Abstract
Background: In-stent restenosis (ISR) is highly prevalent and leads to repeat revascularisation. Long-term implications of ISR are poorly understood.
Aims: This study aimed to evaluate the long-term outcomes of patients undergoing percutaneous coronary intervention (PCI) for ISR.
Methods: National Cardiovascular Data Registry CathPCI records for individuals aged ≥65 years undergoing PCI from July 2009 to December 2014 were linked to Medicare claims. Baseline characteristics and long-term rates of death, myocardial infarction (MI), repeat revascularisation including target vessel revascularisation (TVR), and major adverse cardiovascular and cerebrovascular events (MACCE) were compared between ISR PCI versus de novo lesion PCI.
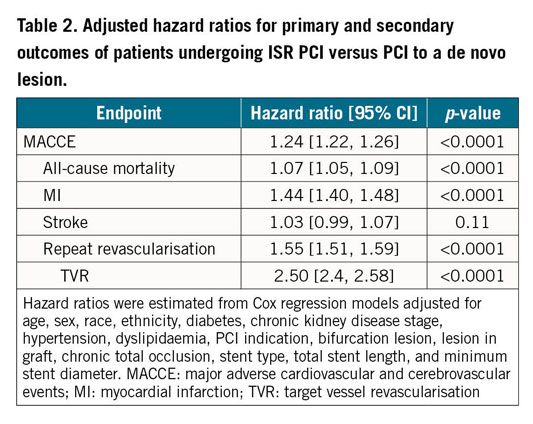
Results: Of 653,304 individuals, 10.2% underwent ISR PCI and 89.8% underwent de novo lesion PCI. The median duration of follow-up was 825 days (quartile 1: 352 days–quartile 3: 1,379 days). The frequency of MACCE (55.6% vs 45.0%; p<0.001), all-cause mortality (27.8% vs 25.5%; p<0.001), MI (19.0% vs 12.3%; p<0.001), repeat revascularisation (31.9% vs 18.6%; p<0.001), TVR (22.4% vs 8.0%; p<0.001), and stroke (8.8% vs 8.3%; p=0.005) was higher after ISR PCI. After multivariable adjustment, ISR PCI remained associated with worse long-term outcomes than after de novo lesion PCI (hazard ratio [HR] for MACCE 1.24 [95% CI: 1.22, 1.26], mortality 1.07 [95% CI: 1.05, 1.09], MI 1.44 [95% CI: 1.40, 1.48], repeat revascularisation 1.55 [95% CI: 1.51, 1.59], and TVR 2.50 [95% CI: 2.42, 2.58]).
Conclusions: ISR PCI was common and was associated with a significantly higher risk of recurrent long-term major ischaemic events compared to patients undergoing de novo lesion PCI. There remains a need for new strategies to minimise ISR.
Introduction
Over half a million percutaneous coronary interventions (PCI) with metallic stents are performed annually in the United States of America (USA)1. These patients are at risk of in-stent restenosis (ISR) and development of recurrent symptoms. The incidence rate of ISR is reported to be between 5% and 20% with drug-eluting stents (DES) five years post procedure2,3,4.
Despite improvements in short-term outcomes after DES placement, including low rates of stent thrombosis and one-year target vessel failure (TVF), patients receiving these stents have persistently rising rates of TVF over the long term5,6. Furthermore, the presence of stents may impact on future interventions such as repeat stenting and coronary artery bypass graft (CABG) surgery.
Despite the high annual number of PCIs performed worldwide, there is a poor understanding of the burden of ISR and the long-term outcomes associated with ISR PCI. In this study, we evaluated the frequency of ISR PCI in a large representative sample of older adults in the USA, the patient and procedural characteristics, and the associated long-term outcomes.
Methods
STUDY POPULATION
Procedures in the American College of Cardiology National Cardiovascular Data Registry CathPCI Registry were considered for inclusion7. This registry includes data on PCIs from ~1,400 US catheterisation laboratories. Data elements are prospectively acquired using standardised forms and definitions.
Our analysis included all PCIs performed among patients aged ≥65 years between July 2009, the date of implementation of Version 4 of the CathPCI data collection form, and December 2014. Patients who underwent salvage PCI or presented with cardiogenic shock or cardiac arrest were excluded, as they have high mortality unrelated to their lesion characteristics. In patients with multiple PCIs, the first procedure was the index procedure. Patients were categorised as undergoing PCI for ISR if 1) the index lesion was identified as a restenotic lesion, and 2) they had a documented history of prior PCI in the CathPCI Registry.
