Abstract
Aims: To evaluate clinical outcome of patients undergoing repeated percutaneous coronary intervention (PCI) for drug-eluting stent (DES) restenosis.
Methods and results: We identified 213 patients who underwent re-PCI for DES restenosis. The study population was divided in two groups according to the treatment strategy: 94 patients were treated with at least one repeat DES implantation (DES-sandwich group); 119 patients were treated with balloon angioplasty alone (BA group). Diffuse pattern of restenosis was more frequent in DES-sandwich group (34.0% vs. 17.6%; P=0.006). During a median follow-up of 20.2 months (interquartile range 13.7 to 30.1), the incidence of cardiac death was 6.5% in the DES-sandwich and 2.5% in the BA group (P=0.18), the incidence of myocardial infarction 6.5% and 0.8% (P=0.04), and the incidence of TLR 13% and 10.9% (P=0.63), respectively. After adjustment for angiographic characteristics, DES-sandwich strategy tended to be associated with a higher rate of myocardial infarction (OR 8.2, 95%CIs[0.9-69.6]; P=0.05). By multivariate analysis, early and diffuse pattern of restenosis were found as predictors of adverse outcome at follow-up (OR 4.7, 95%CI[2.2-9.6], P<0.001; OR 2.3, 95%CI[1.1-4.8], P=0.02, respectively).
Conclusions: A default strategy of repeat DES implantation does not seem to be advantageous and could be associated with a higher rate of myocardial infarction.
Introduction
The use of coronary stents reduced the incidence of restenosis compared to the use of balloon angioplasty alone1. However, these devices led to the emergent problem of in-stent restenosis, which can be considered as an excessive response of the vessel wall to the stent-related injury2. The introduction of drug-eluting stents (DES) represented a major advance in percutaneous coronary intervention (PCI), by reducing restenosis and the need for repeat revascularisation3,4. The efficacy of DES in comparison with bare metal stents (BMS) was found in most of patient and lesion subsets (including diabetes, bifurcation lesions, chronic total occlusions, small vessels, long lesions) leading to a widespread use of DES. However, DES restenosis, even if not frequent, is not abolished and the optimal percutaneous management of this condition is, currently, not well established. In this study, we sought to evaluate the long-term clinical outcome of patients undergoing repeated PCI for DES restenosis, also investigating the influence of restenosis pattern and treatment strategy.
Methods
From dedicated databases of all consecutive DES implantation procedures of two high-volume Italian catheterisation laboratories, the Ferrarotto University Hospital, Catania, and the S.Orsola-Malpighi University Hospital, Bologna, we retrospectively identified 213 patients who underwent repeated PCI for DES restenosis between May 2002 and May 2007. In-stent restenosis was defined, by visual assessment, as a luminal stenosis > 50% within the stent or within 5 mm of its edges. Cases of stent thrombosis were previously excluded, as well as cases of DES implantation for BMS in-stent restenosis. We analysed 252 DES restenotic lesions categorised, according to the Mehran classification, as focal (type I) and diffuse (type II, III and IV)5. The study population was divided in two groups according to the treatment strategy: 94 patients (44.1%) were treated with at least one repeat DES implantation (DES-sandwich group); 119 patients (55.9%) were treated with balloon angioplasty alone (BA group). The choice of treatment strategy was at the operators’ discretion. IVUS usage was 13.8% in DES-sandwich patients and 11.7% in BA patients (P=0.8). All patients were in lifelong treatment with aspirin 100 mg daily. A loading dose of 300-600 mg of clopidogrel was administered to the DES-sandwich group patients if they were not already on a maintenance dose of clopidogrel. A double antiplatelet therapy (aspirin 100 mg daily and clopidogrel 75 mg daily or ticlopidine 250 mg twice a day) was prescribed for at least one month to patients of the BA group and for at least six months to patients of the DES-sandwich group. No patient discontinued double antiplatelet therapy before the prescribed time. The study patients were clinically followed for a median of 20.2 months (interquartile range 13.7 to 30.1); DES-sandwich patients median follow-up was 20.7 months (interquartile range 13.7 to 29.3) and BA pts median follow-up was 18.7 months (interquartile range 13.7 to 32.2). On a per patient basis, we analysed the incidence of cardiac death, myocardial infarction and target lesion revascularisation (TLR) during hospitalisation and at follow-up in the overall population and in each group. We also reported the rate of stent thrombosis, according to the Academic Research Consortium (ARC) definitions6, in the overall population and in each subgroup.
