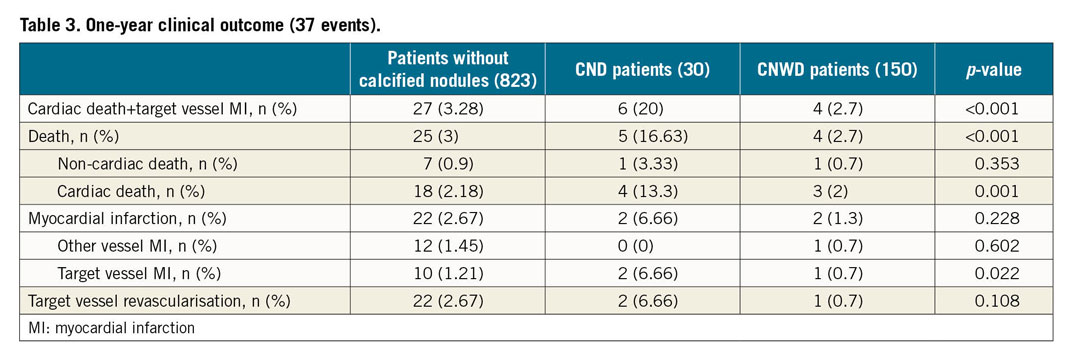
Table 4 shows the OCT characteristics of CN according to the occurrence at one-year follow-up (FU) of the CLIMA hard composite endpoint (target lesion anterior MI and/or cardiac death). The presence of fibrous layer disruption at the CN surface was higher in the patients who experienced the hard endpoint (16.8% vs 2.5%, p<0.001).

Also, after correction for the baseline clinical differences and the single or combined presence of the four CLIMA features of plaque vulnerability, the presence of CND was confirmed as an independent predictor of an event (HR 6.58, 95% CI: 2.7-15.8, p<0.001) (Figure 2).
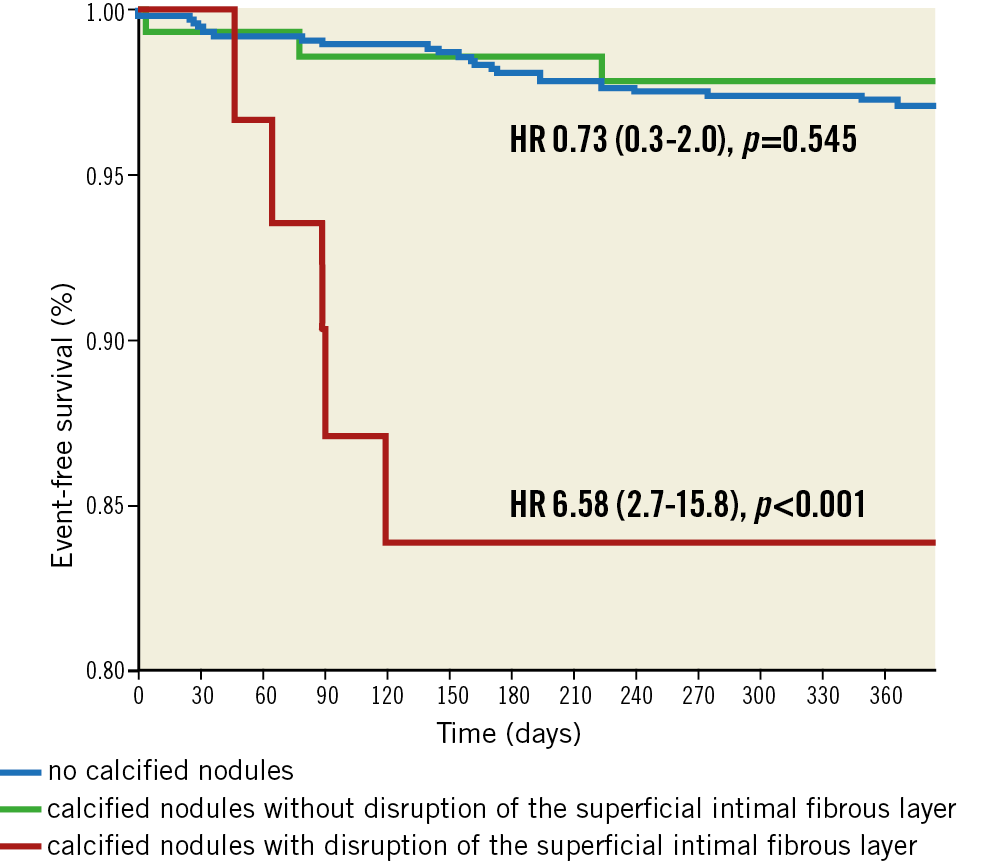
Figure 2. MACE-free survival according to absence versus presence of calcified nodules with or without fibrous layer disruption.
Discussion
The main finding of the present study, conceived as a post hoc analysis of the CLIMA trial, a large prospective registry on 1,003 patients, is that the presence of CND is related to a high incidence of cardiac death and/or target lesion anterior MI at one year, whilst the presence of CNWD does not identify a population at risk of hard endpoints.
Pathology studies of patients dying of sudden coronary thrombosis showed that ACS are caused by calcific nodules in about 5-6% of cases1. Such data have been confirmed in the last decade by OCT studies. OCT, thanks to an axial resolution in the range of 10-20 microns, accurately identifies calcific nodules and differentiates CN with loss of integrity of the intimal fibrous layer and possible superficial thrombus apposition (CND) from those with integrity of the intimal fibrous layer and absence of superficial thrombus apposition (CNWD)3,4. In other words, OCT identifies those CNs on which the thrombus has very likely stratified, due to the loss of the integrity of the intimal layer that covers the CN at the surface, distinguishing them from those with a smooth intimal surface on which thrombotic apposition is not seen.
