Abstract
Aims: The optimal drug-eluting stent (DES) in ST-elevation myocardial infarction (STEMI) patients remains unclear. We sought to compare the long-term performance of everolimus-eluting stents (EES) and Endeavor zotarolimus-eluting stents (E-ZES) in STEMI.
Methods and results: The current analysis of a prospective registry included consecutive patients treated with EES or E-ZES for STEMI. Adjustment for measured confounders was done using Cox regression. In total, 931 patients met the inclusion criteria (412 EES and 519 E-ZES). Baseline characteristics were balanced, apart from a lower rate of renal insufficiency in EES. Median follow-up duration was 2.4 years (IQR 1.6-3.1). Mortality outcomes were similar. Up to three-year follow-up, the composite endpoint of cardiac death, target vessel-related myocardial infarction and target lesion revascularisation (TLR) was lower in EES; 9.7% vs. 13.7% in E-ZES (HR 0.64, 95% CI: 0.42-0.99), primarily driven by reduced TLR rates; 3.4% in EES vs. 7.3% in E-ZES (HR 0.46, 95% CI: 0.23-0.92). Definite stent thrombosis rates were low and similar between groups (1.1% in EES vs. 1.9% in E-ZES, p=0.190).
Conclusions: Use of EES led to lower rates of the composite endpoint, driven by reduced TLR. This suggests that EES are more efficacious than Endeavor ZES in STEMI. Definite ST rates were low, and the strategy of second-generation DES implantation and the administration of upfront GP IIb/IIIa inhibitors appear to be safe in STEMI.
Introduction
Second-generation everolimus-eluting stents (EES) have shown superior results in stable coronary lesions and all-comer patients compared to both bare metal and first-generation paclitaxel-eluting stents (PES)1-5. Comparison of Endeavor zotarolimus-eluting stents (E-ZES) with bare metal and PES showed improved outcome after E-ZES implantation in stable coronary lesions6-9. The results of these trials have led to the widespread use of second-generation stents in current clinical practice. The use of drug-eluting stents (DES) in the setting of ST-elevation myocardial infarction (STEMI) is, however, still under investigation. Trials comparing DES in STEMI have mainly focused on the comparison of bare metal and first-generation DES10. Therefore, limited data exist with regard to the performance of different types of second-generation DES in patients presenting with STEMI. The current study sought to investigate the long-term performance of the second-generation EES and Endeavor ZES in an unselected STEMI population.
Methods
DESIGN AND PATIENTS
The prospective MISSION! registry included all patients treated with primary percutaneous coronary intervention (PCI) for STEMI in a high-volume tertiary centre11. For the current retrospective analysis, consecutive patients treated between the 1st of January 2007 and the 1st of October 2010 were eligible for inclusion. Patient selection was done according to procedural stent type. All patients treated with either EES (Promus®; Boston Scientific, Natick, MA, USA) or E-ZES (Endeavor®; Medtronic Vascular, Santa Rosa, CA, USA) were included in the current analysis. E-ZES were implanted in the Leiden University Medical Center from early 2006 and EES were implanted from the beginning of 2007. Therefore, both stent types were used during the entire inclusion period. Stent choice was left to the discretion of the operator. Patients treated with both stents simultaneously as well as patients treated with other types of drug-eluting or bare metal stents (BMS) were excluded. Patients were treated and followed according to the institutional STEMI protocol (MISSION!), implemented at Leiden University Medical Center from February 200411. Patients follow a standardised pre-hospital, in-hospital and outpatient clinical framework for decision making and treatment. The pre-hospital protocol included field triage by 12-lead electrocardiogram (ECG) faxed to the operator on call and in-ambulance treatment with a loading dose of clopidogrel, aspirin, heparin, and intravenous glycoprotein IIb/IIIa inhibitors. Upon arrival at the hospital, patients were transferred directly to the catheterisation laboratory or coronary care unit to wait for the arrival of the intervention team. Procedures were performed according to current clinical guidelines. If tolerated, patients received beta-blockers, ACE-inhibitors and statins within 24 hours. Additionally, patients were prescribed dual antiplatelet therapy, consisting of aspirin 100 mg daily for life and clopidogrel 75 mg daily for 12 months. Patients with an indication for Coumadin were prescribed warfarin instead of aspirin.