To obtain long-term outcomes, patients were linked to centres for Medicare and Medicaid services (CMS) fee-for-service beneficiary claims data based on social security number, date of birth, and sex. Claims up to 31 December 2015 were used to ensure that each patient had ≥1 year of follow-up. CMS provides health insurance coverage for the majority of adults aged ≥65 years in the USA, and these claims data have been extensively used for health outcomes research.
COVARIATES AND OUTCOMES
The primary exposure was PCI for ISR versus PCI for a de novo lesion. These variables are specified in the CathPCI data collection instrument and are site reported. Covariates included demographic characteristics (including age, sex, and race/ethnicity), prior medical history (including diabetes mellitus, current dialysis, hypertension, and dyslipidaemia), and procedural and lesion characteristics (including PCI indication, bifurcation lesion, lesion in graft, chronic total occlusion, stent type, total stent length, and minimum stent diameter).
The primary outcome was the occurrence of major adverse cardiovascular and cerebrovascular events (MACCE), defined as the composite of death from any cause, MI, stroke and repeat revascularisation. Validated International Classification of Diseases, Ninth Revision codes were used to identify these endpoints (Supplementary Table 1),8,9,10. Secondary outcomes included the component outcomes of mortality, MI, repeat revascularisation (any vessel), target vessel revascularisation (TVR), and stroke. We extracted information on TVR by re-linking repeat revascularisation events found in CMS data to corresponding entries in the CathPCI Registry. We defined TVR as repeat PCI in a major epicardial vessel territory (left main, left anterior descending, left circumflex or right coronary artery) treated during the index admission.
STATISTICAL ANALYSIS
Baseline patient and procedural characteristics were obtained from the CathPCI Registry and compared using standardised differences. We used the Kaplan-Meier method to estimate the cumulative incidence of the primary and secondary outcomes and used the log-rank statistic to compare the differences between groups. A Cox proportional hazards regression model that included possible confounders selected a priori (age, sex, race, ethnicity, diabetes, chronic kidney disease stage, hypertension, dyslipidaemia, PCI indication, bifurcation lesion, lesion in graft, chronic total occlusion, stent type, total stent length, and minimum stent diameter) was used to perform an adjusted time-to-event analysis. A robust sandwich covariance matrix estimate was applied to account for the intracluster dependence of patients nested in hospitals.
Because patients with ISR PCI have a longer history of known coronary disease compared with those undergoing de novo lesion PCI, we performed a sensitivity analysis restricting the de novo lesion PCI group to patients with a history of prior PCI in another vessel. Additional subgroup and sensitivity analyses are provided in Supplementary Appendix 1. Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
The institutional review board of the Beth Israel Deaconess Medical Center exempted this study from review.
Results
BASELINE CHARACTERISTICS
Of the 3,017,110 patients who had a PCI between July 2009 and December 2014, 1,568,783 (52.0%) were aged ≥65 years (Figure 1). The main reasons for exclusion (4.5% of patients) were salvage PCI (0.4%), presence of cardiogenic shock (2.9%), cardiac arrest (0.9%) and inconsistent documentation of ISR PCI (ISR PCI listed at index but no prior history of PCI [0.3%]). Fifty-six percent of the remainder of patients were unable to be linked to CMS: 20.9% were enrolled in Medicare Advantage plans which are privately administered health plans for which fee-for-service data were not available, and 35.5% did not have sufficient data to be linked. The final cohort included 653,304 patients (Figure 1). There were no clinically significant differences between linked and non-linked patients (Supplementary Table 2).