Statistical analysis
Continuous variables are reported as means±SD and compared using independent sample Student t test. Discrete variables are reported as frequencies (percentage) and compared using Chi-square or Fisher exact tests, as appropriate. On a patient-based setting, a multivariate logistic regression analysis was performed to identify the independent predictors of major adverse cardiovascular events (MACE) at follow-up. A binary logistic regression model was used to determinate the unadjusted and adjusted association between repeat DES implantation and worse clinical outcome. A p value <0.05 was considered statistically significant. All statistical tests were performed using SPSS 13.0 for Windows.
Results
No significant differences in baseline demographic and clinical characteristics were found between the DES-sandwich group and the BA group (Table 1).
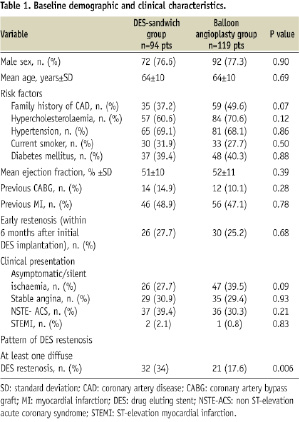
In both groups there was a high prevalence of diabetics (39.4% and 40.3% in DES-sandwich and in BA group, respectively; P=0.88), underscoring theintrinsic high risk profile of thispatients subset. Among the overall population, 64.3% of the patients (58.5% in DES-sandwich group and 68.9% in BA group; P=0.15) presented with a stable clinical status (asymptomatic, silent ischaemia or stable angina). Asymptomatic patients represented 5.6% of the overall population (5.3% in DES-sandwich group and 5.0% in BA group; P=0.82). In 65.7% of patients presenting with acute coronary syndrome (ACS), without any significant differences between the two groups, DES restenosis was indentified as the culprit lesion. Because of the selection criteria, none of the BA group patients received repeat DES implantation; conversely, 4.2% of the DES-sandwich group patients had a DES-restenosis treated with balloon angioplasty alone (besides the DES-sandwich lesion). We analysed 252 DES restenotic lesions: 118 lesions in the DES-sandwich group and 134 lesions in the BA group. Among all of the study lesions, the initial DES implanted was a Cypher™ (Cordis, Johnson & Johnson, Warren, NJ, USA) sirolimus-eluting stent (SES) in 143 lesions (56.7%), a Taxus™ (Boston Scientific, Natick, MA, USA) paclitaxel-eluting stent (PES) in 98 lesions (38.9%) and an Endeavor™ (Medtronic, Minneapolis, MN, USA) zotarolimus-eluting stent (ZES) in 11 lesions (4.4%). The pattern of restenosis was focal in 197 lesions (78.2%) and diffuse in 55 lesions (21.8%). We did not find any significant association between DES type and pattern of restenosis. The DES-sandwich group patients had a lower prevalence of small treated vessel (≤ 2.5 mm diameter) (29.7% vs. 47%, P=0.005) and a higher prevalence of LAD treatment (58.5% vs. 43.3%, P=0.016), compared with BA group patients. Moreover, the DES-sandwich group patients had a higher prevalence of diffuse and focal-edge restenosis pattern in comparison with the BA group patients (28.8% vs. 15.7%, P=0.01, and 38.9% vs. 11.9%, P<0.0001; respectively). Angiographic and procedural characteristics of the patients are presented in Table 2.

Among the overall population, the incidence of in-hospital death was 0.9%. It was related to two patients, the first one enrolled for a PES restenosis treated with SES implantation (hetero-DES sandwich), who developed fatal acute stent thrombosis, and the second one enrolled for a SES restenosis treated with SES implantation (homo-DES sandwich) who died for a non-cardiac cause (suspect bowel ischaemia and acute peritonitis). No significant difference in the in-hospital event rate was found between the DES-sandwich group and the BA group (Table 3).
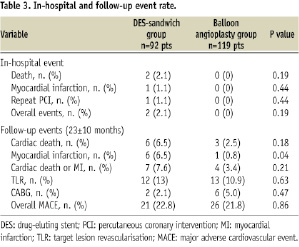
During follow-up, in the overall population the incidence of cardiac death, myocardial infarction and TLR were 4.3%, 3.3% and 11.8%, respectively; the overall MACE-rate (composite of cardiac death, MI or TLR) was 22.3%. Comparing subgroups, we found a higher incidence of myocardial infarction in the DES-sandwich group in comparison with the BA group (6.5% vs. 0.8%, P=0.04) (Table 3). Kaplan-Meier curves of cardiac death, myocardial infarction, TLR and MACE-free survival are showed in Figure 1.