Following hospital discharge, patients were intensively monitored and managed in the outpatient clinic for one year, after which they were referred back to the general practitioner or referred to a regular, generally regional, cardiological outpatient clinic. Vital status was gathered through municipal records. Follow-up data were adjudicated and prospectively collected in the electronic patient file (EPD Vision version 8.7.0.1.) by independent clinicians; data from patients participating in the out-patient programme were gathered by out-patient chart review, and follow-up data of patients not participating in the out-patient programme were gathered by telephone interviews.
Definitions
STEMI was defined as symptoms of angina lasting longer than 30 minutes along with electrocardiogram demonstrating STEMI (ST-segment elevation ≥0.2 mV in ≥2 contiguous leads in V1 through V3 or ≥0.1 mV in other leads or presumed new left bundle branch block). Recurrent myocardial infarction was defined as symptoms of angina lasting longer than 30 minutes in addition to troponin levels above the ULN (upper limit of normal) or a 25% re-rise of troponin levels in case of reinfarction after the index procedure. Periprocedural infarction was defined as an elevation of troponins three times above ULN for PCI and five times above ULN for coronary artery bypass grafting (CABG). Target vessel revascularisation (TVR) was defined as any repeat percutaneous intervention or surgical bypass of any segment of the target vessel. Target lesion revascularisation (TLR) was defined as any repeat PCI or bypass surgery of the target lesion including the 5 mm proximal or distal region of the stented area. Stent thrombosis (ST) was defined according to Academic Research Consortium (ARC) definitions12. Furthermore, ARC-suggested composite endpoints were defined. The device-oriented endpoint was a composite of cardiac death, MI not clearly related to a non-target vessel and target lesion revascularisation (TLR). The patient-oriented endpoint consisted of all-cause mortality, any myocardial infarction and any repeat revascularisation procedure.
Statistical analyses
Continuous variables are presented as means with standard deviations (SD) and were compared using Student’s t-test. Categorical variables are expressed as counts and percentages and were compared by means of Pearson’s χ2 test. Time to endpoint was analysed using Kaplan-Meier plots and the log-rank test was applied to compare the cumulative incidences of the endpoints between groups. All statistical tests were two-tailed and a p-value ≤0.05 was considered statistically significant. Crude and adjusted hazard ratios (HR) with 95% confidence intervals (CI) were calculated using Cox proportional hazard regression models. Univariable predictors of outcome were entered into multivariable models using a cut-off p-value <0.10. In case of limited number of events, selection of variables was based on effect size.
Results
During the inclusion period a total of 1,199 patients were treated with primary PCI. Of these patients 931 met the inclusion criteria of this study: 412 patients received at least one EES and 519 patients at least one E-ZES (Figure 1). Median follow-up duration was 2.3 years (IQR 1.6-3.0) for EES patients and 2.4 years (IQR 1.6-3.2) for E-ZES patients.
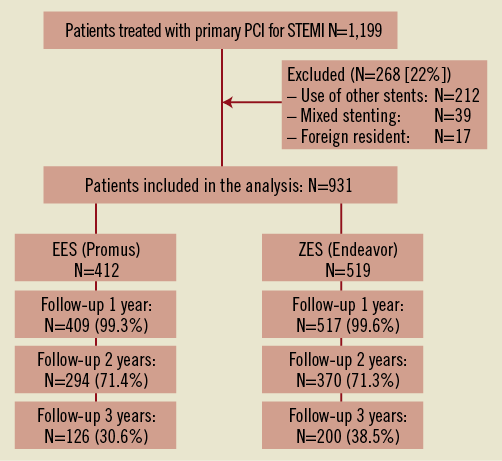
Figure 1. Inclusion and follow-up chart.
Baseline characteristics (Table 1) showed that patients treated with E-ZES more frequently had a history of renal insufficiency. Furthermore, patients treated with EES were more frequently discharged with beta-blockers compared to E-ZES patients (Table 2). Other baseline and procedural characteristics were balanced (Table 2).