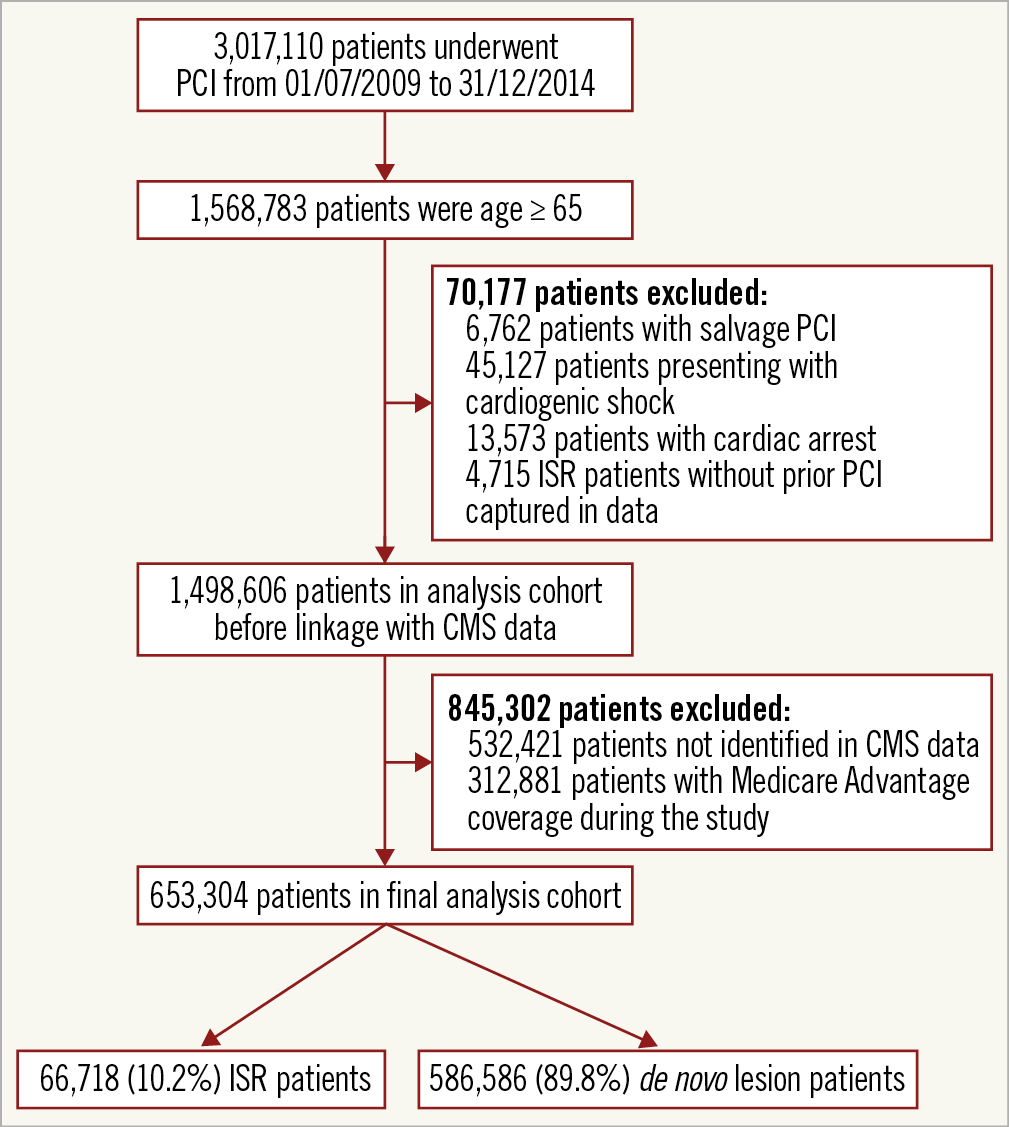
Figure 1. Study flow diagram.
Among this cohort, 66,718 patients (10.2%) underwent PCI for ISR and 586,586 (89.8%) underwent PCI for a de novo lesion. Patients undergoing ISR PCI were more likely to have diabetes mellitus (43.1% vs 36.1%), dyslipidaemia (92.7% vs 79.8%), prior MI (50.4% vs 24.7%) and prior CABG (30.6% vs 21.0%) compared to patients undergoing PCI to de novo lesions (Table 1). The frequency table by stent characteristics is shown in Supplementary Table 3.
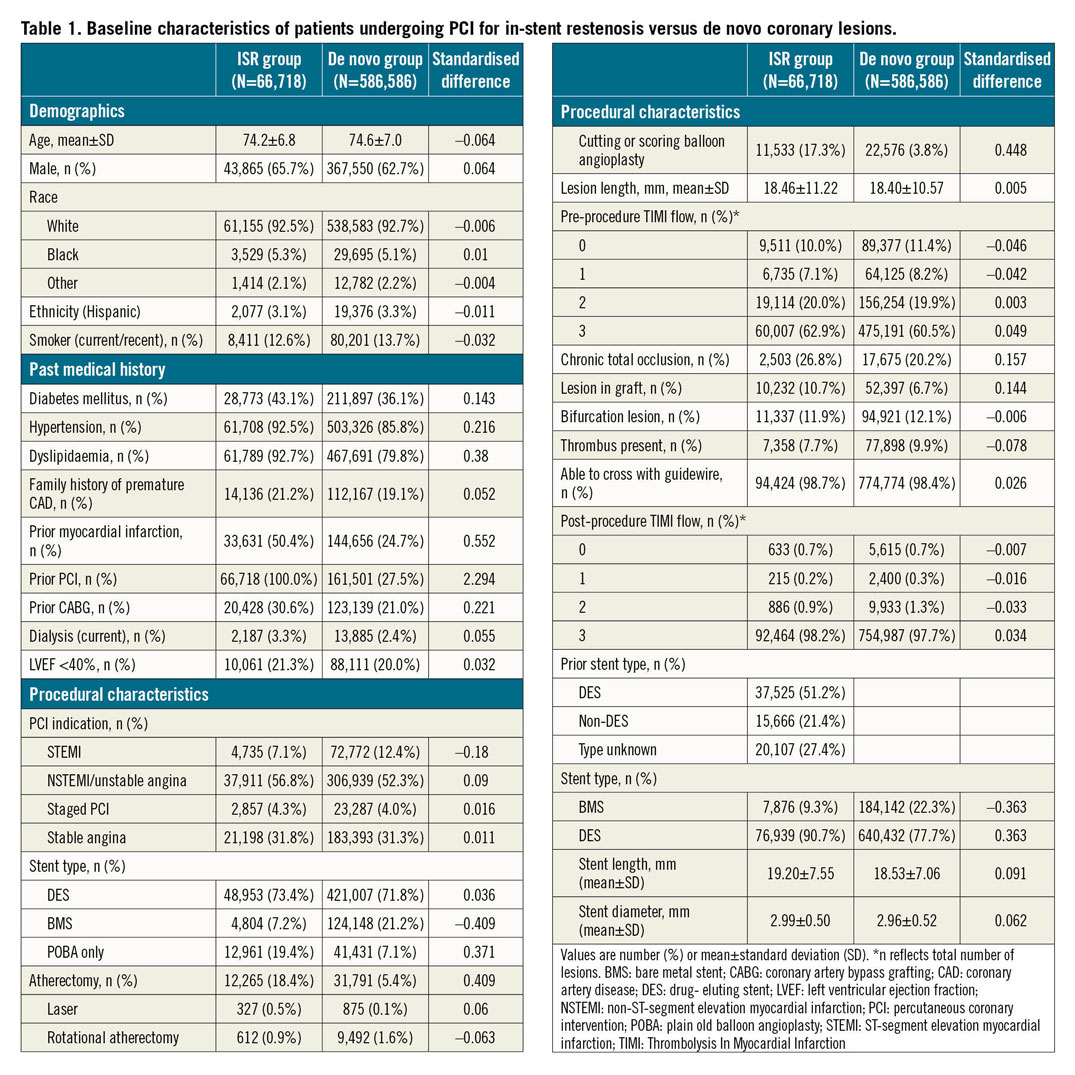
PROCEDURAL CHARACTERISTICS
Presentation with ST-elevation MI was less common in patients undergoing ISR PCI (7.1%) versus de novo lesion PCI (12.4%). Bare metal stents (BMS) were used in 7.2% of patients with ISR versus 21.2% of patients with de novo lesions; plain old balloon angioplasty was more common in patients with ISR (19.4%) versus de novo lesions (7.1%). Cutting or scoring balloon use was more frequent in patients with ISR (17.3%) versus de novo lesions (3.8%). Use of laser or rotational atherectomy was similar between groups. There was no difference in the ability to cross with a guidewire between groups.
UNADJUSTED COMPARISONS OF OUTCOMES AFTER ISR PCI AND DE NOVO LESION PCI
