Recently developed intracoronary imaging techniques allow real-time, in vivo identification of lipid in atherosclerotic plaques. Optical coherence tomography (OCT), a light-based imaging technique with high axial resolution (10-20 μm), identifies lipid-laden plaques as signal-poor regions with diffuse borders. A validation study performed versus histopathology confirmed the high sensitivity (90% to 94%) and specificity (90% to 92%) of OCT to identify lipid-laden plaques1. Near-infrared spectroscopy (NIRS) detects lipid-laden plaque by analysing light absorption that varies depending on the coronary tissue components and the wavelength of the incident near-infrared light. NIRS displays the probability of the presence of lipid-laden plaque on a colour scale from red (0%) to yellow (100%) as a chemogram. The methodology of NIRS for detecting lipid-laden plaque was established in a rigorous, histopathological validation study, confirming the accuracy of spectroscopy in detecting plaques with markedly different lipid content2. Limitations pertain to differences between ex vivo validation and the clinical use of intracoronary imaging devices.
Present study
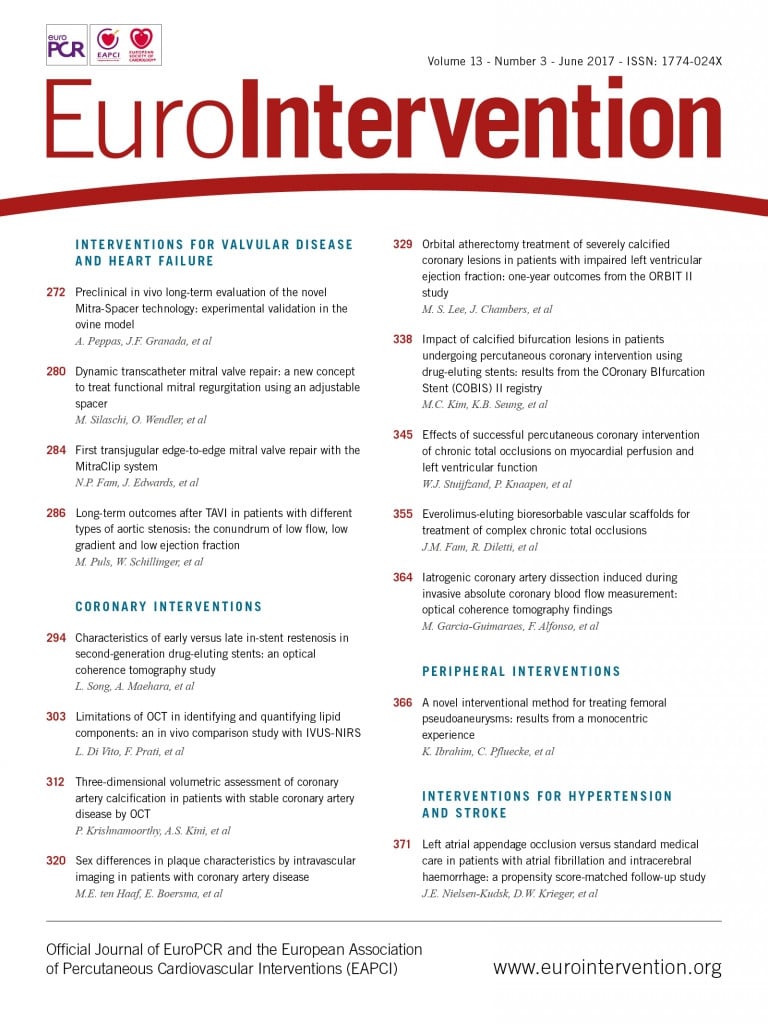
In the current issue of EuroIntervention, Di Vito et al3 report the limitations of OCT for identifying lipid-laden plaque as compared with NIRS in living patients.
The authors demonstrated that the ability of OCT for identifying NIRS-derived lipid-laden plaque was suboptimal. In fact, the presence of macrophage accumulations and superficial calcifications negatively affected lipid identification with OCT.