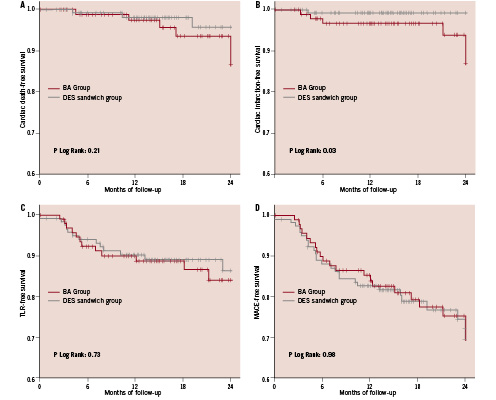
Figure 1. Kaplan-Meier curves of cardiac death-free survival (A), Myocardial infarction-free survival (B), TLR-free survival (C) and MACE-free survival (D) in the pooled population according to the treatment strategy.
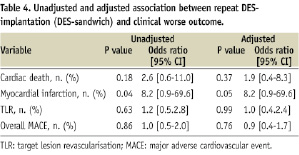
After adjustment for baseline angiographic characteristics: small vessel (reference vessel diameter ≤2.5 mm), LAD treatment, diffuse pattern of restenosis, DES-sandwich strategy tended to be associated with a higher incidence of myocardial infarction (OR 8.2, 95% CIs [0.9-69.6]; P=0.05) (Table 4).
During hospitalisation and follow-up, stent thrombosis occurred in eight patients (details for each group in Table 5).
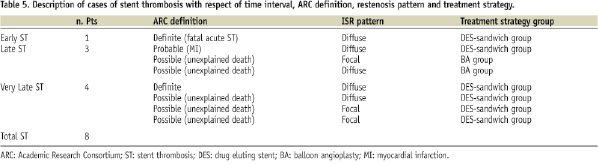
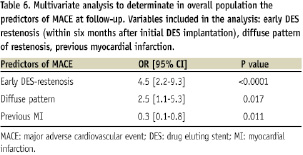
The overall incidence of stent thrombosis (definite, probable or possible) was 6.4% and 1.7% (P=0.14) in DES-sandwich and BA group, respectively. This difference was especially due to a higher incidence of very late stent thrombosis (4.3% vs. 0% in DES-sandwich and in BA group, respectively; P=0.03). On the other hand, when adopting a more restrictive definition of stent thrombosis, excluding the possible ones, a trend toward a higher rate of stent thrombosis among patients with repeat DES implantation was also seen (3.2% vs. 0% in DES-sandwich and in BA group, respectively; P=0.08). Among all of the study population, univariate analysis showed that patients suffering a MACE at follow-up had more frequently an early (51.1% vs. 18.9%; P<0.0001) and diffuse DES restenosis (38.3% vs. 20.7%; P=0.014) compared to those without events; whereas event-free patients had more frequently a previous MI (52.4% vs. 31.9%; P=0.013). A multivariate analysis, including these three variables, confirmed the presence of a significant association between early and diffuse restenosis, and adverse outcome at follow-up (OR 4.5, 95% CI [2.2-9.3], P<0.0001 and OR 2.5; 95% CI [1.1-5.3], P=0.017, respectively) (Table 6).
Angiographic follow-up was performed in 31.9% of the DES-sandwich patients and 30.2% of the BA patients at 10.7±6.7 months, if required by clinical status or if scheduled at the time of index procedure. Recurrence of restenosis was 15.2% in the DES-sandwich patients and 16.4% in the BA patients (P=0.93).
Discussion
The main findings of our study are the following: (a) DES restenosis has a predominantly stable clinical presentation and a focal pattern, (b) percutaneous treatment of DES restenosis is a relatively safe and effective procedure considering the high cardiovascular risk of the study population, (c) repeat DES implantation does not improve the clinical outcome of patients in comparison with balloon angioplasty alone and could affect the safety profile of the procedure, (d) lesion-related factors (time, pattern) influence the clinical outcome of the patients.