The median duration of follow-up was 825 days (quartile 1: 352 days–quartile 3: 1,379 days). The cumulative incidence of all-cause rehospitalisation at 30 days was 10.3% in the ISR group and 10.6% in the de novo lesion PCI group (p=0.02), and at 90 days was 20.4% in the ISR group and 20.3% in the de novo lesion PCI group (p=0.87). Patients undergoing ISR PCI had a higher cumulative incidence of MACCE compared to those undergoing de novo lesion PCI (55.6% vs 45.0% at 4 years; p<0.001) (Figure 2). There was a higher cumulative incidence of all secondary outcomes at 4 years in patients undergoing ISR PCI compared to those undergoing PCI to de novo lesions: all-cause mortality (27.8% vs 25.5%; p<0.001), MI (19.0% vs 12.3%; p<0.001), repeat revascularisation (31.9% vs 18.6%; p<0.001), TVR (22.4% vs 8.0%; p<0.001), and stroke (8.8% vs 8.3%; p=0.005). Definite stent thrombosis requiring PCI in the same vessel as index PCI was 1.98% in the ISR group and 0.43% in the de novo group (p<0.001). For the results of the ISR subgroup comparisons, see Supplementary Figure 1 for primary and secondary outcomes in the ISR group stratified by time to ISR, and Supplementary Figure 2 for the cumulative incidence of events after PCI for ISR of different vessels.
