Abstract
Aims: We examined long-term outcomes after implantation of the Resolute zotarolimus-eluting stent (R-ZES) in ST-segment elevation acute myocardial infarction (STEMI) patients.
Methods and results: We compared long-term outcomes of STEMI patients undergoing primary angioplasty <12 hours from symptom onset who were randomised to the R-ZES (n=122) or the everolimus-eluting stent (EES, n=158) in the RESOLUTE All Comers Trial after propensity score adjustment. The five-year cumulative incidence of target lesion failure (TLF) was 7.6% versus 10.4% among patients treated with R-ZES versus EES, respectively, (adjusted p=0.304), and comprised clinically driven target lesion revascularisation (TLR, 2.5% versus 2.0%, adjusted p=0.766) and cardiac death/target vessel MI (5.1% versus 9.1%, adjusted p=0.123). The five-year cumulative incidence of stent thrombosis was 0.8% for R-ZES patients versus 1.3% for EES patients (adjusted p=0.868). In the RESOLUTE Global Clinical Trial Program, excluding RESOLUTE All Comers, the three-year cumulative incidence of TLF with R-ZES was 9.8% and comprised 7.0% clinically driven TLR and 4.5% cardiac death/target vessel MI.
Conclusions: Patients with STEMI who received R-ZES had excellent long-term clinical outcomes which were similar to those of patients who received EES.
Introduction
Patients with ST-segment elevation acute myocardial infarction (STEMI) are at greater risk of recurrent MI and stent thrombosis (ST) as compared to patients with stable coronary artery disease, probably due to heightened thrombotic milieu1. Autopsies of patients with acute MI who received first-generation drug-eluting stents (DES) demonstrated delayed strut coverage and persistent inflammation and thrombus at the culprit site, as compared with the lesions of stable angina patients2. Treatment of STEMI patients with DES requires evaluation of the patients’ ability to remain on prolonged dual antiplatelet therapy (DAPT). In an urgent setting it is more challenging to evaluate financial or social barriers that may limit patient compliance with DAPT or a possible need for invasive or surgical procedures within the subsequent year.
As compared with first-generation DES, current-generation DES have been associated with improved outcomes3-5. However, most studies in STEMI patients that reported long-term outcomes were with first-generation DES6,7, and there is still limited information on the comparative long-term effectiveness of current-generation DES in STEMI patients8,9. Patients who discontinued DAPT after implantation of the Resolute™ zotarolimus-eluting stent (R-ZES) (Medtronic, Santa Rosa, CA, USA) had low rates of adverse events10, suggesting that R-ZES may be useful in patients at high risk of ST, such as those with STEMI. We examined the long-term comparative effectiveness of R-ZES versus the XIENCE V® everolimus-eluting stent (EES) (Abbott Vascular, Santa Clara, CA, USA) in STEMI patients enrolled in the RESOLUTE All Comers randomised controlled trial. To confirm the applicability of these results to a large population of STEMI patients, we also examined patients in the RESOLUTE Global Clinical Trial Program5,11-13.
Methods
RESOLUTE ALL COMERS TRIAL
We compared the outcomes of STEMI patients randomised to the R-ZES (n=122) or the EES (n=158) in the RESOLUTE All Comers randomised controlled trial11, a real-world study with limited inclusion and exclusion criteria. The study required at least one coronary lesion with ≥50% stenosis and a reference vessel between 2.25 and 4.0 mm in diameter. There were no exclusions on the number of treated lesions or vessels, lesion length, or the number of stents implanted. Patients were randomised 1:1 to R-ZES or EES. STEMI patients were a pre-specified subgroup for analysis and included all STEMI patients who underwent primary percutaneous coronary intervention (PCI) within 12 hours of symptom onset; however, the pooled analysis was not pre-specified. Follow-up was available for five years after randomisation.
