The impressive strides made by interventional cardiology in the last two decades have been able to improve the quality of life and the prognosis of patients with coronary artery disease. Novel drug-eluting stents (DES) and refined adjunct pharmacological therapies have provided unprecedented results in terms of the safety and efficacy of coronary revascularisation1. Notwithstanding these remarkable advances, stent failure still overshadows the results of percutaneous coronary interventions (PCI)2. Angiographic restenosis is still seen in routine clinical practice but tends to be considered a technical nuisance that, when clinically indicated, can be readily tackled by repeat interventions1,2. These reinterventions are simple procedures from a technical standpoint but suffer from higher recurrence rates compared with PCI in de novo lesions1,2. In addition, the incidence of in-stent restenosis (ISR) in different scenarios, the burden generated by the ISR “activity” worldwide and, more importantly, the long-term fate of these patients are not well established2. Accordingly, new epidemiological studies, observational registries, and randomised clinical trials are warranted to shed new light on this unmet clinical need1,2. Likewise, administrative databases, enabling analyses from huge patient populations, provide alternative insights on the prevalence and results of ISR treatment.
Present study
In this issue of EuroIntervention, Tamez et al3 report data from the National Cardiovascular Data Registry (NCDR) CathPCI Registry, comparing results of patients treated for ISR and de novo lesions.
Of ~3,000,000 patients treated with PCI between 2009 and 2014, one half were aged >65 years and in 44% of them long-term clinical outcomes could be obtained by linking to Medicare and Medicaid services claims databases. The final study cohort consisted of 653,304 patients, of whom 66,718 (10.2%) required the treatment of ISR. After a median follow-up of 2.3 years, major adverse events (54.6 vs 45%), all-cause mortality (27.8 vs 25.5%), myocardial infarction (19 vs 12.3%), repeat revascularisation (31.9 vs 18.6%), target vessel revascularisation (22.4 vs 8%) and stroke (8.8 vs 8.3%) were more frequent in the ISR group. In addition, after careful adjustments, patients with ISR showed a significantly higher rate of events, including any revascularisation, target vessel revascularisation and mortality.
This study provides novel insights on the burden of ISR activity in US facilities and on the clinical fate of these patients. Importantly, results from this huge patient population complement and challenge current knowledge. Overall, the study suggests that 1) “ISR activity” remains very high (1 in every 10 PCI procedures), and 2) the prognosis of these patients is markedly worse than that seen in patients treated for de novo lesions. Some methodological issues, however, deserve consideration.
First, administrative databases offer the possibility of assessing data from impressively large patient samples and, therefore, are particularly attractive to address problems with a relatively low prevalence. Alternatively, these studies systematically suffer from codification caveats and lack the required clinical granularity to ensure a reliable adjustment for variables with well-established implications4. For instance, the elapsed time between initial PCI and the repeat PCI for ISR was not available whereas, at follow-up, rates of target lesion revascularisation could not be ascertained as only data on target vessel revascularisation were captured. Nevertheless, the authors should be commended for their efforts to perform different adjustments (multivariable and propensity score) and also several sensitivity analyses, to mitigate these potential problems. Reassuringly, the results of all these analyses were largely consistent. However, when the baseline characteristics of the population under comparison are so different, it is likely that some unknown confounders (by definition impossible to adjust for) will also play a major role in the results4. In addition, the adjudication of events at follow-up may be questioned, especially when linking different administrative data sets is required.
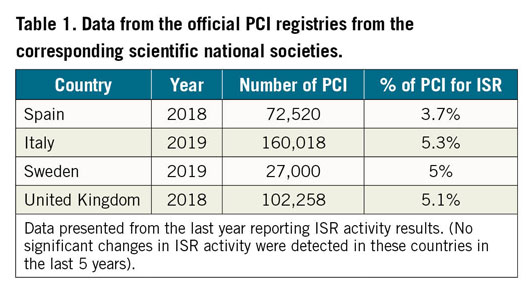
Second, ISR activity accounts for 10% of PCI (i.e., 1 in every 10), which is very high and, in fact, difficult to understand from a European perspective1,2. Data from several activity registries from national scientific societies suggest that the ISR activity in Europe is consistently lower: ~5% (Table 1). This figure (i.e., 1 in every 20 PCI) is better aligned with clinical experience. It may be argued that these official nationwide activity registries also suffer from methodological issues, including audit and codification problems but, reassuringly, despite using distinct approaches, yielded consistent results. Whether the oculostenotic reflex could play a more relevant role in US sites, whereas assessment of ischaemia (non-invasively, intracoronary physiology) is more frequently required in Europe before proceeding with ISR treatment, remains speculative1,2. Actually, most patients included in the study of Tamez et al4 had a clinical indication for the repeat PCI procedure. Therefore, it remains possible that codification, data management or statistical issues could help to explain this major gap (5% vs 10%) in ISR activity across the Atlantic.
Third, the study confirms the large body of evidence demonstrating that PCI for ISR is associated with poorer results than treatment of de novo lesions1,2. A decade ago, Cassese et al5 already suggested that the appearance of ISR after stent implantation was associated with an increase in mortality. In a study including ~10,000 patients (~15,000 lesions) undergoing systematic late angiographic surveillance, ISR was significantly associated with four-year all-cause mortality. This association persisted after adjusting for potential confounders (adjusted HR 1.23)5. Likewise, a study with pooled patient-level data from 21 randomised clinical trials stratified 32,524 patients according to whether or not repeat target lesion revascularisation was performed6; after a median follow-up of 37 months, 2,330 patients (7.2%) underwent non-emergent target lesion revascularisation. After adjustment, target lesion revascularisation emerged as an independent predictor of mortality (adjusted HR 1.23)6.
The present study also confirms that treatment of DES-ISR is associated with poorer outcomes than treatment of bare metal stent (BMS)-ISR. The DAEDALUS study7, a large patient-level meta-analysis including ~2,000 patients from 10 randomised clinical trials, demonstrated that treatment of DES-ISR is particularly challenging. Both DES and drug-coated balloons (DCB) provided equivalent results in patients with BMS-ISR. However, in the more challenging subset of patients with DES-ISR, DES proved to be superior to DCB regarding clinically driven target lesion revascularisation7.
Finally, a disturbing finding of this study is the overall high rate of events during a relatively short follow-up. These event rates are significantly higher than those reported in randomised clinical trials comparing different therapeutic modalities in patients with ISR8,9,10. In the current study, only elderly patients (with higher comorbidity) were included and some presented unusual findings for ISR (7.1% ST-segment elevation, 17% Thrombolysis In Myocardial Infarction [TIMI] 0-1 flow) and were treated with devices (27% conventional balloons or BMS) different from guideline recommendations1. Likewise, information on the use of intracoronary imaging, as suggested by current guidelines1, was not provided. Moreover, in randomised studies the clinical indication for repeat revascularisation at follow-up is clearly defined, whereas it may be elusive in routine clinical practice. The benign clinical profile of the selected patient populations included in randomised trails may also explain the differences. Nevertheless, the overall high event rate found in this study suggests that paying major attention to late clinical outcomes remains of paramount importance. These findings represent a red flag that reminds us that, in addition to the efforts made to optimise the results of the repeat interventions, a holistic management strategy, including aggressive secondary prevention measures, remains mandatory for these challenging patients1,2.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.