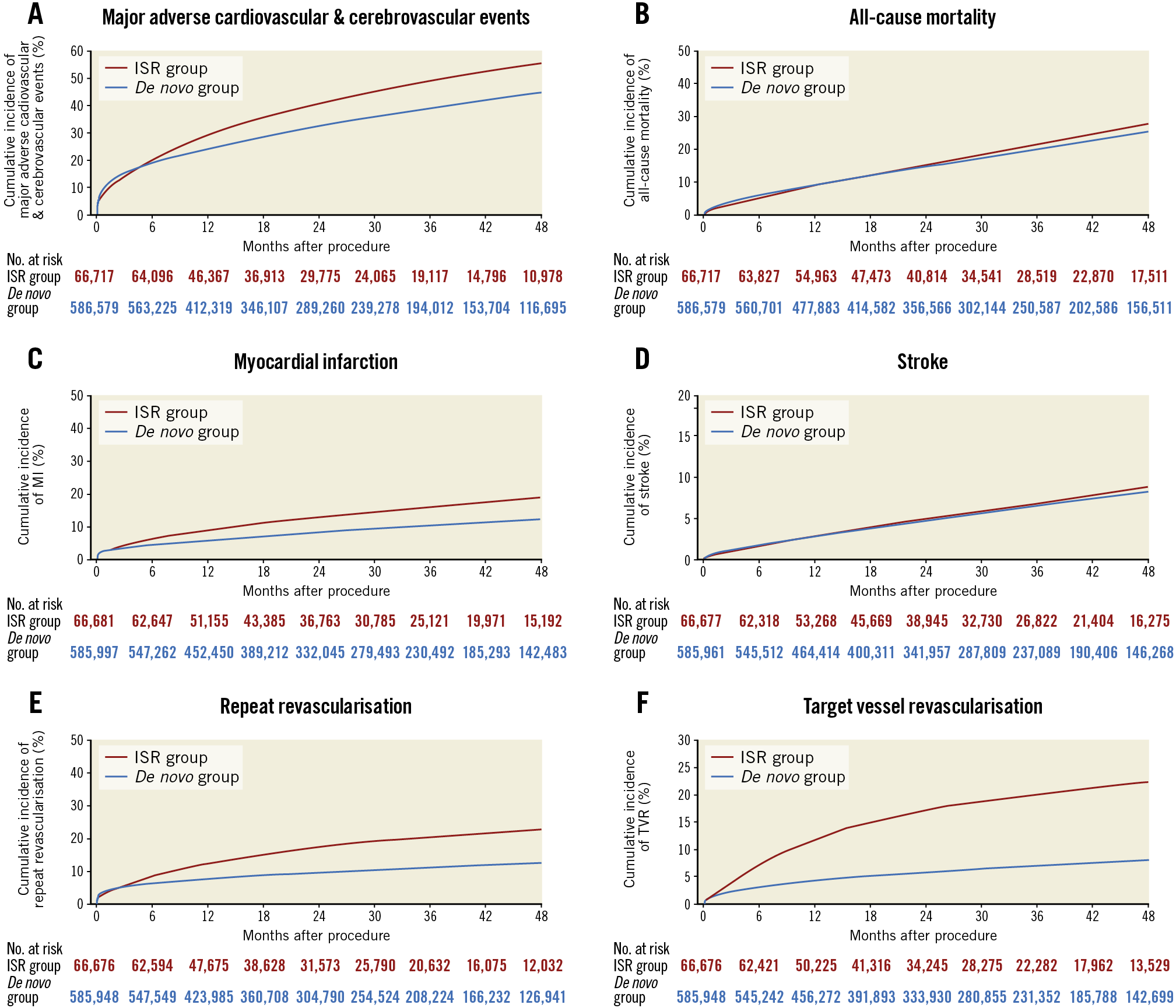
Figure 2. Cumulative incidence of primary and secondary outcomes in patients undergoing ISR PCI and de novo lesion PCI. The cumulative incidence of major adverse cardiovascular and cerebrovascular events (A), all-cause mortality (B), myocardial infarction (C), stroke (D), repeat revascularisation (E) and target vessel revascularisation (F) in patients undergoing ISR PCI (red line) versus de novo lesion PCI (blue line).
ADJUSTED COMPARISON OF OUTCOMES AFTER ISR PCI WITH DE NOVO PCI
Multivariable adjustment showed that patients undergoing ISR PCI had an increased hazard of MACCE (hazard ratio [HR] 1.24 [95% CI: 1.22, 1.26]; p<0.001) (Table 2) versus de novo lesion PCI. Most components of MACCE were increased in patients undergoing ISR PCI compared with de novo lesion PCI, including all-cause mortality (1.07 [95% CI: 1.05, 1.09]; p<0.001), MI (1.44 [95% CI: 1.40, 1.48]; p<0.001), repeat revascularisation (1.55 [95% CI: 1.51, 1.59]; p<0.001) and TVR (2.50 [95% CI: 2.42, 2.58]; p<0.001). Adjusted rates of stroke were not significantly different between groups (1.03 [95% CI: 0.99, 1.07]; p=0.11). Findings were similar after excluding patients with unknown prior stent type (Supplementary Table 4).
