Abstract
Background: Myocardial ischaemia with non-obstructive coronary arteries (INOCA) represents a challenging and frequent, but largely underdiagnosed, condition.
Aims: We aimed to investigate the feasibility and diagnostic value of angiography-derived coronary microcirculatory resistance in patients with INOCA syndrome.
Methods: This is an investigator-driven, prospective and blinded study. The diagnostic yield of angiography-derived index of coronary microcirculatory resistance (angio-IMR) was investigated against thermodilution-derived IMR (thermo-IMR) in patients with clinically indicated coronary angiography due to suspected myocardial ischaemia and angiographically normal or non-obstructive coronary arteries. The angio-IMR was derived from resting angiograms (contrast-flow angio-IMR [cAngio-IMR]) by an expert analyst blinded to the thermo-IMR. An independent, blinded, physiology core laboratory analysed the raw intracoronary physiology data and provided the final thermo-IMR values.
Results: A total of 104 patients (108 coronary vessels) were analysed after fulfilling predefined inclusion criteria. Most patients were female (67%). Obstructive epicardial disease was angiographically (percent diameter stenosis <50%) and physiologically (fractional flow reserve>0.80) ruled out in all cases. Median thermo-IMR and cAngio-IMR were 16.6 (12.7, 23.0) and 16.8 (12.8, 23.1) units, respectively (median difference −0.31, 95% confidence interval: −1.53 to 1.00; p=0.654). cAngio-IMR showed good correlation (Pearson coefficient 0.76; p<0.001), agreement (mean bias 0.4), discriminatory power (area under the curve from the receiver operator characteristics 0.865; p<0.001) and accuracy (85%), compared to thermo-IMR (≥25 U).
Conclusions: Evaluating coronary microcirculatory resistance in patients with INOCA syndrome using cAngio-IMR is feasible and accurate. By circumventing the need of coronary instrumentation and hyperaemic drugs, this method may facilitate the assessment of coronary microcirculatory resistance in patients with suspected INOCA. ClinicalTrials.gov: NCT04827498.
Introduction
Up to 70% of patients with clinically suspected myocardial ischaemia do not show epicardial stenoses in their coronary angiogram1. In this context, clinical guidelines recommend the assessment of other mechanisms of myocardial ischaemia including coronary microcirculatory dysfunction (CMD)2, mainly because it has been demonstrated that a tailored medical therapy may alleviate angina symptoms and improve quality of life3. Yet, the adoption of invasive coronary function testing (ICFT) into practice has been very slow, most likely due to the need of dedicated physiology wires, coronary instrumentation with low but not negligible iatrogenic risk, additional time, and the need of hyperaemic drugs like adenosine, all of which increase procedural costs and cause patient discomfort.
Over the last few years, we have witnessed the development of coronary angiography-derived physiology techniques which allow the estimation of coronary pressure and flow parameters without the need of physiology wires nor hyperaemic drugs4. Recently, it has been demonstrated that coronary revascularisation based on angiography-derived fractional flow reserve (FFR) (i.e., quantitative flow ratio [QFR]) is superior to that based on conventional angiography in terms of 1-year clinical outcomes5. By circumventing the reasons that cause low penetration of FFR6, it is assumed that these novel techniques may increase the use of physiology to guide coronary revascularisation decision-making in daily clinical practice.
Of note, the use of these novel angiography-derived methods can be extended to the interrogation of the microvascular compartment. Recent studies have demonstrated the feasibility and accuracy of these techniques, using either resting or hypaeremic angiograms to assess the coronary microcirculatory resistance in patients with ST-elevation myocardial infarction (STEMI) and chronic coronary syndromes with epicardial vessel stenoses789. In the present study, we aimed to assess the diagnostic value of angiography-derived index of microcirculatory resistance (angio-IMR) in patients with suspected myocardial ischaemia and non-obstructive coronary arteries (INOCA). We also aimed to determine which of the described approaches, using either hyperaemic or regular coronary angiograms, resulted in a better diagnostic yield.
Methods
Study design
This is an investigator-driven, prospective, observational, blinded study evaluating the diagnostic yield of angiography-derived index of coronary microcirculatory resistance compared to invasive thermodilution-derived IMR (thermo-IMR) as the reference standard. Angio-IMR was calculated by an expert analyst in a blinded fashion with respect to the invasive physiology data. An independent physiology core laboratory (Amsterdam UMC, the Netherlands) provided the final thermo-IMR values after a quality-check analysis blinded with respect to the angio-IMR. The study protocol was approved by the local ethics committee (21/289-E), and all patients gave written informed consent. The study was conducted following the principles of the Declaration of Helsinki and was registered at ClinicalTrials.gov: NCT04827498.