RESOLUTE GLOBAL CLINICAL TRIAL PROGRAM
We performed an additional analysis of outcomes in STEMI patients who received an R-ZES using pooled patient-level data from three studies of the RESOLUTE Global Clinical Trial Program, excluding RESOLUTE All Comers: RESOLUTE International12, RESOLUTE China Randomized Controlled Trial5, and RESOLUTE China Registry13, all of which were all-comer trials with similar inclusion and exclusion criteria, endpoint definitions, adjudication processes, and methodologies. RESOLUTE International was a worldwide, single-arm registry with limited inclusion and exclusion criteria that enrolled 2,349 patients treated with R-ZES who were followed for three years12. The RESOLUTE China Randomized Controlled Trial randomised 198 patients to receive the R-ZES and 202 patients to receive the TAXUS™ (Boston Scientific, Marlborough, MA, USA) paclitaxel-eluting stent5. The RESOLUTE China Registry was a single-arm registry that enrolled 1,800 patients who were treated with R-ZES13. Both of these studies, RESOLUTE China Randomized Controlled Trial and the RESOLUTE China Registry, had limited inclusion and exclusion criteria, and patients were followed for three years. At discharge, all patients were prescribed DAPT, consisting of aspirin and an adenosine diphosphate P2Y12 receptor antagonist (clopidogrel, ticlopidine, prasugrel, or ticagrelor) daily, for a minimum of six months.
Informed consent was obtained from all patients enrolled in these studies, and study protocols conformed to the ethical guidelines of the 1975 Declaration of Helsinki. All serious adverse events were adjudicated by an independent clinical events committee for all studies.
The three studies in the RESOLUTE Global Clinical Trial Program, excluding RESOLUTE All Comers, enrolled a total of 4,347 patients treated with R-ZES, of whom 371 were treated for STEMI. To be consistent with the RESOLUTE All Comers definition, the STEMI analysis presented here is limited to the 250 patients who underwent primary angioplasty within 12 hours of symptom onset.
CLINICAL ENDPOINT DEFINITIONS
Clinically driven target lesion revascularisation (TLR) (and target vessel revascularisation [TVR]) was defined as revascularisation at the target lesion (and target vessel) associated with positive functional ischaemia or ischaemic symptoms AND an angiographic minimal lumen diameter stenosis ≥50% by quantitative coronary angiography, or revascularisation of a target lesion with diameter stenosis ≥70% by quantitative coronary angiography without either angina or a positive functional study. The incidence of MI after PCI was defined according to the extended historical definition14,15. Target lesion (and vessel) failure was defined as cardiac death, target vessel MI, or clinically driven TLR (and TVR). Major adverse cardiac events were defined as all-cause death, MI, emergent coronary artery bypass surgery, or repeat clinically indicated target lesion percutaneous or surgical revascularisation. Stent thrombosis was defined as Academic Research Consortium (ARC) definite or probable stent thrombosis14.
STATISTICAL ANALYSIS
Because randomisation of patients to the R-ZES and EES arms in the RESOLUTE All Comers Trial was not also stratified based on presentation of STEMI, we included propensity score adjustment with a Cox regression model when comparing these two STEMI cohorts using the following baseline covariates: age, sex, history of smoking, current smoking, prior PCI, history of hyperlipidaemia, diabetes mellitus, insulin-dependent diabetes mellitus, history of hypertension, prior MI, premature coronary artery disease in first degree relative, prior coronary artery bypass graft surgery, vessel location, American Heart Association/American College of Cardiology lesion class B2/C, moderate or severe calcification, lesion located at a bend ≥45 degrees, Thrombolysis In Myocardial Infarction (TIMI) 3 flow, pre-minimal lumen diameter, pre-diameter stenosis, lesion length, lesions treated per patient, number of stents per patient implanted, total stent length per patient, and multivessel treatment.
All analyses were conducted on an intention-to-treat basis. Continuous parameters were presented as mean±standard deviation and compared using the t-test or the Wilcoxon rank-sum test as appropriate. Nominal parameters were presented as percentages and compared using Fisher’s exact test. The incidence of clinical events was calculated using the Kaplan-Meier method and compared using the log-rank test. P-values <0.05 were considered statistically significant. Analyses were performed using SAS software, version 9.1 or later (SAS Institute, Cary, NC, USA).
