Abstract
Aims: This study sought to evaluate the reproducibility of the index of microcirculatory resistance (IMR) in a follow-up model and the role of epicardial artery stenosis and central venous pressure (Pv) on IMR.
Methods and results: Twenty-two patients with stable coronary artery disease underwent coronary catheterisation at baseline and after seven weeks. The IMR was calculated at baseline and follow-up in several ways: as IMRuncorrected=Pd·Tmn (Pd: intracoronary pressure distal to the stenosis; Tmn: transit mean time); IMRcorrected=Pa·Tmn·(Pd - Pw)/(Pa–Pw), (Pw: coronary wedge pressure; Pa: aortic pressure); and as IMRcentral venous pressure (IMRcvp)=(Pa–Pv)·Tmn·(Pd–Pw)/(Pa–Pw). By neglecting Pw, IMR was overestimated irrespective of the haemodynamic severity of the epicardial stenosis (baseline: IMRuncorrected=15.5±8.9 U vs. IMRcorrected=13.5±8 U, p<0.001; follow-up: IMRuncorrected=16.9±4.9 U vs. IMRcorrected=13.8±4.6 U, p<0.001). In the intra-individual analysis IMR did not differ between the two time points. The IMRcvp equalled the IMRcorrected at all time points.
Conclusions: IMR is a reproducible index in follow-up studies, independent of any overestimation existing when collateral flow status is neglected. Pv can be neglected for calculation of the IMR.
Introduction
The coronary microcirculation is critical for the clinical outcome of patients with or without coronary artery disease1-4. Recently, invasive methods for assessment of the coronary microcirculation have gained ground, as they allow quantitative measurements and are readily applicable and easily combined with other methods during cardiac catheterisation. The measurement of coronary flow reserve (CFR) is limited in the evaluation of microcirculatory resistance, as it is influenced by the flow status of both the epicardial arteries and the microcirculation5. A novel index for the evaluation of microcirculatory resistance (IMR) has been proposed6. The index can easily be acquired by using a single pressure wire and the thermodilution technique. When the coronary wedge pressure (Pw) is known, IMR enables calculation of vascular resistance independent of the status of the epicardial arteries7. This hypothesis has so far been investigated in humans before and after coronary artery stenting, which may lead to immediate changes in microvascular resistance and collateral artery flow8-11. The performance of a coronary intervention in all previous studies did not allow a conclusion on the reproducibility of the index to be drawn. Furthermore, all previous trials assessed IMR by neglecting the venous pressure, supposing that it had no relevant influence on the intracoronary pressure measurements. However, whether the central venous pressure can be neglected for estimation of the pressure gradient across the microvasculature remains elusive.
The aim of this trial was, for the first time, to assess in patients with chronic coronary stenoses: 1) the reproducibility of the IMR in follow-up measurements; 2) the influence of the haemodynamic severity of epicardial stenoses and collateral blood flow on the IMR, in the absence of any coronary intervention; and 3) the role of central venous pressure in the accurate calculation of the IMR.
Methods
PATIENTS
A total of 22 patients (age 61±11 years) with stable coronary artery disease were recruited. All patients met the following inclusion criteria: 1) angiographic narrowing (>70%) of at least one coronary artery diagnosed by visual assessment within the previous two months; 2) no previous infarction in the myocardial region of interest (ROI) for assessment of collateral blood flow; 3) positive non-invasive ischaemic testing in the ROI; 4) pressure-derived fractional flow reserve <0.8; and 5) normal left ventricular function.
The study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the ethics committee of the Charité-Universitätsmedizin Berlin, Germany, in September 2006. All patients gave written informed consent prior to enrolment.
STUDY PROTOCOL
The aim of the Art.Net.-2 trial was to assess the effect of external counterpulsation (ECP) on collateral artery growth. A detailed protocol has already been reported12,13. Briefly, the patients were divided into two groups: one group of patients (n=15) underwent seven weeks of ECP therapy (35 hours of therapy). The other group (n=7) served as a control. All patients underwent a cardiac catheterisation at baseline and at the seven-week follow-up.
