Abstract
Aims: This paper studies in-stent restenosis (ISR) after percutaneous coronary intervention (PCI) following bare-metal stent (BMS) and drug-eluting stent (DES) in all consecutive patients between 2004 and 2007 undergoing PCI for ISR lesions at our centre.
Methods and results: We compared the clinical presentation, pattern and angiographic outcomes in 838 patients with BMS ISR (487) and SES ISR (351). About 18% of the patients presented with acute coronary syndrome with 2% presenting as ST elevation myocardial infarction, similar in both groups. Angiographic pattern was predominantly focal with SES ISR (47%SES ISR vs. 19% BMS ISR; p<0.001) and diffuse with BMS ISR (SES ISR 16% vs. BMS ISR 36%; p=0.003). In our series the use of balloon angioplasty was higher for the treatment of SES ISR patients as compared to BMS ISR (41.6% vs. 18.3%; p<0.001) and the usage of stent was higher in BMS ISR patients (38.6% vs. 23.4%; p<0.001). Angiographic recurrent restenosis with conventional treatment in a consecutive series of patients was 38.6% and target lesion revascularisation was seen in 33.6%. These outcomes were seen slightly higher in SES ISR group (41.1% vs. 36.9%, p=ns). We have identified unstable angina at presentation (OR 3.02; 95%CI: 1.58-5.77, p=0.001), focal pattern of ISR (OR 0.50; 95% CI: .25-.99, p=0.04), stent usage (OR .25; 95% CI .13-.47, p<0.001), and baseline% diameter stenosis (OR1.03; 95%CI: 1.03-1.06, p=0.01) as independent predictors of BMS ISR recurrent restenosis. Unstable angina, focal pattern of ISR, reference vessel diameter, and% diameter stenosis were shown to be independent predictors of SES ISR.
Conclusions: ISR is not a benign condition, and one fifth of the patients presented with acute coronary syndrome. The pattern of restenosis is predominantly non-focal with BMS ISR and focal with SES ISR. Recurrent restenosis rates are high following conventional treatment and further optimal therapies mainly with SES ISR needs to defined.
Introduction
Percutaneous coronary intervention (PCI) has provided a safe and reasonable revascularisation strategy in patients with symptomatic coronary artery disease. Stenting is now performed for a majority of the lesions, and the restenosis rates with bare metal stents (BMS) remains high1,2. Drug eluting stents (DES) have reduced the restenosis rates following BMS in-stent restenosis3-5. With the increasing complexity of cases and off-label use of DES, the restenosis rates with DES are rising and the optimum treatment for DES ISR is not fully defined6-9. The clinical presentation for both BMS in-stent restenosis and DES in-stent restenosis can vary from stable to unstable. There are limited studies in literature comparing the clinical profile and angiographic patterns of BMS and DES in-stent restenosis in contemporary practice.
The purpose of our study is to compare the clinical profile, clinical presentation, risk factors, angiographic patterns, and treatment factors in a consecutive series of in-stent restenosis patients between BMS in-stent restenosis and sirolimus eluting stents (SES) in-stent restenosis.
Methods
Study population
All consecutive patients who underwent treatment for in-stent restenosis between January 2004 and December 2007 at the Toyohashi Heart Centre, Toyohashi, Japan are included in this study. This included all patients with in-stent and stent edge restenosis undergoing treatment. A total of 838 patients underwent treatment for ISR; 487 patients with BMS ISR were compared with 351 patients with SES ISR. All data was prospectively collected, entered in a dedicated database and the present analysis was performed retrospectively. Follow-up angiography was performed routinely at six to nine months, or earlier if clinically indicated, and the results of 625 patients (75%) were available.
PCI procedure
The angioplasty procedure was performed according to the standard techniques exisiting at the time they were performed and the final treatment device was selected on operator’s discretion. During the procedure, patients received weight adjusted dose of heparin to achieve activated clotting time (ACT) >300 sec. All patients were pre-treated with aspirin and ticlopidine and were continued on these agents as per standard procedure. Dual antiplatelet therapy was continued for three months, with the use of balloon angioplasty, rotational atherectomy and bare metal stent implantation. This was continued for six months, with paclitaxel eluting stent, and for twelve months following sirolimus eluting stent implantation.
Angiographic analysis
Coronary angiograms during procedure and at follow-up were analysed by two experienced observers after administration of intracoronary nitroglycerine using quantitative angiographic analysis system (CMS-MEDIS, Medical Imaging Systems, Leiden, The Netherlands). Lesion length, reference diameter, minimal lumen diameter (MLD), and% diameter stenosis were measured.