Results
RESOLUTE ALL COMERS TRIAL
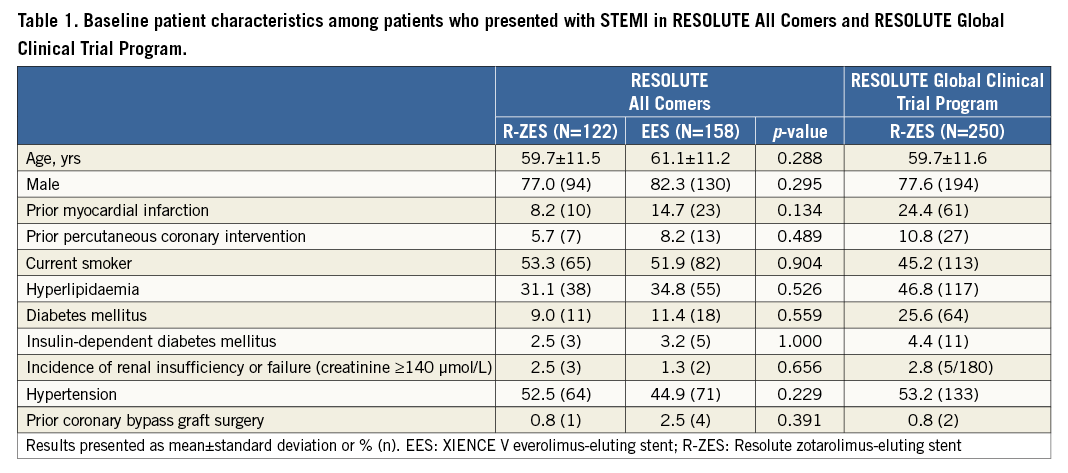
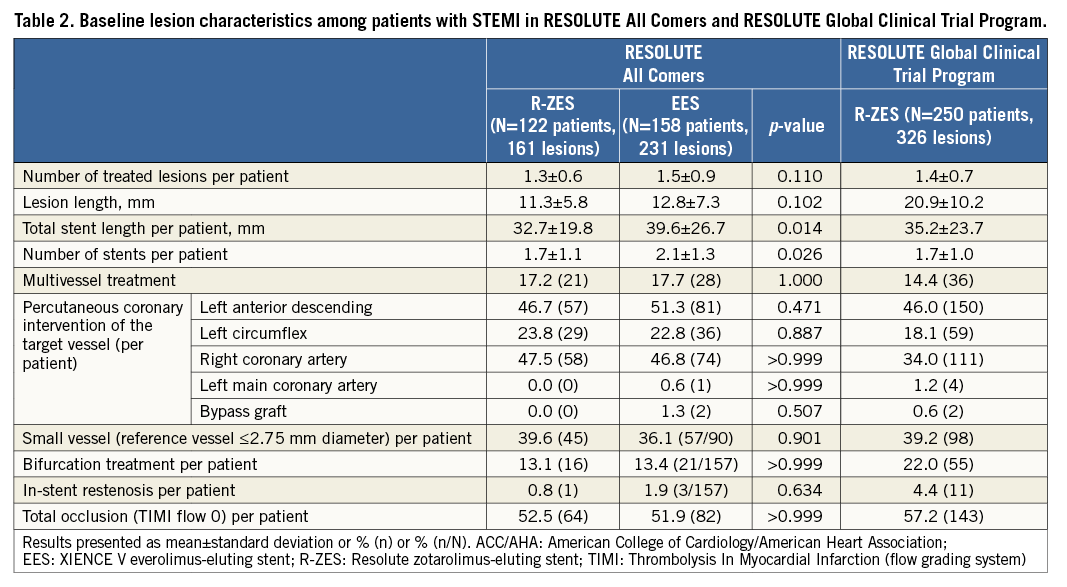
The baseline patient and lesion characteristics in the RESOLUTE All Comers Trial among patients with STEMI treated with PCI within 12 hours of onset of symptoms are shown in Table 1 and Table 2, respectively. Most patients were male, 10% had diabetes mellitus, 13% were treated for a lesion that involved a bifurcation, and more than half had TIMI 0 flow. The R-ZES and EES arms had similar baseline patient and lesion characteristics, including mean lesion length (11.3±5.8 vs. 12.8±7.3 mm, respectively; p=0.102) and number of lesions treated in each patient (1.3±0.6 vs. 1.5±0.9; p=0.110), yet patients in the EES group received more stents (1.7±1.1 vs. 2.1±1.3; p=0.026) and had longer total stent length (32.7±19.8 vs. 39.6±26.7 mm; p=0.014). There were no periprocedural pharmacologic differences between the R-ZES and EES cohorts regarding use of dual antiplatelet therapy (97.5% vs. 98.7%; p>0.999), anticoagulant (including unfractionated heparin or bivalirudin) use (100% vs. 100%; p>0.999), or glycoprotein IIb/IIIa inhibitor use (56.6% vs. 52.5%; p=0.546).
