KEYWORDS
Abstract
Aims: To report long-term outcome data on the V technique using drug-eluting stents.
Methods and results: From April 2002 to December 2006, 31 consecutive patients were successfully treated with V stenting of a de novo bifurcation lesion. The technique involves the deployment of two stents in the two branches of a bifurcation, the proximal edges of the stents just touching one another. Patients exclusively received either sirolimus- (10), paclitaxel- (20) or biolimus-eluting (one) stents. On average, 1.5±0.8 stents with a total length of 26.6±17.2 mm and 1.1±0.4 stents with a total length of 18.3±7.6 mm were deployed in the distal main vessel and side branch respectively. Mean duration of follow-up was 853±553 days. Within 30 days, three patients died; two other patients had definite stent thrombosis involving the V stents, both requiring re-PCI. Beyond 30 days and within one year, there was one death and three cases of target vessel revascularisation, including one target lesion revascularisation. There were a further three deaths (one cardiac) beyond one year. Eleven patients (35.5%) had angiographic follow-up, exhibiting a binary restenosis rate of 9.1% at 203±33 days.
Conclusions: In this real-world cohort, late clinical events stand in accord with studies on competitive techniques, but early outcome was less encouraging, probably due to the baseline risks.
Introduction
The optimal technique for treating bifurcation lesions with percutaneous coronary intervention (PCI) has not been clearly established. There is particularly little outcome data on V stenting in the current drug-eluting stent (DES) era. The V stenting technique scaffolds both distal limbs of a bifurcation lesion from the carina onwards and is only suitable when the lesion spares the proximal main vessel (PMV)1. In treating bifurcation lesions, optimal coverage without any un-stented gaps is essential for optimal scaffolding and drug delivery to mitigate the restenotic process2-4. Recently, various groups have described the Simultaneous Kissing Stents (SKS) technique – the simultaneous deployment of the distal main vessel (DMV) and side branch (SB) stents so that the new apposing struts from the two adjacent stents extended proximally from the carina5-7 for 8±5 mm5 or 8.9±2.5 mm6. Preliminary angiographic6 and histologic7 results showed that a new carinal membrane developed on these struts. While this technique can handle proximal disease close to the carina, the PMV receiving the two stents is often over-dilatated with its attendant risks5. A newer approach is to implant in the PMV a conical self-expandable Axxess (Devax, Irvine, CA, USA) stent with a “flared” distal part covering the outer rim of the bifurcation and two stents distally with V technique to scaffold the inner rim. To facilitate progress in this field, noting the possible dreaded complication of late stent thrombosis8, we reviewed the long-term outcome of V stenting using DES from April 20029 to December 2006.
Methods
Study population
On April 16, 2002, our institution began to use sirolimus-eluting stents (SES, Cypher, Cordis Corporation, Warren, NJ, USA) as the default strategy for every PCI, until Feb 16, 2003 when paclitaxel-eluting stents (PES, Taxus, Boston Scientific, Natick, MA, USA) became our default strategy. Data were recorded in the Rapamycin-Eluting Stent Evaluated at Rotterdam Cardiology Hospital (RESEARCH) registry10 and the Taxus Stent Evaluated AT Rotterdam Cardiology Hospital (T-SEARCH) registry11. From April 2002 to December 2006, 656 procedures involving treatment of de novo bifurcation lesions were performed in 638 patients. Out of this cohort, and after reviewing the angiographic films, we identified 31 consecutive patients, who had one bifurcation lesion successfully treated with V stenting; none of them had a second procedure involving this technique. Written informed consent was obtained from all patients prior to the procedure.
Procedure
V stenting is defined as the delivery and implantation of two stents in the two branches of a bifurcation; one stent is deployed in the DMV and the other one in the SB12. The stents can be deployed either concurrently or in a successive mode13. The latter is presumably an acceptable alternative, provided that the second stent is deployed concurrently with a balloon inflated in the first stent, to protect this from being crushed; systematic post-dilation with kissing balloons should be performed. To differentiate from the SKS technique, we defined V stenting as the proximal edges of the stents just touching one another without any significant overlap, protruding into the PMV by no more than 5 mm12 (Figure 1).