In the three weeks prior to the baseline invasive assessment, oral antihypertensive medication was adjusted to meet the guideline recommendations14. Throughout the study, patients were instructed not to change their daily activity. Patients were eligible for inclusion as soon as haemodynamic significance was proven via FFR. Baseline medication remained unchanged thereafter and throughout the study. To prevent bias, blinded analysis of the invasive data was performed by an experienced cardiologist.
CARDIAC CATHETERISATION PROCEDURE
Cardiac catheterisation was performed on a standard angiography suite (Hicor; Siemens, Erlangen, Germany). Catheters without side holes were used. Weight-adjusted heparin was administered intravenously. Left ventricular end-diastolic pressure was determined at the beginning of the procedure. Intracoronary nitroglycerine (0.2 mg) was injected into the vessel of interest and repeated every 20 minutes throughout the procedure. Routine biplane coronary diagnostic angiography was performed and coronary artery stenosis was assessed by quantitative coronary arteriography (QCA) offline. The same protocol was repeated at baseline and during follow-up.
HAEMODYNAMIC MEASUREMENTS
A 10-minute interval was allowed for dissipation of the effect of the non-ionic contrast agent on coronary vasomotion. The stenosis of interest in a major coronary artery was assessed by FFR. Bypass grafts were not assessed. The mean aortic pressure (Pa, mmHg) was measured via the guiding catheter, and mean central venous pressure (Pv, mmHg) was measured with a catheter placed in the right atrium. Mean distal coronary pressure (Pd, mmHg) and transit mean times (Tmns) were obtained using a 0.014″ guidewire (PressureWire®; St. Jude Medical, St. Paul, MN, USA) positioned distal to the stenosis. The position of the pressure wire in relation to the stenosis was carefully documented in biplane angiography to be repeated at follow-up. Steady-state hyperaemia was achieved with adenosine i.v. (140 μg∙kg–1∙min–1). Three consecutive thermodilution curves were obtained by brisk injection of 3 mL of saline at room temperature into the coronary artery. Data were displayed in real time (RadiAnalyzer Xpress; St. Jude Medical, St. Paul, MN, USA). The pressure-derived collateral flow index (CFIp) was assessed consecutively. To measure collateral artery flow in the ROI, a balloon was placed over the pressure wire proximal to the stenosis in the non-stenotic segment. For measurement of coronary wedge pressure (Pw, mmHg), the balloon was inflated at low pressure (1-3 atm) until antegrade coronary flow was interrupted. The balloon remained inflated for 60 s. This transient complete occlusion was controlled via real-time pressure measurement display and injection of contrast dye.
CALCULATION OF INDEXES
The FFR was calculated as follows: FFR=Pd–Pv/Pa–Pv15. CFIp was determined during a 60 s occlusion and calculated as CFIp=Pw–Pv/Pa–Pv16. CFR was calculated as the ratio of the resting Tmn divided by the hyperaemic Tmn.
The IMR at maximal hyperaemia was calculated in several different ways7:
1. To calculate the IMRuncorrected, Pd and Tmn under hyperaemia were used:
![]()
2. To calculate the IMRcorrected and evaluate the influence of collateral flow on microvascular resistance, the Pw was also taken into account:
![]()
3. To calculate the IMRcentral venous pressure (IMRcvp) and implement the effect of haemodynamic loading conditions, the Pv was taken into account7:
![]()
On the basis of earlier studies on thermodilution17,18, we assessed the variability between each set of three Tmns defined as:
![]()
where ai(1,2,3) corresponds to each Tmn (rest/hyperaemia at baseline and follow-up) and ā corresponds to the mean transit time of each series of three measurements.
Statistical methods
The data are presented as means±SD. Test of normality was performed prior to statistical analysis. Two-tailed paired t-tests were used to compare changes of the haemodynamic parameters from baseline to follow-up and between corrected and uncorrected IMR. Unpaired t-tests were used for comparisons between the groups at baseline and follow-up. Linear regression analysis and multiple regression were used to test the relationship between IMR, CFR, FFR, and CFIp values at each time point. Variability of the Tmn at baseline and during hyperaemia was tested by the Wilcoxon signed-rank test. Statistical significance was defined as p<0.05. All analyses were performed with SPSS for Windows, Version 15.0 (SPSS Inc., Chicago, IL, USA).