Table 3 presents clinical outcomes up to three years. During the first year, the patient-oriented endpoint was balanced between the groups. The device-oriented composite endpoint occurred in 4.7% of EES patients and in 8.7% of E-ZES patients (HR 0.56 in multivariable analysis, 95% CI: 0.32-0.97). This was driven by both lower rates of target vessel-related MI (HR 0.27, 95% CI: 0.08-0.93) and TLR (HR 0.21, 95% CI: 0.06-0.72). In addition, the individual rate of TVR was lower in patients treated with EES compared to E-ZES patients (HR 0.53, 95% CI: 0.29-0.98) and definite ST showed a trend towards a lower rate in EES patients (HR 0.16, 95% CI: 0.02-1.28).
The rate of the device-oriented endpoint remained significantly lower up to three-year follow-up (Figure 2A), with 9.7% of EES patients versus 13.7% of E-ZES patients reaching the endpoint (HR 0.64, 95% CI: 0.42-0.99). This was mainly driven by TLR (Figure 2B), which showed rates of 3.4% in EES patients versus 7.3% in E-ZES patients (HR 0.46, 95% CI: 0.23-0.92). The patient-oriented composite endpoint (Figure 2C) and cardiac mortality (Figure 2D) did not differ during long-term follow-up. Moreover, definite ST (Figure 3) showed comparable rates. ST occurred subacutely (24 hours to 30 days after PCI) in six cases, once in EES and five times in E-ZES. Late ST (30 days to one year after PCI) occurred in two E-ZES patients, and very late ST (later than one year) occurred in two EES patients and one E-ZES patient. Dual antiplatelet therapy compliance was similar between the groups, showing a 99% rate for aspirin/Coumadin adherence and 98% for clopidogrel adherence at one year. Of the patients suffering from late ST, two were using aspirin and one was using both aspirin and clopidogrel at the time of ST.
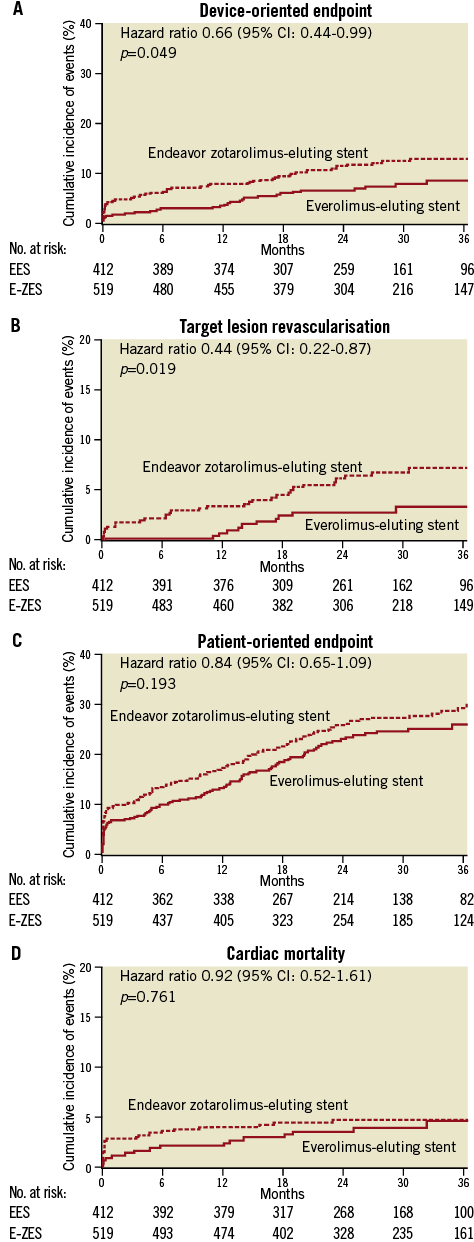
Figure 2. A) Device-oriented endpoint (composite of cardiac death, target vessel-related MI and target lesion revascularisation) up to three-year follow-up. B) Target lesion revascularisation up to three-year follow-up. C) Patient-oriented endpoint (composite of all-cause mortality, any myocardial infarction and any revascularisation procedure) up to three-year follow-up. D) Cardiac mortality up to three-year follow-up. Abbreviations can be found in legend for Figure 1.