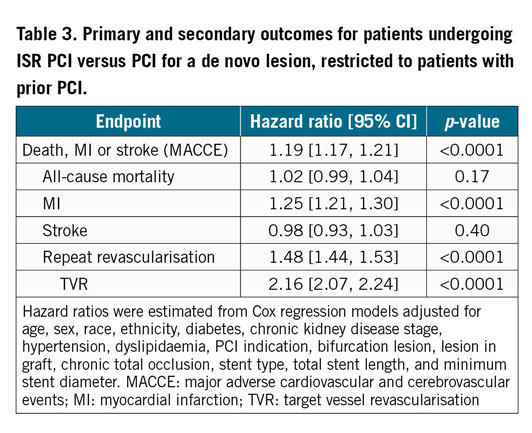
COMPARISON OF DE NOVO AND ISR PCI OUTCOMES AMONG PATIENTS WITH PRIOR PCI
After restricting the population to patients with a history of prior PCI in any vessel, baseline characteristics between groups were similar (Supplementary Table 5). Procedural characteristics included similar indications for PCI, lower BMS use (7.2% vs 17.0%) and higher use of cutting and scoring balloon angioplasty (17.3% vs 4.7%) in the ISR PCI versus the de novo lesion PCI group. The cumulative incidence of MACCE, all-cause mortality, MI, stroke, repeat revascularisation, and TVR is shown in Figure 3.
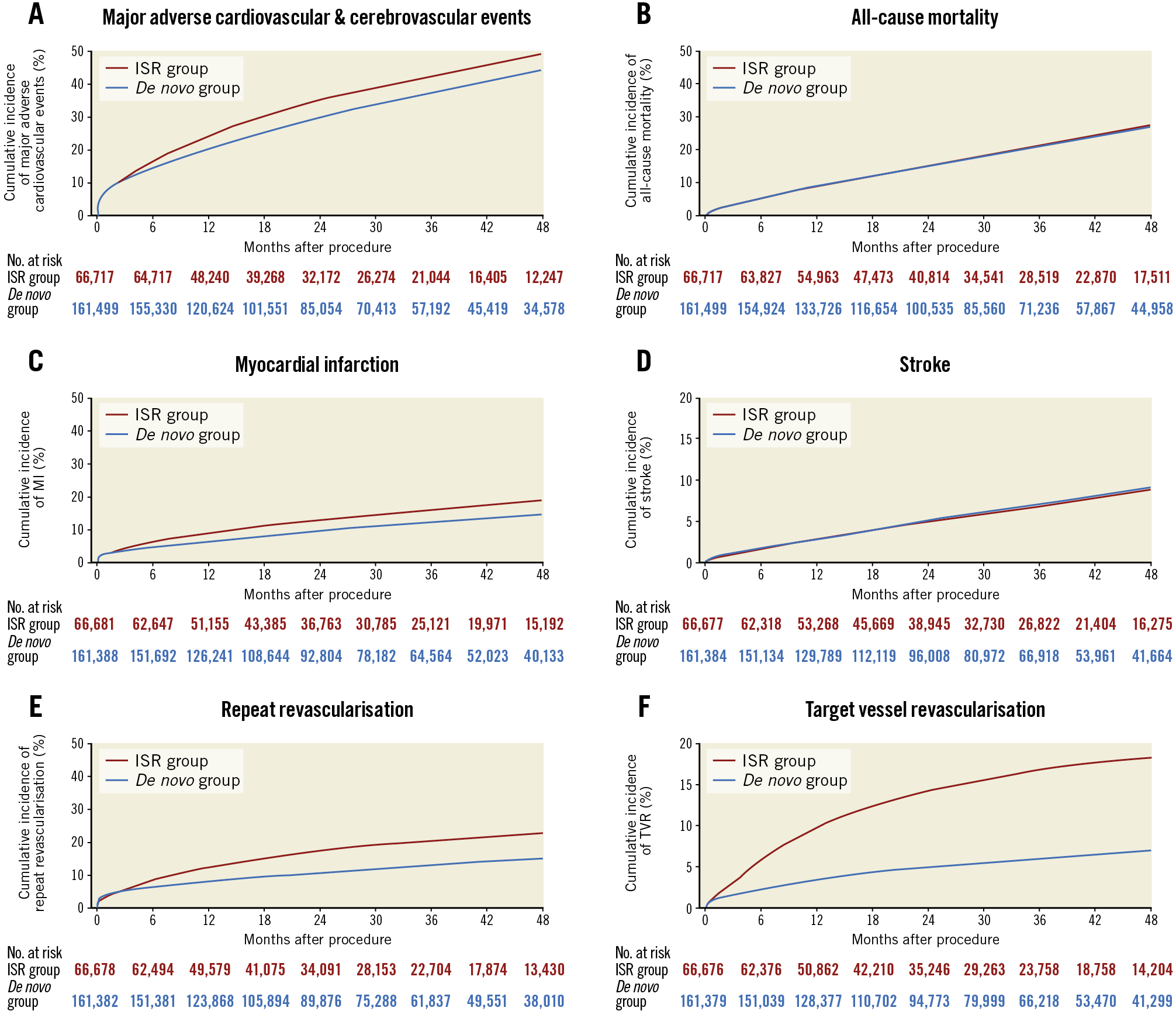
Figure 3. Cumulative incidence of primary and secondary outcomes in patients undergoing ISR PCI and de novo lesion PCI with history of prior PCI. The cumulative incidence of major adverse cardiovascular and cerebrovascular events (A), all-cause mortality (B), myocardial infarction (C), stroke (D), repeat revascularisation (E) and target vessel revascularisation (F) in patients undergoing ISR PCI (red line) versus de novo lesion PCI (blue line).
Multivariable adjustment showed an increased hazard of MACCE (1.19 [95% CI: 1.17, 1.21]; p<0.001), MI (1.25 [95% CI: 1.21, 1.30]; p<0.001), repeat revascularisation (1.48 [95% CI: 1.44, 1.53]; p<0.001), and TVR (2.16 [95% CI: 2.07, 2.24]; p<0.001), in patients undergoing ISR PCI compared to patients undergoing PCI to a de novo lesion in the group with a prior history of PCI (Table 3). There continued to be no significant difference in all-cause mortality (1.02 [95% CI: 0.99, 1.04]; p=0.17) or stroke (0.98 [95% CI: 0.93, 1.03]; p=0.40) between groups after adjustment.
Supplementary Appendix 2 shows the results of the ISR subgroup comparisons (outcomes for patients undergoing ISR PCI vs PCI to a de novo lesion adjusted for stent type used for the initial PCI [Supplementary Table 6]; baseline characteristics by treatment in ISR group [Supplementary Table 7]; outcomes for ISR patients treated with BMS or plain old balloon angioplasty vs DES [Supplementary Table 8]; ISR patient characteristics by stent type in the initial PCI [Supplementary Table 9]; outcomes for ISR patients with BMS vs DES in the initial PCI [Supplementary Table 10]; patient characteristics in a propensity matched cohort [Supplementary Table 11]; outcomes for ISR patients and de novo lesion PCI patients in a propensity matched cohort [Supplementary Table 12]).