Definitions
Clinical presentation at the time of treatment was classified as unstable angina: new onset angina, angina at rest, and non-ST elevation myocardial infarction; Canadian Cardiovascular Society (CSS) class III/IV: severe angina needing hospitalisation; acute myocardial infarction: prolonged ischaemic chest pain associated with ST segment elevation and concomitant elevation of biochemical markers (CK AND CK-MB>3 times); and the remaining patients were classified as stable angina.
Angiographic restenosis and recurrent restenosis was defined as diameter stenosis of>50% occurring within stent and 5 mm on each side.
Baseline angiographic pattern of restenosis was defined as:
– Focal, intimal hyperplasia involving less than 10 mm of the stented segment or at the stent edge;
– Tubular, involving between 10-20 mm;
– Diffuse, involving greater than 20 mm length of the stented segment and includes proliferative and totally occlusive lesions.
Chronic total occlusion (CTO) was defined as totally occlusive ISR lesion with TIMI 0 or 1 flow of > than three months duration.
Statistical analysis
Data for continuous variables were expressed as means ± S.D and the categorical variables were expressed as frequencies. Continuous variables were compared using Student’s t test and categorical variables using chi-square test or Fischer’s exact test. Logistic regression analysis was performed on all variables to identify the predictors of recurrent ISR in ISR patients. A forward stepwise model was used with variable entry (0.05) and removal (0.10) at each step. All tests were two tailed and p<0.05 was considered significant.
Results
Baseline characteristics
Baseline characteristics and clinical presentation is shown in Table 1. Patients with SES ISR were significantly older and had a higher incidence of diabetes. The remaining baseline risk factors were similar in both groups. There were more patients with renal failure on haemodialysis in SES ISR group (p=0.001).
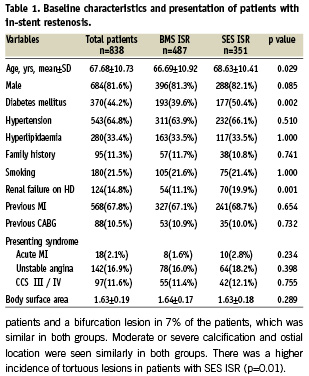
Clinical presentation was seen to be acute myocardial infarction in 2.1% of the patients with a non-significant increase in patients with SES ISR. Unstable angina and angina, CCS class III/IV, was the presenting syndrome in 16% and 11% of the patients respectively, and was similar between the BMS and SES groups. The groups with and without follow-up angiography did not differ significantly with regard to clinical, lesion, or procedural characteristics. However, the 206 patients without follow-up angiography had a higher incidence of CTO lesions (p<0.01), a higher incidence of diffuse ISR (p=.05), and a larger residual% diameter stenosis (p=0.01) than the 625 patients in whom follow-up angiography was performed.
Angiographic characteristics
As shown in Table 2, the target vessel was predominantly RCA followed by LAD and LCX, which was similar in both groups. The ISR target lesion was a chronic total occlusion in 10% of the patients and a bifurcation lesion in 7% of the patients, which was similar in both groups. Moderate or severe calcification and ostial location were seen similarly in both groups. There was a higher incidence of tortuous lesions in patients with SES ISR (p=0.01).
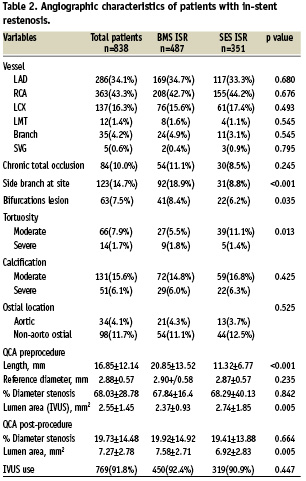
Lesion length was significantly longer in BMS ISR group (p=<0.001) with similar reference vessel diameter and baseline percent diameter stenosis. Postprocedure QCA showed similar residual stenosis in both groups with final lumen area higher in BMS ISR group (p=0.005).
Pattern of restenosis, treatment factors and outcomes
As shown in Table 3, BMS ISR presented predominantly with a non-focal pattern of restenosis and SES ISR presented with a predominantly focal pattern of restenosis. In the SES ISR patients, 47% presented with a focal pattern as compared to 19% in the BMS ISR group (p<0.0001). A diffuse pattern of ISR was seen in 36% of the BMS ISR group as compared to 16% in SES ISR group (p=0.003). The predominant treatment strategy for patients with BMS ISR was cutting balloon angioplasty, plain old balloon angioplasty (POBA), stents, and directional atherectomy (DCA) in 33%, 18%, 38%, and 5% of these patients respectively. On the other hand, the predominant treatment strategy in SES ISR was cutting balloon angioplasty, POBA, stent, and DCA in 31%, 41%, 23%, and 3% of the patients respectively. The use of POBA was significantly higher in SES ISR group (41.6% vs. 18.3%, p<0.001), and the use of stents was significantly higher in BMS ISR group (38.6% vs. 23.4%, p<0.001). A majority of the patients who were treated with stents underwent sirolimus eluting stent implantation (88.9% in BMS ISR group vs. 74% in SES ISR group) and the rest were treated with paclitaxel or bare metal stents.