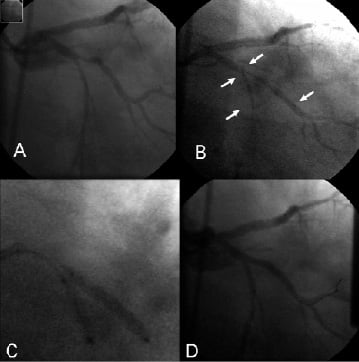
Figure 1. Illustration of V stenting technique. A. Typical 0,1,1 bifurcation lesion involving the left circumflex (LCX) and the obtuse marginal (OM) branch (distal main vessel). B. Two sirolimus-eluting, Cypher, stents have been advanced into position. The 3.0 x 23 mm stent is in the OM, the 2.5 x 13 mm stent is in the LCX. Arrows point at the stents’ markers; the proximal markers barely touch each other, not protruding into the proximal main vessel. C. Both stents are simultaneously deployed. D. Final result.
All procedures were performed according to current interventional standards at the time. The use of predilation, post-procedure kissing balloon inflation and the use of glycoprotein IIb/IIIa inhibitors was left to the operators’ discretion. During the procedure, intravenous heparin was administered, in order to maintain an activated clotting time above 250 seconds. All patients were prescribed 80 mg of aspirin lifelong and were pretreated with 300 mg clopidogrel followed by 75 mg clopidogrel for at least six months.
Clinical definitions and follow-up
Angiographic success was defined as residual stenosis <30% by visual estimation in the presence of Thrombolysis In Myocardial Infarction (TIMI) grade 3 flow. Clinical success was defined as angiographic success without the occurrence of death, myocardial infarction or repeat revascularisation of the target lesion during the hospital stay. Myocardial infarction was diagnosed by an increase in creatine kinase-MB fraction of three times the upper limit of normal, according to American Heart Association / American College of Cardiology guidelines14. Target lesion revascularisation (TLR) and target vessel revascularisation (TVR) were defined according to the Academic Research Consortium (ARC) recommendations15; they were adjudicated as clinically indicated, only if driven by symptoms/ objective signs of ischaemia and a percent diameter stenosis exceeding 50% on follow-up angiography. Clinical events were recorded in two ways: firstly, as composite major adverse cardiac events (MACE), including all-cause death, nonfatal myocardial infarction and TVR and secondly, in the form of the ARC recommended device-oriented composite, including cardiac death, myocardial infarction (not clearly attributable to a non-target vessel) and TLR.
We applied ARC recommendations to adjudicate stent thrombosis. Angiographically defined thrombosis with TIMI grade 0 or 1 flow or the presence of a flow-limiting thrombus accompanied by acute symptoms was considered as definite stent thrombosis. Unexplained death was adjudicated as probable stent thrombosis if occurring within 30 days, and as possible stent thrombosis if after 30 days15. Stent thrombosis was further categorised according to the timing of the event into acute (within 24 hours), subacute (24 hours-30 days), late (30 days-1 year) and very late (beyond one year). We retrieved electrocardiographic (ECG) information on patients with myocardial infarction for adjudication.
Data sources for both registries included municipal civil registries for survival status, information from health questionnaires, medical records, and information from local physicians on repeat coronary interventions (surgical or PCI), myocardial infarction and medication usage 10, 11.