Discussion
In this large national study of older US patients undergoing PCI based on a registry linked to long-term claims data for follow-up, we observed that PCI for ISR is strongly associated with worse long-term outcomes, including higher risk of MACCE, MI, repeat revascularisation, and TVR. To our knowledge, this is the first study evaluating long-term outcomes after ISR PCI using modern stent technologies in a large, comprehensive sample of elderly PCI patients in the USA. It highlights the importance of recognising the occurrence of restenosis as a prognostically meaningful event. Previous studies have used small cohorts and were designed to compare different stent iterations11,12,13,14,15 or to compare drug-coated balloons with stents16,17,18.
Not surprisingly, baseline characteristics differed between the groups, with patients who underwent ISR PCI having a higher prevalence of comorbidities. To minimise confounders, we performed an adjusted analysis and a subgroup analysis restricting the cohort to patients with a history of prior PCI, which ameliorated the differences in baseline characteristics. The association between ISR PCI and increased rates of MI and repeat revascularisation, including TVR, persisted even after this restriction, but there was no longer a difference in all-cause mortality or stroke. A small difference in all-cause mortality was still seen in the propensity-matched population. This could indicate that patients undergoing ISR PCI and PCI to a de novo lesion have significant differences in unmeasured confounders that are not captured by our multivariable or propensity score models. The similar mortality rates after matching on prior PCI suggest that, although ISR PCI portends a worse prognosis with regard to the need for subsequent procedures, this may not influence more meaningful clinical outcomes such as death.