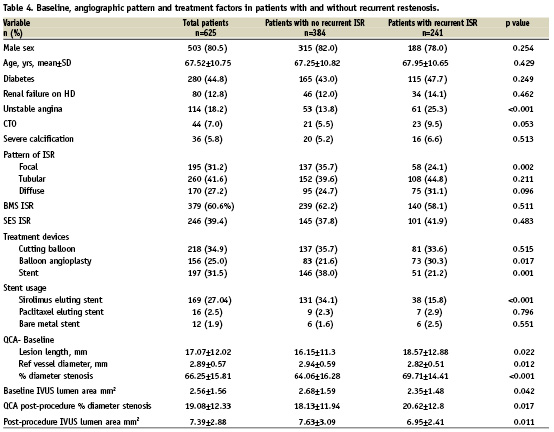
The angiographic recurrent restenosis at nine months was seen in 38.6% of the patients, and target vessel revascularisation was observed in 33.4% of the patients, with higher numerical rates in the SES ISR group as compared to BMS ISR group. There was a significantly higher incidence of sirolimus eluting stent usage in patients with no recurrent restenosis as compared to recurrent restenosis (p<0.001), with no significant impact of paclitaxel eluting or bare-metal stent (Table 4).
Predictors of angiographic recurrent restenosis
Univariate analysis as shown in Table 4, identifies unstable angina, chronic total occlusions, treatment with balloon angioplasty, lesion length, baseline% diameter stenosis, and post-procedure residual stenosis as predictors of recurrent restenosis
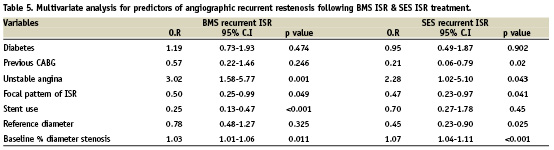
Multivariate analysis for BMS and SES recurrent ISR is shown in Table 5. We have identified unstable angina at the time of presentation, baseline% diameter stenosis, focal pattern of restenosis, and stent usage as independent predictors of BMS recurrent ISR. Unstable angina at presentation, focal pattern of ISR, reference vessel size, and baseline% diameter stenosis were shown to be independent predictors of recurrent SES ISR with no impact of stent usage.
Discussion
The main finding of our study are as following: 1) 19% of patients presented with acute coronary syndrome including acute MI and unstable angina, which was similar in both groups; 2) around half of the patients presented a focal pattern of restenosis in SES ISR group as compared to only 20% in the BMS ISR group; more patients presented with a diffuse and tubular pattern of restenosis in the BMS ISR group; 3) recurrent restenosis after conventional treatment is high (38%), being slightly higher in the SES ISR group; 4) We have identified unstable presentation, reference vessel diameter, and baseline% diameter stenosis as independent factors of recurrent restenosis, irrespective of the stent type.
Presentation of ISR
Previous studies have reported the initial presentation as acute coronary syndrome in patients with ISR ranging from 30% to 60% with bare metal and drug eluting stent in-stent restenosis10-14. The lower rates of patients presenting with acute coronary syndrome in our study could be due to differences in the definitions used, and we have reported separately on CCS angina status III/IV, which were included in some of the earlier reports as acute coronary syndromes. However, the presentation of ISR is not benign and around one third of these patients present with severe angina or ACS. Our series has shown a non-significant higher percentage of patients presenting with acute MI in SES ISR group, also observed in Steinberg’s group14.
There is evidence that neointimal proliferation occurs in association with macrophage accumulation and extensive neovascularisation providing the substrate for mural thrombus formation18. It has also been shown that proliferative tissue within the stent is rich with tissue factor associated with thrombogenic risk19. These risks could increase the chances of an unstable plaque and thrombus formation in patients with ISR resulting in unstable presentation.
Patterns of ISR
The angiographic patterns of restenosis have been studied in earlier studies. Kini et al12 has reported focal ISR in 22% patients, with 78% presenting with non-focal ISR in the Palmaz –Schatz stent ISR. Similarly, Steinberg et al14 has reported 75% of patients with BMS ISR and 50% of patients with DES ISR presenting with non-focal pattern of restenosis. Park et al13 has shown that two third of the patients with DES ISR present with a focal pattern. Similar results are reflected in our study.