OCT and NIRS-IVUS for lipid identification
The difference in the process for identifying lipid-laden plaques might contribute to the suboptimal agreement between OCT and NIRS. In OCT, observers qualitatively identify lipid-laden plaque in the monochrome cross-section images of coronary arteries according to the interpretation criteria. The interobserver and intraobserver agreements in OCT for lipid-laden plaques are high (k=0.88 and k=0.91, respectively) if experienced observers perform the interpretation of the images1. However, to be consistent, the interpretation of OCT images requires a lot of skill and training, and this is a fundamental limitation of current OCT images. On the other hand, NIRS automatically provides the probability of the presence of lipid-laden plaque. The algorithm for calculating the probability of the presence of lipid-laden plaque was established by using histology samples with a lipid core >60 degrees in circumferential extension, >200 μm thick, and with a fibrous cap mean thickness of <450 μm2. The minimum cap thickness of lipid core plaques assessed by NIRS was 164 μm (IQR 101-243 μm). In this setting, the AUC value obtained for detection of localised lipid core plaques by NIRS was 0.80 (95% CI: 0.76-0.85), with major causes of false positive NIRS signals being lipid core plaques over smaller fibroatheroma or in the presence of a thicker cap.
The depth of lipid core is an important factor for determining plaque vulnerability. OCT allows accurate measurement of fibrous cap thickness overlying lipid core plaques. In contrast, NIRS cannot provide direct information on the fibrous cap thickness but only an indirect index based on signal attenuation, confounded in the clinical setting by interposed blood. Lack of structural information on lipid-laden plaque is the major limitation of NIRS.
Similarly, lipid identification with OCT is often disturbed by the presence of confounding signals (e.g., macrophages, calcifications and thrombi)4. Macrophage accumulations on the plaque surface appear as a bright line with backshadow. Observers may then misdiagnose this region as a lipid-laden plaque. Superficial calcium makes it difficult to diagnose the neighbouring lipid core because both calcium and lipid exhibit signal-poor regions and the boundary between the two tissues is vague. Intraluminal or mural thrombi disturb the precise assessment of plaque tissue characteristics due to light signal attenuation by red blood cells, platelets and fibrin. Unlike OCT, NIRS is less significantly affected by plaque content and blood cells. Therefore, NIRS may be able to detect lipid core more precisely than OCT, particularly in plaques with macrophages, calcifications or thrombi. However, besides a large lipid core and a thin fibrous cap, inflammation has to be detected and precisely measured to characterise a vulnerable plaque, a missed target for the current generation of intracoronary imaging devices.
The clinical implications of lipid identification by OCT and NIRS are becoming increasingly obvious. OCT-derived lipid-laden plaque is associated with a high risk of subsequent plaque progression, no-reflow immediately after percutaneous coronary intervention (PCI) and late stent-edge restenosis. NIRS-derived lipid-laden plaque is a potential predictor of periprocedural myocardial infarction, presumably due to embolisation of plaque content during PCI. However, to date, there is no clear evidence reporting a high predictive value of OCT- and NIRS-derived lipid-laden plaques for subsequent plaque rupture and coronary thrombosis.
OCT and NIRS each have inherent strengths and weaknesses for identifying lipid. Suboptimal agreement between OCT and NIRS for identification of lipid-laden plaque suggests the possibility that these two techniques provide distinct information and complement each other. Thus, the combined use of OCT and NIRS may lead to more precise identification of lipid-laden plaque at high risk of future coronary events. Furthermore, the development of novel hybrid imaging OCT-NIRS catheters may combine the unique high resolution of OCT in the near field with the accuracy of spectroscopy in identifying lipid content to limit mischaracterisation of coronary plaques.
Final remarks
OCT and NIRS are promising techniques capable of identifying lipid-laden plaque in coronary arteries. The information provided by such imaging techniques has many potential uses, such as stratifying the risk of future coronary events, determining the aggressiveness of medical therapy, selecting the optimum stent length and stent type for each coronary lesion, predicting thrombosis and restenosis after PCI, and serving as a surrogate endpoint of trials examining therapies targeting coronary lipid-laden plaque. What will be important in future research is to establish the clinical relevance of lipid-laden plaque identified separately by OCT and NIRS and whether combined imaging devices (OCT+NIRS) may improve diagnostic accuracy for high-risk lesion identification.
Conflict of interest statement
T. Kubo and T. Akasaka have received lecture fees and research funds from Infraredx and St. Jude Medical. G. Guagliumi is a consultant for St. Jude Medical.