Five-year follow-up was available for 118 (97%) R-ZES and 155 (98%) EES patients. The five-year cumulative incidence of target lesion failure (TLF) among R-ZES and EES patients was 7.6% versus 10.4%, respectively (adjusted p=0.304), and comprised clinically driven TLR (2.5% vs. 2.0%; adjusted p=0.766), and cardiac death/target vessel MI (5.1% vs. 9.1%; adjusted p=0.123) (Table 3, Figure 1). The five-year cumulative incidence of Academic Research Consortium (ARC) definite or probable ST was 0.8% (one subacute event) for R-ZES versus 1.3% (one early and one very late event) for EES patients (adjusted p=0.868). There were no significant differences in five-year clinical outcomes between the two arms except for the composite of all death and target vessel MI (6.8% R-ZES versus 15.4% EES, adjusted p=0.045), which was significantly higher in EES-treated patients (Table 3). Use of DAPT at one year was 91% in both arms but decreased to 15% at two years (15% R-ZES vs. 16% EES; p=0.735) and to 10% at five years (10% R-ZES vs. 8% EES; p=0.657).
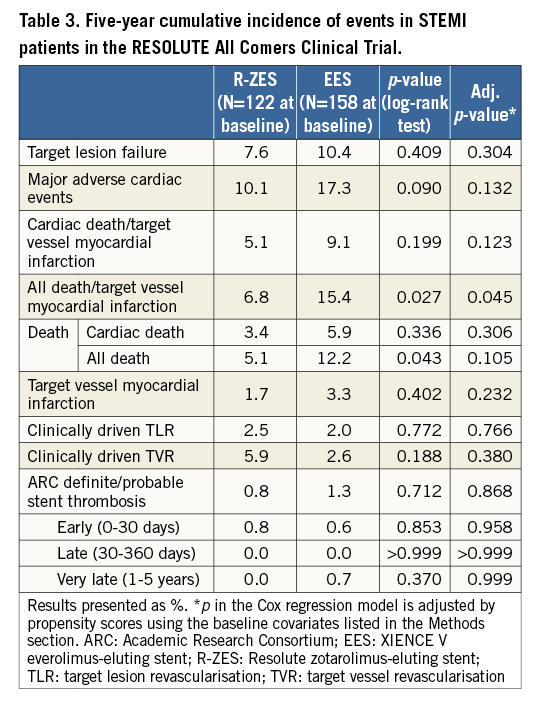
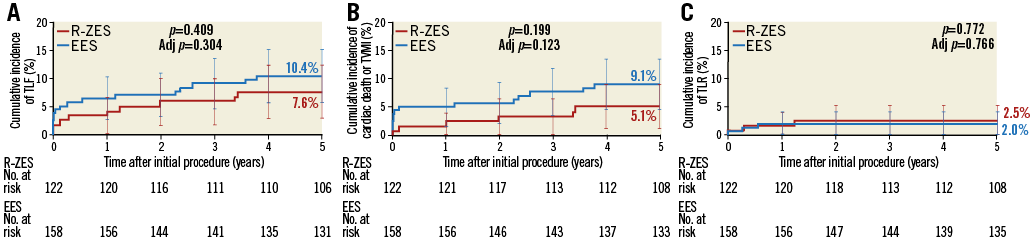
Figure 1. Five-year cumulative incidence of outcomes in the RESOLUTE All Comers randomised controlled study among patients treated with the Resolute zotarolimus-eluting stent (R-ZES) versus the XIENCE V everolimus-eluting stent (EES) for acute STEMI (<12 hours from onset of symptoms to balloon inflation). A) Target lesion failure (TLF) and its components. B) Cardiac death/target vessel myocardial infarction (TVMI). C) Clinically driven target lesion revascularisation (TLR).
One R-ZES patient and 11 EES patients received thrombolytic therapy before PCI in RESOLUTE All Comers; however, exclusion of these patients did not impact on clinical outcomes (data not shown).