Study population
Consecutive patients with symptoms or non-invasive stress testing (NIT) suggesting myocardial ischaemia and angiographically normal coronary arteries or non-obstructive coronary stenoses, by both angiography (percent diameter stenosis [%DS] <50%) and FFR>0.80, were screened from July 2020 to December 2021, at Hospital Clinico San Carlos, Madrid, Spain. Coronary angiography and intracoronary physiology evaluation were indicated by the treating clinical cardiologist according to symptoms or NIT. Exclusion criteria were contraindication or intolerance to adenosine, angiography views not suitable for QFR analysis, non-optimal intracoronary pressure-flow traces as determined by the independent physiology core laboratory, presence of myocardial bridging, significant cardiac valvulopathies, non-normal left ventricle systolic function (left ventricular ejection fraction ≤55%), or cardiomyopathies.
Coronary angiography, QFR analysis and angio-IMR calculation
After routine intracoronary nitrates administration (200 mcg), standard angiography views were obtained following local practice with a Philips X-ray system at 15 frames per second during contrast medium injections performed with a power injector system (ACIST CVi Contrast Delivery System; ACIST). Operators were encouraged to i) perform QFR-aimed high quality angiograms (Supplementary Appendix 1, Supplementary Figure 1), ii) obtain the recommended views for QFR analysis according to the target coronary vessel (Supplementary Table 1), and iii) obtain an additional angiogram under adenosine-induced steady-state hyperaemia. DICOM files were transferred to the QFR console (QAngio XA 3D; Medis Medical Imaging Systems). An expert analyst performed the QFR calculation following standard guidelines10, and the contrast-flow angio-IMR (cAngio-IMR) was derived from resting angiograms as previously described9 (Supplementary Appendix 2), blinded with respect to the intracoronary physiology data. Additionally, the angio-IMR was also derived from angiograms obtained under adenosine-induced steady-state hyperaemia (adenosine-flow angio-IMR [aAngio-IMR]), as previously described8. Defined thresholds for abnormality were %DS ≥50%, QFR ≤0.80 and angio-IMR ≥25.
Intracoronary physiology evaluation
Details of the intracoronary physiology evaluation are given in Supplementary Appendix 3.
Data collection
All data were prospectively collected and registered in a dedicated online electronic case report form including patient demographics, vascular risk factors, clinical presentation and details of angiography and physiology procedures. The independent, blinded, physiology core laboratory (Amsterdam UMC, the Netherlands) received the anonymised raw physiology files extracted from the CoroFlow system (Coroventis), which contained intracoronary flow and pressure measurements, with the aim of performing a quality-check analysis and providing the final validated thermo-IMR values, including pressure drift correction, if necessary.
Statistical analysis
Continuous variables are shown as mean and standard deviation (±SD) or median with interquartile range (IQR 25, 75) according to the Shapiro-Wilk test, and were compared with the t-test, the Wilcoxon test, or the Mann-Whitney U test. Categorical data are presented as numbers with percentages and compared with Pearson’s chi-square or Fisher’s exact test, as appropriate. The diagnostic yield of cAngio-IMR was assessed at a per-vessel level using thermo-IMR as a reference standard; correlation, agreement, discriminatory power, and accuracy were evaluated using regression analysis and the Pearson correlation coefficient, Bland-Altman analysis, the area under the curve (AUC) from the receiver operating characteristics (ROC), and dichotomic agreement (cut-off ≥25), respectively. Sensitivity and specificity were obtained from the ROC analysis. Comparison of AUC between different angiography-derived methods was performed with the DeLong method. To assess interobserver reproducibility, a second analyst performed cAngio-IMR evaluation blinded to the results of the first analyst, but was unmasked to the proximal and distal landmarks of the target coronary vessel. Interobserver reproducibility for cAngio-IMR was investigated using correlation coefficient and dichotomic agreement. Intraobserver reproducibility was assessed by a repeat cAngio-IMR calculation 6 months after the first evaluation, also blinded to the initial results. MedCalc, version 19.3.1 (MedCalc) and SPSS statistics, version 25 (IBM) were used for statistical analysis. A p-value <0.05 was considered statistically significant.