Jia et al performed OCT in 126 patients with ACS. The prevalence of plaque rupture, OCT erosion, and OCT CN was 43.7%, 31.0%, and 7.9%, respectively6. In more detail, the authors found a 10% prevalence of CN culprit lesions in 50 patients with non-ST-segment elevation ACS and 0% in 54 patients with STEMI. In other OCT studies including only STEMI patients, the prevalence of CN in culprit lesions varied from 3.1% to 8.0%7,13,14. Lee et al compared culprit CN lesions in ACS and stable patients. The prevalence of thrombus was higher in the unstable setting (82.4% vs 20.0%; p<0.001)8.
Unlike previous reports focusing on the prevalence of CN at a single time point, the CLIMA registry prospectively addressed the clinical impact of CN. Our data are consistent with a sub-analysis from the three-vessel PROSPECT imaging carried out with IVUS-virtual histology15. CNs were relatively common, being found in 18% of patients in the PROSPECT trial and in 17.9% in the CLIMA registry. In line with the PROSPECT trial, in the present study the presence of CN was not associated with a greater number of anterior MI and cardiac death at a one-year FU15, being found in 27.0% of patients who experienced hard cardiac events versus 17.6% without, p=0.14, HR 1.73.
ROLE OF INTIMAL FIBROUS LAYER DISRUPTION
The hypotheses on the formation of CN include the possibility of non-plated, irregular growth of plaque calcifications or different remodelling of the calcifications themselves during their formation. This should not be an acute process, especially in cases of large calcifications visible on OCT. CNs are usually covered by a layer of intimal fibrous tissue with overlying endothelium, that is clearly distinguished in OCT images (Supplementary Figure 1). The most likely thrombogenic bases of CNs are related more to the loss of the integrity of the fibrous layer that covers their intimal side than to their acute eruptive protrusions. This may lead to subsequent platelet adhesion and fibrin formation, and finally to thrombus generation. These features, initially described by pathologists1, can be appreciated in vivo applying OCT that is able to characterise superficial plaque components6,16.
Interestingly, we observed for the first time that CND seems to convey a worse clinical outcome than CNWD, with an HR for hard coronary events about eight times higher. OCT, therefore, is potentially able to identify a subgroup of vulnerable lesions with CN.
Based on this assumption, coronary plaques with CN that cause ACS are characterised at an early stage by a limited thrombus formation, which later on may progress to a thrombotic luminal obstruction, the ultimate step of ACS. Alternatively, the presence of CND may be simply a marker of more advanced disease. The fact that CND are observed more often in patients with greater age, triple vessel disease and more common features of plaque vulnerability may support this latter hypothesis. The adoption of a more aggressive medical treatment to stabilise atherosclerosis may be a reasonable solution in this scenario, to be preferred to the interventional treatment of vulnerable lesions.
UTILITY OF A PROSPECTIVE IN VIVO APPROACH
The prospective design of the study enabled exploring the role of CN in the pathophysiology of ACS, applying a different view angle. Unlike previous OCT studies that addressed the morphology of culprit plaques at a single time point in ACS patients, the CLIMA registry made it possible to relate plaque morphology in non-culprit segments to the clinical outcome. Also, intraluminal thrombus, found in the vast majority of ACS culprit lesions, is an obstacle to a precise OCT plaque characterisation and to the differentiation of the two entities of CN (CND and CNWD) which we have applied in the present study. These were the main limitations of single time point OCT studies performed in the unstable clinical setting.
Limitations
In the CLIMA trial and consistently in this post hoc analysis, we have applied a definition of calcified nodules that was suggested in the first OCT consensus document4. Other definitions have been adopted more recently, emphasising the presence of fibrous layer disruption as a distinctive feature that characterises calcified nodules5,6. Regardless of the adopted CN definition, the present prospective data bring evidence that focal regions of calcium protruding into the lumen and accompanied by fibrous layer disruption are found in patients with a worse clinical outcome. By study design, a short one-year observation time was adopted. We observed a high incidence of cardiac death and target lesion anterior MI, with the former being surprisingly high. Longer follow-up data will provide adjunctive understanding of the clinical impact of the loss of integrity of the fibrous layer that covers the intimal side of the CN.
Our study did not require a three-vessel analysis; in fact, only left anterior descending arteries were studied. This was in an effort to promote OCT as a practical and low-risk intracoronary imaging modality to be applied in clinical practice.
Consistent with other studies on plaque vulnerability, it was not possible to relate cardiac death to a culprit lesion. However, even in cases where target lesions were not responsible for the fatal event, the presence of CND served as a marker of more advanced disease.
According to pathological and OCT studies, CN is found more often in the mid right coronary artery where coronary torsion stress is maximum. However, this aspect does not seem to affect the study conclusions that establish a relation between the presence of CND and worse clinical outcome.
Conclusions
In a post hoc analysis of the CLIMA study, the presence of CNs with loss of integrity of their fibrous intimal layer was found to be associated with a high one-year incidence of cardiac death and/or target lesion MI.
|
Impact on daily practice Calcified nodules with disruption of fibrous layer can be easily identified using OCT, a high-resolution invasive imaging modality. The presence of calcified nodules with disruption is related to a higher risk of clinical endpoints and is therefore a relatively uncommon marker of plaque-patient vulnerability. |
Funding
This study was supported by a grant from the Centro per la Lotta contro l’Infarto – Fondazione Onlus, Rome, Italy. The study was endorsed and supported by the CLI Foundation.
Conflict of interest statement
F. Prati has served as a consultant for Abbott/St. Jude and Amgen. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.