Results
CLINICAL CHARACTERISTICS
Twenty-two chronic coronary stenoses were assessed twice in 22 patients (17 males), at baseline and after seven weeks. Forty-five percent of the patients had two-vessel disease (stenoses >50%) and 23% had three-vessel disease. All patients (100%) had hypertension, and 21 out of 22 (95.5%) had hyperlipidaemia. Eighteen percent of the patients had diabetes, and 14% were active smokers at the time of study inclusion. Twelve out of the 22 patients had smoked previously. No gender-based differences were present.
INVASIVE RESULTS
The Art.Net.-2 trial showed that CFIp (0.08±0.05 to 0.15±0.07, p<0.001) and FFR (0.68±0.1 to 0.79±0.12, p=0.001) increased significantly in the group treated with ECP, whereas no change in these indices was found in the control group13. Importantly, the degree of coronary stenosis, assessed by QCA, remained unchanged between the two invasive measurements, indicating a haemodynamic benefit due to an improved coronary collateral circulation.
As presented in Table 1, the IMR at maximal hyperaemia was overestimated at each time point when the actual Pw was not taken into account. At baseline and at follow-up, IMRuncorrected was higher than IMRcorrected (baseline 15.5 vs. 13.5 U, p<0.001, and follow-up 16.9 vs.13.8 U, p<0.001). The overestimation of IMR (ΔIMR=IMRuncorrected-IMRcorrected) was positively correlated with the CFIp (r=0.3, p=0.046) and negatively correlated with the FFR (r=–0.44, p=0.03). This indicates that ΔIMR increases with increasing CFIp and decreasing FFR (Figure 1). In the multiple regression analysis the overestimation of IMR (ΔIMR) was dependent on both FFR and CFIp (r=0.31, p=0.001).
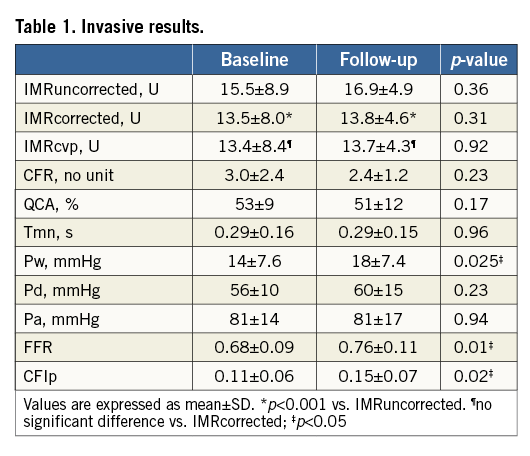
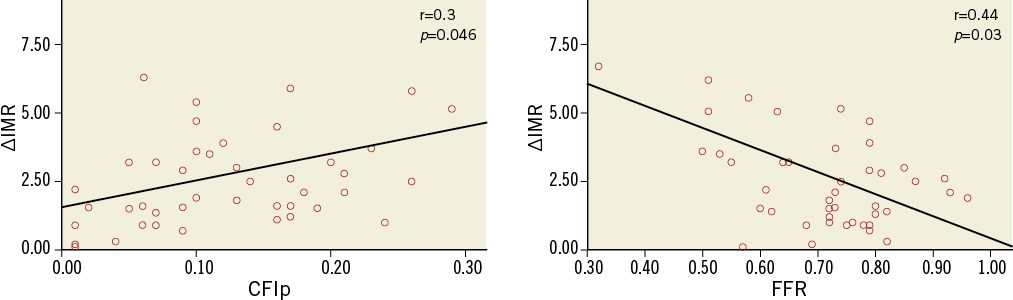
Figure 1. Changes of ΔIMR in relation to CFIp and FFR. The significant increase of ΔIMR by changes of the CFIp and FFR reveals the dependence of the index on the severity of myocardial stenosis and collateral blood flow, when the collateral blood flow is not taken into account. ΔIMR: IMRuncorrected-IMRcorrected; CFIp: pressure-derived collateral flow index; FFR: fractional flow reserve
IMR values did not differ between the groups at baseline or at follow-up (Figure 2). Interestingly, both IMRuncorrected and IMRcorrected did not differ between baseline and follow-up, suggesting that the index is reproducible during an extended period of time, such as seven weeks in the current trial.