Compared to bare metal stent restenosis, DES restenosis is not a frequent phenomenon but its optimal percutaneous treatment has not been established, yet. Dealing with DES restenosis, two factors need to be considered: the pattern of restenosis and the treatment strategy. Similar to BMS, the pattern of DES restenosis can be divided in focal and diffuse. Several experiences showed that the pattern of DES restenosis is predominantly focal (in-stent or at the edges)7,8 and that this pattern, when re-PCI is performed, is associated with better outcome compared to the diffuse one9.
However, the pattern of DES restenosis is not the only factor which influences the choice of treatment strategy and the clinical outcome. In fact, DES restenosis has different biological mechanisms from BMS restenosis10 and a more heterogeneous histopathological composition: whereas BMS restenosis is predominantly composed by smooth muscle cells, the composition of DES restenosis varies from a predominantly smooth muscle cell composition to a T-lymphocyte and macrophages infiltrate or an organised fibrin. The different pathophysiology of DES restenosis, in comparison with that of BMS restenosis, appears to be confirmed by IVUS pattern which frequently shows an echolucent intimal hyperplasia, named “black hole”, typically revealed after brachytherapy, but not after BMS implantation11. The black hole represents an altered response of vessel wall to the stent-related injury and is characterised by a hypocellular matrix with areas of proteoglycans, in absence of elastin or collagen12. Whether or not the black hole phenomenon is associated with the recurrence of restenosis has not been established.
Therefore, although the strategy of DES implantation for the treatment of BMS restenosis has been shown to be promising13, these results could not be extrapolated for the treatment of DES restenosis. Mishkel et al14, in a recent study involving 92 patients undergoing revascularisation for DES failure, showed that the implantation of a different type of DES (hetero-stent sandwich) tended to be associated with lower MACE rates and need for reintervention at 12 months follow-up in comparison with homo-stent implantation or other treatment, without any differences in myocardial infarction and death rates. Cosgrave et al15 compared the strategies of same and different DES implantation for the treatment of DES restenosis in 174 patients and 201 lesions. A multivariate analysis showed the lack of association between the treatment strategy and the target lesion revascularisation (OR 0.7; 95% CI [0.2-1.6]; P=0.42), whereas a diffuse pattern of restenosis was found as a predictor of TLR (OR 2.9; 95% CI [1.2-7.2]; P=0.015) and restenosis (OR 3.6; 95% CI [1.5-8.8]; P=0.004). This study also showed no significant difference in the safety profile between same DES and different DES implantation approaches. Similar results were reported by Garg et al in a study involving 116 patients treated for DES restenosis: no difference was found in the safety and efficacy profile between same and different DES implantation at one year follow-up16.
In our experience, the strategy of repeat DES implantation has shown no apparent advantage as compared to balloon angioplasty alone in reducing the need for reintervention at long-term follow-up but, even after adjustment for the prevalence of diffuse pattern of restenosis and other angiographic characteristics, tended to increase the risk of myocardial infarction. Importantly, the rate of stent thrombosis was higher among patients treated with repeat DES implantation, because of an higher rate of very late stent thrombosis. Even excluding the “possible” stent thrombosis, we found a trend toward a higher risk of stent thrombosis among DES-sandwich subgroup of patients. Although no definitive conclusion can be drawn from our data, this remains an important observation that deserves further investigation. Balloon angioplasty alone, if the immediate angiographic result is satisfying, could be safer and equally effective compared to repeat DES implantation for the treatment of DES restenosis. The ongoing CRISTAL study17, a prospective, multicentre, randomised trial comparing sirolimus-eluting stent and balloon re-angioplasty for the treatment of DES restenosis, and GISE-CROSS study18, a prospective, multicentre, randomised trial evaluating a crossover repeat DES implantation strategy, will probably give us useful data to understand the optimal treatment of DES restenosis.
Conclusion
In our experience, percutaneous treatment of DES restenosis is associated with a relatively low incidence of adverse events at long-term follow-up. After adjustment for baseline angiographic characteristics, no significant differences were found in efficacy profile between repeat DES implantation and balloon angioplasty alone, although the safety profile of repeat DES implantation should be better clarified. Early DES restenosis and diffuse pattern of restenosis were found as predictors of adverse outcome at follow-up.
Study limitations
The main limitations of our study are the absence of randomisation to the treatment strategy and the retrospective nature. Other limitations are the low usage and the absence of IVUS data, the relatively small sample size and the relatively low rate of angiographic follow-up, which could under power the study to detect very long-term differences between the groups.