The different angiographic pattern of restenosis with BMS and DES could be explained as a result of different underlying pathophysiological mechanisms of ISR. In BMS ISR the neointimal tissue proliferation is uniform and it occurs along the length of the stent15-17. In DES ISR patients, the underlying mechanism in the majority of the patients are mechanical factors resulting in unequal local drug delivery leading to a more focal pattern. This also is reflected in our observation of the increased length of the restenotic lesion seen in the BMS ISR group.
Recurrent restenosis in ISR
There is limited literature regarding the recurrent restenosis rates in this subgroup of patients with BMS and DES ISR. Kini et al12 has reported overall recurrent restenosis rate of 46%, with diffuse pattern and 14% with focal pattern following BMS ISR treatment with POBA, stenting and rotational atherectomy. Two landmark randomised trials have shown benefit of DES over brachytherapy in patients with BMS ISR4,5. Angiographic binary restenosis rate was reported as 19.8% following use of sirolimus eluting stent for BMS ISR in SISR study4. In our study, drug eluting stents were used in only 38% of the patients with BMS ISR and this could explain the higher incidence of angiographic restenosis in this group.
Treatment of DES ISR
The optimal treatment modality of DES ISR has not been well defined and there are conflicting outcomes with different treatments. Lemos et al6 evaluated the clinical and angiographic outcomes of 24 patients presenting with SES ISR following different treatments. This group reported overall recurrent restenosis rates of 42.9% and 29.3% with repeat DES implantation. Cosgrave et al7 has reported outcomes following similar DES or different DES implantation following DES ISR and reported similar rates of target vessel revascularisation (15.9% vs. 16.0%). Garg et al8 has reported a 28.8% rate of target vessel revascularisation following treatment of DES ISR with repeat DES. Recently, Steinberg et al14 has compared outcomes between BMS ISR and DES ISR following treatment with DES in 238 patients. They reported higher rates of target vessel revascularisation with patients with DES ISR group (16.0% with BMS ISR vs. 25.2% with DES ISR, p=0.08). Park et al13 reported high recurrent restenosis rates after treatment of DES ISR with DES (53.6%). Solinas et al20 has shown in a consecutive series of 182 lesions of DES ISR, the focal pattern of restenosis was observed in 69.5% of the lesions and the target vessel revascularisation rate was 8% at one year.
In our study, the angiographic recurrent restenosis and target vessel revascularisation were similar to the published literature and similar between BMS ISR and SES ISR. There was a non-significant increases in restenosis and target vessel revascularisation in the SES ISR group. This difference could be explained due to the different treatment modalities used to treat this group in our study as compared to the above mentioned studies. However, the recurrent restenosis rate remains high with DES ISR with the current available treatment.
Pathogenesis of ISR
The pathogenesis of ISR could be different in BMS and DES ISR, and targeted therapy is needed to reduce the incidence of recurrent restenosis. In BMS ISR, the restenotic tissue can be suppressed by DES implantation, but the response could vary with the initial pattern and aggressive nature of the restenosis. However, DES ISR could be due to mechanical factors like incomplete stent expansion which could well be treated with repeat balloon inflation. In some cases this could be due to the resistance to the drug and the repeat DES implantation could be detrimental with increasing incidence of restenosis due to multiple layers of stent and polymer. Further randomised studies are needed to further elucidate the mechanism and optimal treatment for the restenosis in BMS and DES ISR.
Predictors of recurrent ISR
We have also identified the presentation of unstable angina as one of the independent predictors of recurrent ISR, this phenomenon could potentially be explained by more aggressive nature of restenosis in patients presenting with unstable angina. Further studies are needed to confirm this association in large studies. Usage of the stent (DES) for the treatment of BMS ISR was shown to have a negative impact on recurrent restenosis as compared with the balloon based treatment, and is consistent with published literature4,5. However, stent usage for SES ISR was not associated with recurrent ISR. The focal pattern of ISR was also associated with less recurrent ISR.
Limitations
Our study has several limitations: firstly, the retrospective nature of the study can be subject to selection bias; secondly, in our study, the treatment of ISR was at the operators discretion and some of the differences could account for this; thirdly, incomplete angiographic follow-up could effect the outcomes, however the follow-up was similar in both groups and there was no significant difference between the baseline and angiographic characteristics of patients who failed to follow-up.
Conclusion
We have shown in our study that the presentation of ISR is not always benign with one-third of patients presenting with ACS or severe angina. The pattern of restenosis is different between SES and BMS ISR, and the recurrent restenosis rates are high and similar in both groups with current treatment. Further studies are needed for a better understanding of the pathophysiology and treatment for this group of patients.