Results
Baseline clinical characteristics
One hundred and twenty-seven patients with clinically indicated coronary angiography due to suspected INOCA were prospectively screened. After fulfilling clinical, functional coronary angiography, and physiology core lab inclusion criteria, 104 patients (108 coronary vessels) were included in the final analysis (Figure 1). The mean age was 61.2±10.9 years, most patients were female (67%), and traditional vascular risk factors were frequently reported (Table 1). The main patient symptom at index clinical presentation was chest pain (91%). A significant proportion of patients were medicated with antianginal drugs at baseline, including beta blockers (52%), calcium channel blockers (40%), or nitrates (23%).
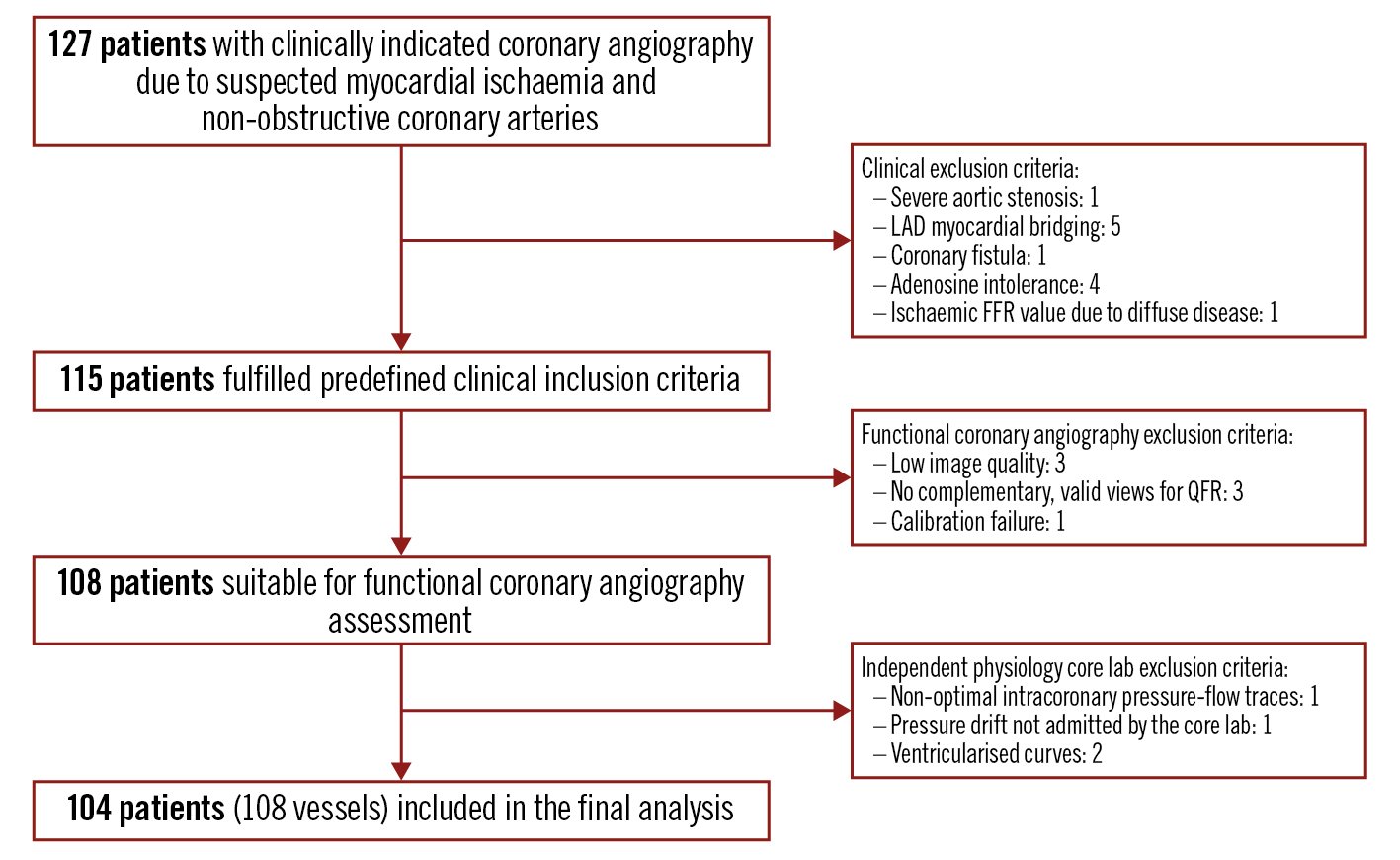
Figure 1. Study flow chart. FFR: fractional flow reserve; LAD: left anterior descending coronary artery; QFR: quantitative flow ratio
Table 1. Patient clinical characteristics
| N=104 | ||
|---|---|---|
| Demographics and vascular risk factors | Age, yrs | 61.2±10.9 |
| Female | 69 (67) | |
| Hypertension | 54 (52) | |
| Dyslipidaemia | 44 (42) | |
| Diabetes mellitus | 15 (14) | |
| Peripheral vascular disease | 2 (2) | |
| Active smoking | 12 (12) | |
| Body mass index, kg/m2 | 28 (25, 30) | |
| Previous AMI | 4 (4) | |
| Main symptom at index presentation |
Chest pain | 95 (91) |
| Dyspnoea | 3 (3) | |
| Both | 6 (6) | |
| Non-invasive myocardial ischaemia testing performed | 81 (78) | |
| Treadmill test | 65 (80) | |
| Positive | 47 (72) | |
| SPECT | 20 (25) | |
| Positive | 12 (60) | |
| Stress echocardiography | 13 (13) | |
| Positive | 3 (23) | |
| Ejection fraction, % | 58 (57, 60) | |
| Baseline medication | Aspirin | 61 (59) |
| Beta blocker | 54 (52) | |
| Calcium channel blocker | 42 (40) | |
| Nitrates | 24 (23) | |
| ACEI or ARB | 58 (56) | |
| Statin | 67 (64) | |
| Data are presented as mean±standard deviation, median (25th, 75th percentile), or counts (percentages). ACEI: angiotensin-converting enzyme inhibitor; AMI: acute myocardial infarction; ARB: angiotensin II receptor antagonist; SPECT: single photon emission computed tomography | ||