Angiographic evaluation
The bifurcation lesions were adjudicated according to the Medina classification16 after reviewing the pre-procedure images. Quantitative coronary angiographic (QCA) analysis was performed by means of dedicated bifurcation QCA software (CAAS 5.4, Maastricht, PIE Medical software, The Netherlands) (Figure 2); the relevant methodology employing a ten-segment model for the bifurcation lesion has already been described17. Angiographic parameters, namely minimal lumen diameter (MLD), interpolated reference vessel diameter (RVD) and percentage diameter stenosis (DS), were independently determined both within the stent(s) and within the segment(s). These parameters were measured pre-procedure, post-procedure and, when available, at follow-up. In the case of a chronic total occlusion (CTO), the MLD equals 0 mm, %DS equals 100% and RVD cannot be determined. Late lumen loss (LLL) was calculated as the difference in MLD between post-procedure and follow-up. Angles between the PMV and SB (proximal bifurcation angle) and between DMV and SB (distal bifurcation angle) were automatically determined. Binary angiographic restenosis was defined as DS ≥50% at follow-up.
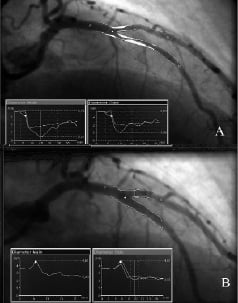
Figure 2. Quantitative coronary angiography of a bifurcation lesion involving the left anterior descending (LAD) and the diagonal branch (side branch). Automatic contour detection pre-procedure (A) and post-procedure (B). Images include the corresponding diameter plots for the main branch and the side branch (CAAS 5.4, Maastricht, PIE Medical software, The Netherlands).
Statistical analysis
Categorical variables are presented as counts and percentages, whereas continuous variables are expressed as mean ± standard deviation. A comparison of angiographic variables both between pre and post and between post and follow-up was performed with a Wilcoxon signed rank test. A p- value of <0.05 was considered significant. Statistical analysis was performed using commercially available software (SPSS 12.0 for Windows, SPSS, Chicago, IL, USA).
Results
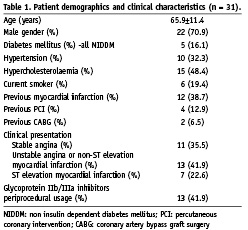
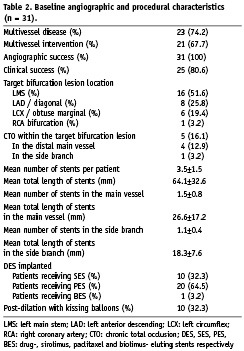
The baseline demographics and procedural characteristics in the 31 patients are reported in Tables 1 and 2. PCI was performed in 20 (64.5%) patients for an acute coronary syndrome (22.6% with ST elevation myocardial infarction and 41.9% with unstable angina or non-ST elevation myocardial infarction). Twenty-three patients (74.2%) had multivessel disease and 12 of them (38.7%) had interventions to at least one additional major epicardial vessel beyond the target vessels. All patients received exclusively one type of DES; Taxus and Cypher stents were implanted in 20 and 10 cases respectively. There was a single patient who received exclusively biolimus-eluting stents (BES, Biomatrix, Biosensors, Singapore); he was recruited in a research study and had no clinical event during the follow-up period. The average number of stents was 3.5±1.5 per patient with a total stent length 64.1±32.6 mm. However, regarding the bifurcation lesion itself, 1.5±0.8 stents with a mean total length of 26.6±17.2 mm and 1.1±0.4 stents with a mean total length of 18.3±7.6 mm were deployed in the DMV and SB respectively. All patients had Medina bifurcation lesion classification of 0,1,1 for the lesion receiving V stenting. The left main bifurcation was the location of the lesion in the majority of the cases (16 cases-51.6%); the lesion involved the left anterior descending (LAD)/diagonal bifurcation in eight cases, the left circumflex (LCX)/obtuse marginal bifurcation in six cases and the distal right coronary artery (RCA) bifurcation in one case. Stents were deployed simultaneously at all times, whereas post-dilation with kissing balloons was performed in 10 cases (32.3%); glycoprotein IIb/IIIa inhibition was employed in 13 cases (41.9%).