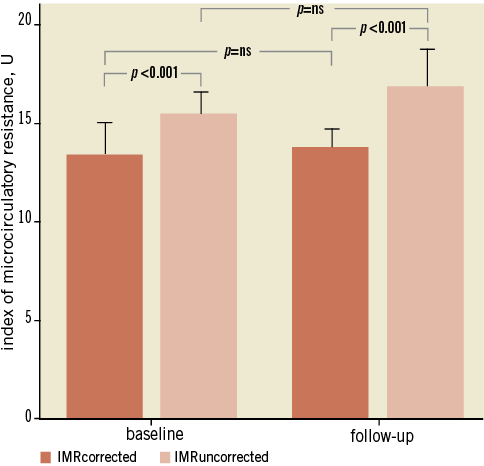
Figure 2. Changes of IMR from baseline to follow-up. IMRuncorrected was significantly higher than IMRcorrected at baseline and follow-up, demonstrating a constant overestimation of the index when the collateral blood flow was not taken into account. However, when comparing the IMR calculated upon a single equation, no difference was seen during the follow-up demonstrating a good reproducibility of the index.
In line with the IMR, the mean variability of Tmn under hyperaemia within a set of three measurements did not differ between the groups at any time point: 7.6±3.2% at baseline and 6.6±4.8% at follow-up (p=0.79).
The mean Pv was 4.2±2.7 mmHg at baseline and 5.6±3.1 mmHg during follow-up (p=ns). The IMRcvp calculated from equation 3 (corrected for Pv) did not differ from the IMRcorrected at any time point.
No statistical differences with regard to the IMR were found between patients who were treated with ECP and those who served as a control. In particular, at baseline, in the ECP group IMRcorrected was 14.0±8.8 U, and in the control group 10.1±4.5 U (p=0.09). In the ECP group the IMRuncorrected was 15.1±9.8 U, and in the control group 12.8±6.0 U (p=0.41). At follow-up, in the ECP group the IMRcorrected was 15.1±5.7 U, and in the control group 12.0±3.1 U (p=0.11). In the ECP group the IMRuncorrected was 16.7±5.2 U, and in the control group 15.7±4.8 U (p=0.72). For patients of both groups no change of the IMR (both corrected and uncorrected) was found from baseline to follow-up (p>0.1).
Discussion
In the current trial, different models for calculation of the IMR were evaluated in patients with chronic coronary artery stenoses. We demonstrated that an additional measurement of coronary occlusion pressure is necessary for reliable calculation of IMR. When IMR is calculated based on the Tmn and Pd only, an overestimation of the index occurs for FFR <0.8. This overestimation (ΔIMR) increases with increasing severity of the stenosis and is negatively correlated with FFR, as has recently also been shown in patients undergoing PCI10.
Despite a significant improvement in Pw from baseline (14±7.6 mmHg) to follow-up (18±7.4 mmHg), IMR (IMRuncorrected and IMRcorrected) remained unchanged. These data suggest that mild changes in the collateral status (indicated by a mean ΔCFIp=0.03±0.08) do not significantly influence the coronary microcirculation. In particular, IMRuncorrected, in spite of overestimating the resistance, remained unchanged between the two time points. This information could be useful in clinical trials investigating the effect of interventional or pharmaceutical therapies on microvascular resistance in patients with coronary artery disease. In this case, measurement of coronary occlusion pressure can be avoided in the follow-up study. However, for patients with severe haemodynamic stenoses, measurement of collateral blood flow at both baseline and follow-up may be essential, even for intra-individual comparison.