Physiology procedure characteristics
Coronary arteries were angiographically normal or presented any non-obstructive coronary stenosis in 64% and 36% of patients, respectively. The left anterior descending coronary artery (LAD) was the target vessel in most cases (91%). The mean length of the segmented vessel for QFR and angio-IMR analyses was 65±16 mm. Obstructive epicardial stenoses were ruled out in all cases by three-dimensional quantitative coronary analysis (%DS <50%), angiography-derived FFR (QFR>0.80) and intracoronary physiology evaluation (FFR>0.80) (Supplementary Figure 2). Impaired coronary microcirculatory dilation, determined by high thermo-IMR (≥25) or low CFR (<2.0), was identified in 22.2% and 28.7% of coronary vessels, respectively. Table 2 summarises the per-vessel procedure characteristics.
Table 2. Procedure characteristics
| N=108 coronary vessels | ||
|---|---|---|
| Target vessel | Left anterior descending | 98 (91) |
| Left circumflex | 6 (6) | |
| Right coronary artery | 4 (4) | |
| 3D-QCA | Length of segmented vessel, mm | 65±16 |
| Percent diameter stenosis, % | 25 (20, 33) | |
| Percent diameter stenosis ≥50% | 0 (0) | |
| Invasive coronary haemodynamics | Mean resting Pa, mmHg | 93 (86, 100) |
| Mean hyperaemic Pa, mmHg | 84±13 | |
| Pd/Pa | 0.94 (0.93, 0.96) | |
| FFR | 0.91±0.04 | |
| FFR ≤0.80 | 0 (0) | |
| Thermo-IMR | 16.6 (12.7, 23.0) | |
| Thermo-IMR ≥25 | 24 (22) | |
| Thermo-CFR | 2.8 (1.9, 3.9) | |
| Thermo-CFR <2.0 | 31 (29) | |
| Functional coronary angiography assessment | QFR | 0.96±0.04 |
| QFR ≤0.80 | 0 (0) | |
| cAngio-IMR | 16.8 (12.8, 23.1) | |
| cAngio-IMR ≥25 | 20 (19) | |
| Data are presented as mean±standard deviation, median (25th, 75th percentile), or counts (percentages). 3D-QCA: three-dimensional quantitative coronary analysis; cAngio-IMR: contrast-flow angiography-derived coronary microcirculatory resistance; FFR: fractional flow reserve; Pa: aortic pressure; Pd: intracoronary distal pressure; QFR: quantitative flow ratio; thermo-CFR: thermodilution-derived coronary flow reserve; thermo-IMR: thermodilution-derived index of coronary microcirculatory resistance | ||