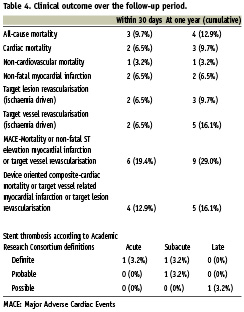
Thirty-day outcome
Within 30 days, three patients died (patients 1, 2 and 3 in Table 3). The first death was regarded as non-cardiovascular, since the patient succumbed to hospital acquired pneumonia after a stroke, whereas patient 2 was adjudicated to have probable stent thrombosis. Patient 3 could not be saved despite a rescue procedure for cardiogenic shock after failed thrombolysis, and died of heart failure. Two other patients had definite stent thrombosis and required emergency PCI, one on day 0 and one on Day 5. The latter (patient 4 in Table 3), a 78-year old man suffering a heart attack five days after a prostate operation, had a cerebral haemorrhage on day 4 and therefore aspirin and clopidogrel were discontinued; the stents occluded the very next day. Finally, another patient who had the V stents placed at the left main bifurcation, and also had intervention on a sub-totally occluded venous graft to his right coronary artery, had a myocardial infarction on the same day; ECG changes pointed to the treated graft as the culprit.
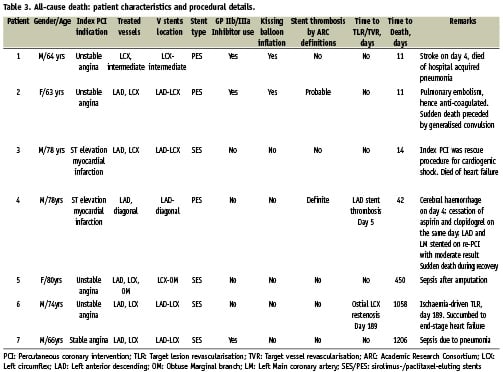
Late clinical outcome
Survival status was available in every patient for ≥ 12 months after the initial PCI. The mean duration to the last follow-up or to death was 853±553 days. Beyond 30 days, and within a year, there was one more death (Table 4). Patient number 4 in Table 3 died on day 42 while recovering from the cerebral haemorrhage; this sudden death was adjudicated as possible stent thrombosis. Three patients required a target vessel revascularisation, but in only two were the bifurcation V stents the targets for re-intervention. One patient underwent repeat coronary angiography and subsequently reintervention on day 160 upon referral for unstable angina. He had a mid-LAD in-stent restenosis of 70% and a borderline 50% (by visual estimation) ostial LAD restenosis, involving the V stents implanted at the LAD-LCX bifurcation. The former lesion was deemed the culprit lesion and was re-stented with a DES, whereas the latter was also treated with a DES deployed in the distal left main into the proximal LAD, fenestrated to the LCX; the procedure was completed with a kissing balloon inflation. However, QCA analysis ascribed a 43.9% stenosis to the ostial LAD restenotic lesion; thus this was not adjudicated as an ischaemia-driven revascularisation. Another patient with LAD-LCX V stents, had a re-study on day 189 revealing ostial LCX in-stent restenosis, which was treated with balloon dilatation. No patients had reinfarction beyond 30 days (Table 4). There were a further three deaths on days 450, 1058, 1206; the causes of death were respectively sepsis, end-stage heart failure and sepsis and none was adjudicated as having stent thrombosis (Table 3). The patient who died of heart failure was actually the single ischaemia-driven TLR case. The overall rates of mortality and other clinical endpoints within 30 days and 1-year (cumulative) are summarily reported in Table 4.