RESOLUTE GLOBAL CLINICAL TRIAL PROGRAM
Among the 250 STEMI patients undergoing primary angioplasty <12 hours from symptom onset in the RESOLUTE Global Clinical Trial Program, 165 were from RESOLUTE International, 83 from the RESOLUTE China Registry, and two from the RESOLUTE China Randomized Controlled Trial. Baseline patient and lesion characteristics for patients with STEMI treated with PCI within 12 hours of onset of symptoms in the RESOLUTE Global Clinical Trial Program, excluding RESOLUTE All Comers, are shown in Table 1 and Table 2, respectively. Patients in the RESOLUTE Global Clinical Trial Program were more complex, including a higher percentage of patients with diabetes mellitus (26%), prior percutaneous coronary intervention (11%), and hyperlipidaemia (47%). Additionally, patients in the RESOLUTE Global Clinical Trial Program were treated for longer lesions (21±10 mm), and bifurcation lesions (22%) were more often involved. Periprocedural use of dual antiplatelet therapy, anticoagulant use (including unfractionated heparin or bivalirudin), and glycoprotein IIb/IIIa inhibitor use in STEMI patients was 91.6%, 93.2%, and 60.8%, respectively.
At three years, the incidence of clinically driven TLF was 9.8%, including 7.0% clinically driven TLR, and the incidence of cardiac death/target vessel MI was 4.5% (Table 4, Figure 2). Use of DAPT among patients with STEMI in the RESOLUTE Global Clinical Trial Program, excluding RESOLUTE All Comers, was 94% at 12 months and 37% at three years. The cumulative incidence of early, late, and very late ARC definite or probable ST was 2.0%, 0.8%, and 0%, respectively.
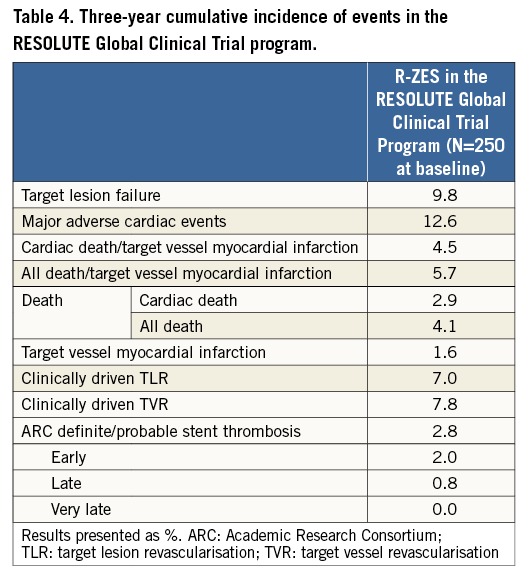
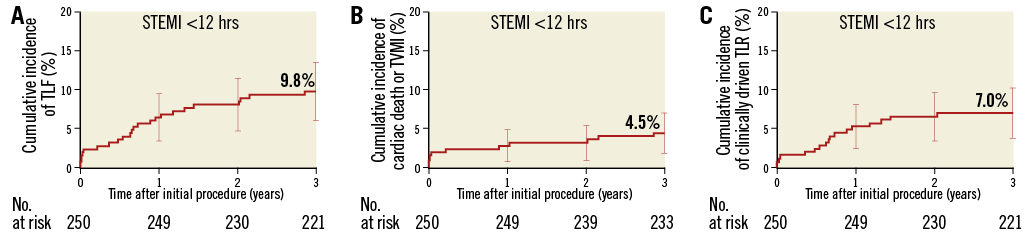
Figure 2. Three-year cumulative incidence of outcomes in the RESOLUTE Global Clinical Trial Program among patients treated with the Resolute zotarolimus-eluting stent for acute ST-elevation myocardial infarction (STEMI) (<12 hours from onset of symptoms to balloon inflation). A) Target lesion failure (TLF) and its components. B) Cardiac death/target vessel myocardial infarction (TVMI). C) Clinically driven target lesion revascularisation (TLR).
Thirteen patients in the RESOLUTE Global Clinical Trial Program, excluding RESOLUTE All Comers, were treated with PCI for STEMI within 12 hours of onset of symptoms after administration of thrombolytics. There were no major adverse cardiac events associated with these patients at three years.