An important advantage of the invasive protocol used in this study, compared to previous trials, is the validation of IMR by measuring the Pw during both catheterisations and at the end of a 60 s balloon occlusion interval, as indicated for the correct assessment of collateral status19. Consequently, at each time point the actual values of Pw, Pd, and Pa were used for calculation of the IMRcorrected. Previous validations were based on a single measurement of Pw7,10 or on measurements of the collateral blood flow only during a 30 s coronary artery occlusion11. In these trials the single Pw value was then used to calculate the IMRcorrected, together with Pd and Pa values obtained from two different degrees of coronary stenoses or before and after a percutaneous coronary intervention. On the contrary, we measured at each time point all necessary parameters for calculating the IMR, including the collateral blood flow during a 60 s balloon inflation, as required for a maximal collateral recruitment19. This means that IMR was assessed each time by taking into account the actual collateral status for each degree of haemodynamic stenosis severity.
Another important aspect of the current trial is that we performed two invasive measurements in the absence of any coronary intervention between these time points. This minimises the chance of a change in microcirculatory resistance due to vasoconstriction or distal embolisation caused by a percutaneous intervention20,21. We demonstrated for the first time that IMR can be used for intra-individual comparisons in studies with follow-up assessment after a few weeks. Thus, IMR, when measured properly, is a reproducible index, even in the presence of significant epicardial stenoses. These results confirm previous data on the haemodynamic independence of IMR which were obtained in patients with angiographic stenosis <50% and FFR >0.7522. Finally, we present the first data that Pv can be excluded from the calculation of IMR. In future trials an additional central vein catheterisation for measurement of the central venous pressure will no longer be necessary, which may reduce the procedure time and possible complications due to puncture of the vein and placement of the catheter.
Study limitations
The major limitation of this trial is that the ECP therapy may have exerted effects on the status of the coronary microcirculation. There are no data about this issue in the literature. According to published data on the positive effect of ECP on peripheral endothelial function23, it can be hypothesised that ECP may improve microcirculatory function. However, a change in microcirculatory resistance due to improved endothelium-dependent vasodilatation is not mirrored by the CFR or IMR, both of them measured based on endothelium-independent hyperaemia induced by adenosine24. Therefore, the unchanged values of IMR and CFR in both the ECP and control groups at each time point indicate that ECP does not influence the coronary microcirculation. Another limiting factor is that repeated measurements of IMR may be subject to error due to different distances of the temperature sensor in the pressure wire from the tip of the guiding catheter. In the current trial, we always positioned the pressure wire in the most distal part of the coronary artery and recorded a view for the follow-up. It is suggested that small differences in the position of the pressure wire do not have a major impact on IMR2,22. As long as the hyperaemic Tmns are almost identical at baseline and follow-up, it is unlikely that the location of the pressure wire will influence the results of the trial. Furthermore, we have to mention that the current findings were made in patients with stable coronary heart disease who are expected to have a low Pv, as was found in our trial. In unstable patients with heart failure, the higher Pv may still be needed for the accurate measurement of IMR. However, some studies in patients with acute myocardial infarction showed that IMR, calculated by neglecting Pv, still has a prognostic value25. In addition, a possible influence of collateral status on the IMR in patients with good collateral arteries (CFIp>0.25) cannot be excluded. Lastly, these data are not conclusive about a possible overestimation of the IMR for stenosis with FFR >0.8, as such a population was not studied in this trial. However, since an overestimation of IMRuncorrected correlates with lower FFR according to published literature, we suppose that for non-significant stenoses (with higher values of FFR) the simple formula of IMR may be used.
Conclusions
This study demonstrates that the IMR can be reliably calculated only with simultaneous measurement of the CFlp. Otherwise, increasing collateral flow and stenosis severity cause overestimation of the index. However, even the uncorrected form of IMR is a reproducible index and can therefore be used for intra-individual comparisons in follow-up studies assessing the coronary microcirculation. The central venous pressure is no longer needed for accurate calculation of IMR in stable patients.
| Impact on daily practice The index of microcirculatory resistance (IMR) is constantly overestimated when collateral circulation is not taken into account. However, when the course of IMR over time has to be evaluated to assess the effects of interventional or pharmaceutical therapies on microcirculation, the index can be safely used for intra-individual comparisons without an additional measurement of collateral blood flow. Furthermore, in daily practice, it is no longer necessary to measure the central venous pressure when estimating IMR, as the index is independent of the venous pressure in stable patients. |
Conflict of interest statement
The authors have no conflicts of interest to declare.