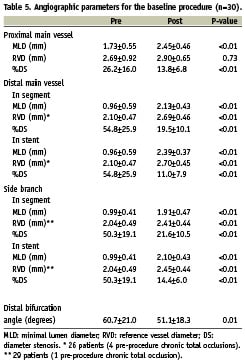
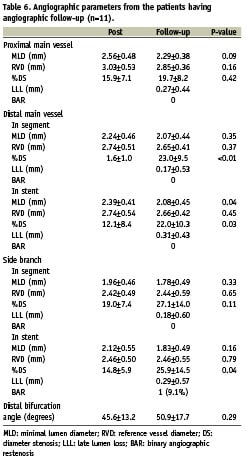
Quantitative angiographic analysis
Analysis of the baseline procedure could be done for 30 out of the 31 patients (Table 5); we could not retrieve post-procedure images for one case. Out of the 30 baseline procedures analysed, there were five cases involving a CTO, therefore the preprocedure RVD and the bifurcation angulation parameters could not be determined. In 11 cases, there was minimal stent protrusion into the PMV (2.23±0.72 mm), however never exceeding 5 mm or the respective RVD of the PMV; in three cases the protrusion was actually less than half the respective RVD. Angiographic follow-up (at a period of 203±33 days) was available for 11 patients (35.5%); data are presented in Table 6. Out of this group, eight patients underwent routine control coronary angiography and presented no binary angiographic restenosis of the target bifurcation lesion; out of the three patients who were referred for anginal symptoms (two with stable angina and one with unstable angina), one patient had binary in-stent restenosis. Thus, this cohort exhibited a restenosis rate of 9.1% (1/11). The LLL in the DMV and SB was 0.17±0.53 mm and 0.18±0.60 mm in-segment and 0.31±0.43 mm and 0.29±0.57 mm in-stent respectively. Sixteen cases exhibited a Y anatomical configuration regarding the bifurcation treated, whereas nine were T-shaped; the distal bifurcation angle was smaller than 70 degrees in the former and larger in the latter.
Discussion
This paper reports a real-world experience on V stenting technique using DES. The paucity of outcome data after V stenting reflects that this technique is rarely performed9; the current series of 31 patients were collected over nearly five years. A percentage of 13.7% has been reported18 regarding the frequency of the type 4 bifurcation lesion according to the ICPS classification system, which is the equivalent of the 0,1,1 lesion in the Medina classification. Even if this is per definition, the ideal lesion configuration for the implementation of V stenting, similar techniques such as Simultaneous Kissing Stents claim a great share of those procedures, accounting for the rarity of V stenting.
Many techniques have been described to treat bifurcations, reflecting the lack of a perfect solution. Although the proposed strategy would be stenting the main branch with provisional stenting of the side branch, this would not apply in this setting; a bifurcation lesion involving a large side branch with a long stenosis certainly calls for a two-stent strategy. With the Crush technique, bench studies revealed that stent deployment even after kissing balloon inflation is often suboptimal and associated with malapposition4,19, findings corroborated by intravascular ultrasound studies20. Stent under-expansion could predispose to higher restenosis rate and thrombotic risk21,22. Less data has accumulated for Culotte stenting in the current DES era, but this technique has attracted renewed attention23,24.
Early outcome
The admittedly less than desirable early outcome (MACE rate of 19.4%) should be interpreted in the context of unstable clinical presentation, extensive coronary disease and a multitude of aggravating factors. This series bears the highest rate (64.5%) of acute coronary syndrome as the clinical presentation compared to other relevant studies in the DES era (13.3-62.0%)2,3,6,7,24,25; moreover the rates of multivessel disease (74.2%), multivessel intervention (67.7%), intervention on additional major epicardial vessels beyond the target vessels (38.7%) and the rate of left main stem stenting (51.6%) rank high among the corresponding studies. Out of the three deaths occurring within 30 days, none was clearly attributable to the PCI itself, even though two of them were adjudicated as cardiac. One was due to cardiogenic shock, not reversed by a rescue procedure after failed thrombolysis, and the other one had to be adjudicated as probable stent thrombosis, recent pulmonary embolism notwithstanding; an autopsy was not performed.