Discussion
The main finding of our study is that, in the RESOLUTE All Comers Trial, STEMI patients receiving R-ZES had similar five-year TLF, cardiac death, and MI as compared with those receiving EES. Furthermore, the incidence of ARC definite ST was low (0.8% versus 1.3%; adjusted p=0.868) at five years, despite low use of DAPT after the first year (~15% at two years and approximately 10% at five years in both arms). The low incidence of adverse clinical outcomes with R-ZES in RESOLUTE All Comers was consistent with that observed with R-ZES across the RESOLUTE Global Clinical Trial Program in acute STEMI patients, demonstrating excellent safety and effectiveness of both R-ZES and EES in this high-risk patient cohort.
A previous analysis on the RESOLUTE Global Clinical Trial Program analysed outcomes at two years in patients with acute coronary syndrome, including STEMI, in RESOLUTE All Comers and RESOLUTE International (N=335)16 and was used to support CE mark approval of R-ZES in patients with acute coronary syndrome, including STEMI, in 2012. Our analysis is unique because it analyses outcomes specifically in STEMI patients, those at greatest risk of adverse events, as well as providing long-term outcomes (five years in the RESOLUTE All Comers randomised controlled trial and three years in the RESOLUTE Global Clinical Trial Program). Our analysis also compares outcomes with R-ZES vs. EES in the RESOLUTE All Comers Trial.
No other studies have evaluated outcomes of STEMI patients treated with R-ZES. However, the Real-World Endeavor Resolute Versus XIENCE V Drug-Eluting Stent Study in Twente (the TWENTE trial) randomised non-STEMI patients to R-ZES or EES and reported a similar incidence of the primary endpoint, TVF (6.9% [1,402] vs. 8.7% [1,806]; p=0.50)17.
Previous meta-analyses have shown superiority of EES to first-generation DES in STEMI patients8,9. Our analysis on outcomes in STEMI patients is important in order to understand outcomes in STEMI patients treated with current-generation R-ZES. Furthermore, although there have been previous publications on the treatment of STEMI with other current-generation DES, most of these studies have not focused on acute STEMI (<12 hours). The Everolimus-Eluting Stents Versus Bare-Metal Stents in ST-Segment Elevation Myocardial Infarction (EXAMINATION) trial enrolled patients within 48 hours of symptom onset18. The time to onset of symptoms was not defined in the COMPARE STEMI analysis19 or the XIENCE V USA STEMI analysis20. In MISSION, however, which randomised patients with STEMI to EES versus Endeavor-ZES, more than 95% of patients were treated for STEMI within 12 hours of onset of symptoms; the one and three-year rates of clinically driven TLF with EES were 4.7% and 9.7%21, respectively, similar to the rates observed in this analysis, 3.3% and 5.8%, in patients treated with R-ZES in RESOLUTE All Comers, and 5.2% and 8.2% in the RESOLUTE Global Clinical Trial Program. Additionally, in the Randomised Comparison of Everolimus Eluting Stents and Sirolimus Eluting Stents in patients with ST elevation Myocardial Infarction (RACES-MI) study, investigators randomised patients with acute STEMI (<12 hours) to EES or the CYPHER® sirolimus-eluting stent (Cordis, Johnson & Johnson, Warren, NJ, USA)22. At three years with EES, the rate of major adverse cardiac events (MACE) was 16%, and the rate of ARC definite/probable ST was 1.6%22, similar to the rates with R-ZES in RESOLUTE All Comers (7.5% MACE and 0.8% ST) and the RESOLUTE Global Clinical Trial Program (11.0% and 2.2%, respectively) at three years.
Although baseline patient and lesion characteristics in RESOLUTE All Comers were similar in patients treated with R-ZES or EES for STEMI, there were some differences in lesion treatment. Treatment with EES resulted in significantly more stents per patient and therefore longer total stent length, suggesting a possible economic benefit with the use of the R-ZES. This observation is also consistent with other studies on EES. In both SPIRIT III and SPIRIT IV3, the number of stents used per lesion, and therefore the total stent length per lesion, was higher with EES as compared with the TAXUS paclitaxel-eluting stent.