We also found that ISR PCI of a previously placed DES versus BMS was associated with more frequent subsequent MI and repeat revascularisation. This may be because patients with previously placed BMS had higher mortality, which may reflect that they are sicker and less likely to receive future invasive treatment. It is also plausible that patients who develop restenosis in a DES have more aggressive coronary disease than those with restenosis of a BMS. This is consistent with a recent meta-analysis which found higher rates of treatment failure in the treatment of ISR of a DES than ISR of a BMS19.
The cumulative frequency of repeat revascularisation nearly doubled in patients undergoing ISR PCI compared with de novo lesion PCI. Most repeat revascularisations were explained by TVR (70% in ISR PCI vs 43% in de novo lesion PCI). The cumulative frequencies of MACCE and TVR were higher than described in randomised trials16,20. In a recent meta-analysis including data on >25,000 patients in randomised trials of metallic stents, patients were younger (62 vs 74 years) and had fewer comorbidities compared to our cohort. The five-year MACCE rate was lower in their study (9.4%) as compared to ours (45% in the de novo lesion PCI group and 55.6% in the ISR PCI group)20. Although our study was limited to older adults by design, these findings underscore how trial outcomes may differ from those in real-world practice.
Our study has important clinical implications. First, despite the technological advances of newer DES with lower incidence of ISR and the general impression of restenosis being benign, our study shows increased morbidity among patients who undergo ISR PCI. Our findings reinforce the importance of using all techniques available to reduce ISR, including adequate stent expansion and apposition and maximising luminal area13,21. Furthermore, use of intracoronary imaging can help to corroborate adequate lesion preparation and stent expansion before deployment of a second layer of stent, and has been shown to decrease the rate of MACCE22. Lastly, optimal medical therapy, novel stent technologies, and the emergence of drug-coated balloons may decrease the rate of ISR and change its treatment. Further research is needed to demonstrate whether improved treatments for restenosis can mitigate some of the late clinical events associated with ISR, and thus demonstrate that ISR is not only a strong marker of severe and aggressive coronary artery disease, but also causal of adverse outcomes.
Limitations
Our study has several limitations. This is an observational study so we cannot be certain that the association between restenosis and subsequent events is causal, and events may be missing or misclassified. Due to the nature of the data, for patients who underwent PCI to several vessels during the index procedure, we cannot distinguish which vessel had TVR, and we cannot determine if repeat revascularisation in the target vessels occurred in the same lesion. Similarly, because the data set lacks information on all prior PCIs for patients with ISR, other modelling approaches such as treating ISR PCI as a time-dependent covariate were not possible. Furthermore, MI could not be attributed to the treated lesion. We cannot rule out the potential for residual confounding, and we were unable to adjust for variables that were not present in the data. However, after limiting the de novo lesion PCI population to those with prior PCI in remote vessels, baseline characteristics between groups appeared balanced. Our study excluded 4,715 patients for whom we lacked information about prior PCI, and we were unable to link a large fraction of individuals in the CathPCI database to CMS claims. However, there were no clinically significant differences in measured variables between the linked and non-linked groups. Finally, we do not have information on concomitant medications which could differ and influence event rates between groups.
Conclusions
Patients who undergo ISR PCI are at higher risk of MACCE, MI, and repeat revascularisation, particularly of the target vessel, compared with patients undergoing PCI to de novo lesions. Novel devices and techniques to prevent the occurrence of restenosis and improve its treatment are needed.
|
Impact on daily practice Patients who undergo PCI for in-stent restenosis are at higher risk of major adverse cardiovascular and cerebrovascular events such as myocardial infarction and the need for repeat revascularisation, including target vessel revascularisation, compared with patients undergoing the procedure for a de novo lesion. Practitioners should be aware of this increased risk and should use all available techniques to prevent the occurrence of restenosis and improve its treatment. |
Funding
This study was funded by an investigator-initiated grant from Abbott Vascular.
Conflict of interest statement
E.A. Secemsky reports grants/personal fees from Medtronic, CSI, Boston Scientific, Philips, Cook Medical, BD Bard, AstraZeneca, Janssen. C.A. Simonton is a former employee of Abbott Vascular, and an employee of Abiomed. C.M. Gibson received research support and consultant fees from Janssen Pharmaceuticals, Johnson and Johnson, Bayer, and Portola, as well as research support from the Baim Institute for Clinical Research. J.J. Popma is an employee of Medtronic and is not affiliated with Beth Israel Deaconess Medical Center. He reports grants from Medtronic, Boston Scientific, Abbott, and Edwards Lifesciences. R.W. Yeh received a research grant, consulting, and advisory board fees from Abbott Vascular, Boston Scientific, and Medtronic. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.