As to the two definite stent thrombosis cases, both of them presented with ST elevation myocardial infarction; neither of them was treated with glycoprotein IIb/IIIa inhibitors at index procedure, most probably due to old age; cessation of both antiplatelet agents in the second case was undoubtedly the major contributor to the stent thrombosis within 24 hours. Interestingly, in these two cases, stent protrusion by QCA was either trivial on non-existent. The remaining case of myocardial infarction was related to the concomitant intervention on the sub-totally occluded saphenous vein graft. Applying the ARC recommended device-oriented composite, the event rate substantially drops (12.9%), not adjusting however for the aforementioned circumstances.
Late outcome
Contrary to the early outcome, event rates at one year excluding the first 30 days, are close to the corresponding values reported in the vast majority of the relevant literature. As a matter of fact, cumulative 1-year TVR and TLR rates (16.1% and 9.7% respectively) compare favourably to DES studies employing Crush (11.0% TVR and 9.7% TLR at nine months)25, Culotte (11.1% TVR and 8.9% TLR at nine months)24, T stenting (TVR and TLR 27.3% at nine months)24, SKS (TLR 4.0-13.9%)5,6 and mixed cohorts (TLR 4.3-9.5 at six months)2,3,9. Equally amenable are the angiographic features (low LLL in both branches and low binary restenosis rate), despite the increased average number of stents and total stent length implanted. Of note, in the RESEARCH and T-SEARCH registries10,11, the average stent length was 38.7±23.7 mm and 42.9±31.2 mm respectively. The Nordic Bifurcation Study stands out due to its strikingly low rates of events (3.4% MACE and 1.0% TLR at six months in the two stent arm); however, this is offset by leaving the much higher angiographic restenosis (16.0%) unattended26. Over an average of 853 days of follow-up, there was only one case of possible late stent thrombosis.
Unlike the Crush or Culotte techniques, the V stenting technique does not deform conventional tubular stents. It allows the operator to preserve access to both branches throughout the procedure, without the need to rewire. However, this has to be traded against the possibility of using a smaller guiding catheter, since a guiding catheter of at least 7 Fr for the Taxus stent or even 8 Fr for the Cypher stent, is required for simultaneous stent deployment12. Moreover, great precision is required for accurate positioning of the stents, in order to avoid geographic miss or protrusion into the PMV. When the PMV is also involved (i.e. Medina classification 1,1,1), usage of dedicated devices such as the Devax stent to deal with the proximal lesion in the main vessel combined with V stenting of the bifurcation should provide full coverage of the lesion with minimal overlapping of the stent struts. The recent multicentre Axxess Plus trial27 on 139 patients receiving the Axxess (Devax) stent, reported satisfactory outcome at 6-months with a TLR rate of 7.5% and angiographic in-stent LLL of 0.09 mm. However, only 77.7% of patients were regarded as having “true” bifurcation lesions involving both the PMV and SB and only 41.9% had stenting of both DMV and SB27. Future studies with V stenting, plus a proximal dedicated device for more challenging bifurcation lesions, are eagerly awaited.
Limitations
An obvious limitation to this analysis is the small number of patients involved. This precluded us from performing any kind of subgroup analysis; we could not compare events in the DMV and the SB or study the influence of variables, such as the type of DES, the clinical indication, the number of stents and total stented length, the location of the bifurcation lesion and last, but not least, the impact of angulation on the short- and long-term outcome. Even more limited was the rate of angiographic follow-up (35.5%), which was not routinely acquired. Regrettably, IVUS images were not available; in this setting they would have verified complete and accurate lesion coverage and adequate stent struts apposition. Finally, this is a retrospective, single-centre study, with no control arm. This does not allow us to favour or discredit the technique at hand.
Conclusions
We provided long-term outcome data on an unselected cohort who had V stenting of de novo bifurcation lesions with drug-eluting stents. It is a technique dedicated to a distinct anatomic dataset. Early outcome looks less than encouraging, but on closer scrutiny could appear circumstantial and endpoint-dependent; late outcome, on the other hand, stands in accord with competitive techniques and merits further evaluation.