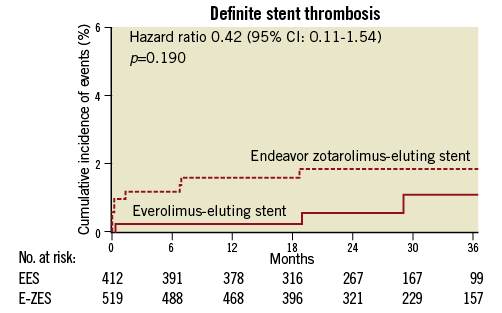
Figure 3. Definite stent thrombosis.
Discussion
The major finding of this observational investigation, comparing long-term outcomes of EES and Endeavor ZES in an unselected STEMI population up to three-year follow-up, was that EES implantation was independently associated with lower rates of the device-related endpoint of cardiac mortality, target vessel-related MI and TLR compared to E-ZES. This was driven by lower rates of TLR in EES patients. Furthermore, definite ST rates were low and the strategy of second-generation DES implantation and the administration of upfront GP IIb/IIIa inhibitors appear to be safe in STEMI.
Myocardial infarction has long been considered an off-label indication for DES. While first-generation DES have been shown to reduce revascularisation rates in STEMI patients compared to BMS, the benefit is offset by a higher risk of very late ST13,14. Stenting in acute coronary syndromes was found to be an independent predictor of ST after DES implantation15. Delayed endothelialisation, thrombotic burden, stent underexpansion and stent malapposition have been identified as mechanisms for the higher rate of ST after DES implantation in patients with acute coronary syndromes16-18. Moreover, evaluation of patient adherence to dual antiplatelet therapy is complicated by the acute setting of myocardial infarction. Second-generation stents have been developed to reduce the incidence of ST while attempting to improve the efficacy of DES. In this study, we compared the second-generation EES and E-ZES. The EES is a thin strut (81 µm), cobalt-chromium, Multi-Link™ stent (Abbott Vascular, Redwood City, CA, USA) with a biocompatible polymer eluting everolimus, a sirolimus analogue. Eighty percent of the everolimus is eluted in the first 28 days. EES showed faster endothelialisation compared to first-generation stents in preclinical studies19. The Endeavor ZES is based on a cobalt-chromium Driver™ platform (Medtronic), consisting of 91 µm struts covered by a biomimetic phosphorylcholine polymer releasing the sirolimus analogue zotarolimus. The Endeavor stent releases 95% of its inhibitory drug within 28 days, which is the fastest elution of all stents currently in use.
In the current study, patients treated with EES showed lower rates of the composite endpoint of cardiac mortality, target vessel-related MI and TLR compared to E-ZES patients up to three-year follow-up. The difference was driven by lower rates of TLR in EES patients. This observation is in line with previous studies demonstrating an association of EES with lower late luminal loss (average 0.14 mm, compared to 0.6 mm in E-ZES) which is a strong surrogate endpoint for TLR20,21. This indicates that EES have a higher potential for suppressing neointimal growth. It underlines that more aggressive inhibition of intimal hyperplasia is not directly related to a higher risk of ST but that other factors, like stent design, polymer properties and release characteristics of the drug, also play a role.
Recently, Hannan et al performed a propensity score matched comparison of EES and E-ZES and found a reduced rate of repeat revascularisations for EES patients during two-year follow-up22, reflecting the current results. Ten percent of patients included in their registry were treated for MI within 24 hours; however, exact diagnosis was not mentioned. Trials or registries focusing on the use of EES or E-ZES in STEMI patients specifically are limited. The Evaluation of XIENCE V stent in Acute Myocardial Infarction (EXAMINATION) trial randomised MI patients to EES or BMS and reported lower rates of TVR, TLR and definite ST in the EES group after one year23. A comparison of EES and SES was made in the XIENCE V Stent vs. Cypher Stent in Primary PCI for Acute Myocardial Infarction (XAMI) trial, which included 96% STEMI patients, and suggested superior MACE rates in EES compared to SES up to one-year follow-up, although the trial was not powered for this24. Additionally, Kedhi et al25, comparing EES with PES in the indication of STEMI in a post hoc analysis, observed superior outcomes of EES up to two years of follow-up. Rates of mortality, MI and revascularisations were relatively low compared to the current study. This is most likely due to a higher risk population in the current analysis, since no patients were excluded on account of clinical or angiographic characteristics. In contrast, the HORIZONS-AMI trial26 reported markedly higher rates of definite ST after PES implantation (4.2% at three years) despite inclusion of lower risk patients, indicating that there might be improved safety with the use of second-generation stents in STEMI.