Clinical outcomes among patients treated for acute STEMI in the RESOLUTE All Comers study are consistent with those observed in the RESOLUTE Global Clinical Trial Program. The cumulative incidence of TLR at three years in the RESOLUTE Global Clinical Trial Program (7.0%) was numerically higher than that at five years in RESOLUTE All Comers with R-ZES (2.5%) and probably reflects the more complex baseline patient and lesion characteristics (higher percentage of patients with diabetes mellitus, prior PCI, hyperlipidaemia, as well as treatment for longer lesions and lesions more often at a bifurcation) in the RESOLUTE Global Clinical Trial Program, excluding RESOLUTE All Comers. These baseline characteristics have often been associated with higher adverse events23-28.
Historically, bare metal stents were considered the standard of care for patients with acute STEMI, given both the concern of very late stent thrombosis with first-generation DES and the concern of prolonged DAPT after implantation of DES in a patient population in which compliance with DAPT before stent implantation cannot always be confirmed. The 2013 American College of Cardiology/American Heart Association STEMI guidelines provided a class IA recommendation for the use of a DES or bare metal stent (BMS) for primary PCI in STEMI. However, a BMS is recommended for patients in whom one year of DAPT may not be possible (due to tolerance, compliance, or anticipated surgery)29. There is some reassurance with the R-ZES given that DAPT interruption between one and 12 months has been shown to be associated with low rates of ST and adverse cardiac outcomes10. The most recent European Society of Cardiology guidelines on coronary revascularisation recommend new-generation DES over BMS for primary PCI (class IA)30.
Limitations
The relatively small sample size used in this analysis could have limited the power to detect differences between the R-ZES and the EES; however, the incidence of events was numerically lower in the R-ZES group. The RESOLUTE Global Clinical Trial Program enrolled various populations from multiple countries, a possible source of heterogeneity. The advantage of the pooled analysis, however, is the addition of 250 patients revascularised with R-ZES after STEMI <12 hours from onset of symptoms and the truly global origin of the results, enhancing the applicability of the findings. The consistently low incidence of long-term outcomes after implantation with R-ZES after STEMI <12 hours from onset of symptoms in both the RESOLUTE All-Comers trial and the RESOLUTE Global Clinical Trial Program provides reassurance that results apply to different clinical practices and ethnic groups throughout the world.
Conclusion
Patients with acute STEMI (<12 hours from onset of symptoms) who received an R-ZES had good long-term (five-year) clinical outcomes which were similar to those of patients who received an EES. These findings were confirmed in a larger cohort of patients, demonstrating the long-term efficacy and safety of current-generation DES for the treatment of patients with STEMI.
| Impact on daily practice Patients who undergo primary PCI for ST-segment elevation acute myocardial infarction are at increased risk for subsequent adverse cardiovascular events. Our analysis of 530 primary PCI patients demonstrated good long-term (five-year) clinical outcomes after implantation of the Resolute zotarolimus-eluting stent that were similar to those of the everolimus-eluting stent. |
Guest Editor
This paper was guest edited by David Kandzari, MD; Piedmont Heart Institute, Atlanta, GA, USA.
Acknowledgements
We thank Nicole Brilakis, MS, MBA, and Colleen Gilbert, PharmD, CMPP, for editorial assistance and Minglei Liu, PhD, and Yun Peng, MS, for statistical analysis and oversight (all from Medtronic).
Funding
This study was funded by Medtronic. Clinical Trial Registration—URL: http://www.clinicaltrials.gov. Unique identifiers: RESOLUTE All Comers, NCT00617084; RESOLUTE International, NCT00752128; RESOLUTE China Randomized Controlled Trial, NCT01334268; and RESOLUTE China Registry, NCT01243749.
Conflict of interest statement
C. Di Mario and S. Silber have received a research grant from Medtronic (regarding the RESOLUTE All Comers Trial). P. Widimsky receives minor speaker’s honoraria from Medtronic. S. Windecker reports having received research grants from Biotronik and St. Jude Medical and honoraria from Abbott, Biotronik, Medtronic, AstraZeneca, Eli Lilly, and Daiichi Sankyo. The other authors have no conflicts of interest to declare. The Guest Editor receives research/grant support from Abbott Vascular, Biotronik, Boston Scientific Corporation, Medinol and Medtronic CardioVascular and consulting honoraria from Boston Scientific Corporation and Medtronic CardioVascular.