The ST rates found in the E-ZES group of this study were somewhere in between the results of PES and EES. E-ZES have previously been compared with SES in the setting of STEMI by Kim et al27. Up to one-year follow-up, E-ZES showed a similar incidence of ST (1.0% vs. 1.8%). Additional studies found no differences in outcome among PES, SES and E-ZES in STEMI patients up to 18 months of follow-up28-31. In these studies, the E-ZES groups showed variable ST rates ranging from zero to 2.9 percent. Longer-term data on the performance of E-ZES in STEMI are lacking.
Recent results from the RESOLUTE all-comers trial showed non-inferiority of the Resolute ZES (R-ZES, characterised by a new biocompatible polymer with a more gradual release of zotarolimus; Medtronic) compared to EES. The two-year definite ST rate was 2.0% in the R-ZES compared to 1.0% in EES32. In contrast, the recent TWENTE trial found a trend towards a reduction in definite/probable ST after one year in patients treated with R-ZES compared to EES33. These results suggest that improved safety and efficacy outcomes of the R-ZES compared to E-ZES are possibly due to improvements in polymer and elution pattern. However, this remains speculation without definitive randomised clinical data. In this study a trend towards lower one-year ST rates in EES was seen, due to differences in the incidence of ST in the early period after stent implantation. From previous studies it is known that acute ST is related to procedure-related factors like dissection, undersizing of stent, TIMI flow less than 3 after procedure and lack of glycoprotein IIb/IIIa inhibitors34. However, no acute ST were observed in our population. Subacute ST, which occurred in six instances, is related to a variety of factors, among which are diabetes mellitus, left ventricular function under 40%, complex lesions and acuteness of PCI35. The role of procedure-related factors is smaller in subacute ST, suggesting that the higher early rate of ST in E-ZES might be due to differences in stent design. However, long-term rates of ST were similar in our population, supporting adequate safety of both second-generation stents during long-term follow-up.
Study limitations
The current observational cohort included the entire range of STEMI patients encountered in daily practice. Optimal care consisted of low diagnosis times and low door-to-balloon times, upfront glycoprotein IIb/IIIa inhibitors and an intensive outpatient management programme. There are, however, several limitations to the current study design. Because the Endeavor ZES is no longer clinically in use, the Resolute ZES might have been better for comparison with EES. Furthermore, the results must be interpreted with caution due to the non-randomised, observational nature of the study. Although a wide range of baseline and angiographic characteristics was balanced between the groups, bias could have occurred during the selection of the patients. Multivariable Cox proportional hazards analyses were performed to correct for confounders but unmeasured characteristics may have influenced comparison of the groups. Propensity score matching might have provided more adequate correction for confounding but was not possible due to limitations in population size. The study was underpowered to detect differences in rare events like ST. Additionally, the adjudication of repeat MI events was not performed according to the latest trial protocols, and this may have led to underestimation of MI events, though there is no reason to suspect that this favoured any of the stent types. Moreover, this was a single-centre investigation and there were no predefined endpoints which may have increased the chances of type 2 error. Therefore, the results of this analysis should be considered hypothesis-generating. Whether the advantage of EES in the setting of STEMI remains when compared to the newer-generation R-ZES has yet to be explored. Large randomised trials with long-term follow-up and sufficient power are necessary to decide which newer-generation stent is most suitable for STEMI patients.
Conclusions
The current retrospective investigation of EES and Endeavor ZES in the setting of STEMI found lower rates of the device-oriented endpoint in EES patients compared to E-ZES patients, driven by lower rates of TLR. This suggests that EES is more efficacious than E-ZES in the setting of ST-elevation myocardial infarction up to three years of follow-up. Furthermore, definite ST rates were low and the strategy of second-generation DES implantation and the administration of upfront GP IIb/IIIa inhibitors appear to be safe in STEMI.
Funding
The Department of Cardiology received research grants from Boston Scientific, Medtronic and Biotronik.
Conflict of interest statement
The authors have no conflicts of interest to declare.