Diagnostic yield of cAngio-IMR
The distribution of cAngio-IMR and thermo-IMR values within the study population was similar, with no significant difference found in the median values for both techniques (16.8 [12.8, 23.1] vs 16.6 [12.7, 23.0], respectively; median difference â0.31, 95% confidence interval [CI]: â1.53 to 1.00; p=0.654) (Figure 2). The regression analysis identified a linear positive correlation between thermo-IMR and cAngio-IMR, with a good association as per the Pearson correlation coefficient (r=0.76; p<0.001) (Figure 3A). A Bland-Altman plot revealed an overall low systematic bias (mean difference between the 2 techniques 0.4), although with wide limits of agreement mirroring individual significant differences (Figure 3B). Yet, cAngio-IMR had a high accuracy in detecting increased coronary microcirculatory resistance, correctly classifying 85% of cases according to thermo-IMR, using the threshold ≥25 units (Figure 3C). The ROC analysis revealed a high AUC (0.865; p<0.001), confirming a good discriminatory power for cAngio-IMR using thermo-IMR ≥25 as reference (Figure 3D); sensitivity and specificity were 0.83 (95% CI: 0.63 to 0.95) and 0.82 (95% CI: 0.72 to 0.90), respectively. Interobserver reproducibility for cAngio-IMR was good, as depicted by the correlation coefficient between paired measurements, 0.88 (95% CI: 0.83 to 0.91; p<0.0001) and classification agreement (low vs high values) 81% (p<0.01). Intraobserver reproducibility was high: correlation coefficient 0.96 (95% CI: 0.94 to 0.97; p<0.0001), classification agreement 96% (p<0.0001).
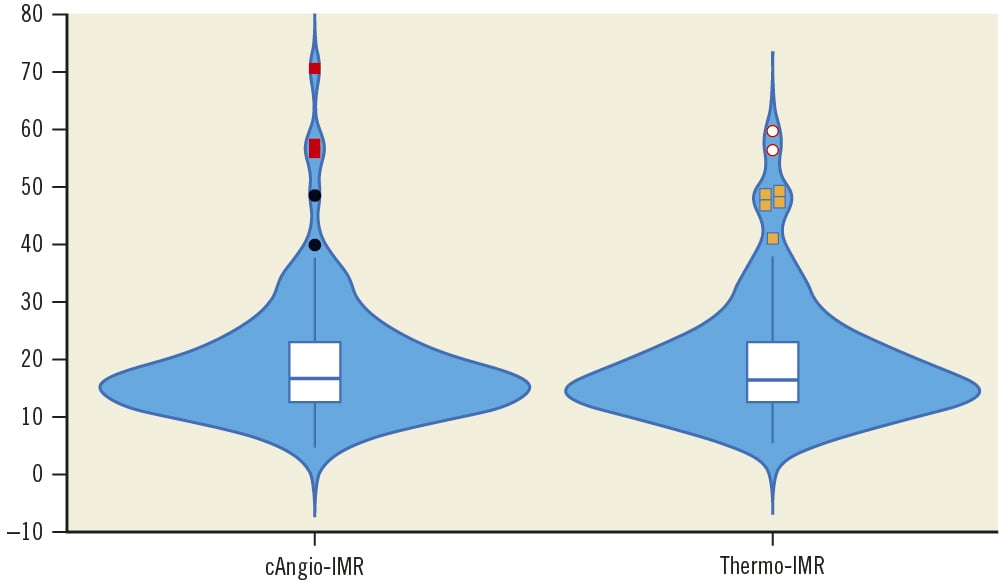
Figure 2. Distribution of cAngio-IMR and thermo-IMR values across the study population. Violin plots show the density trace of values for cAngio-IMR and thermo-IMR. Inside each violin plot is also shown the corresponding box and whisker plot with median, 25th and 75th percentile, and outliers for both methods. cAngio-IMR: contrast-flow angiography-derived index of coronary microcirculatory resistance; thermo-IMR: thermodilution-derived index of coronary microcirculatory resistance
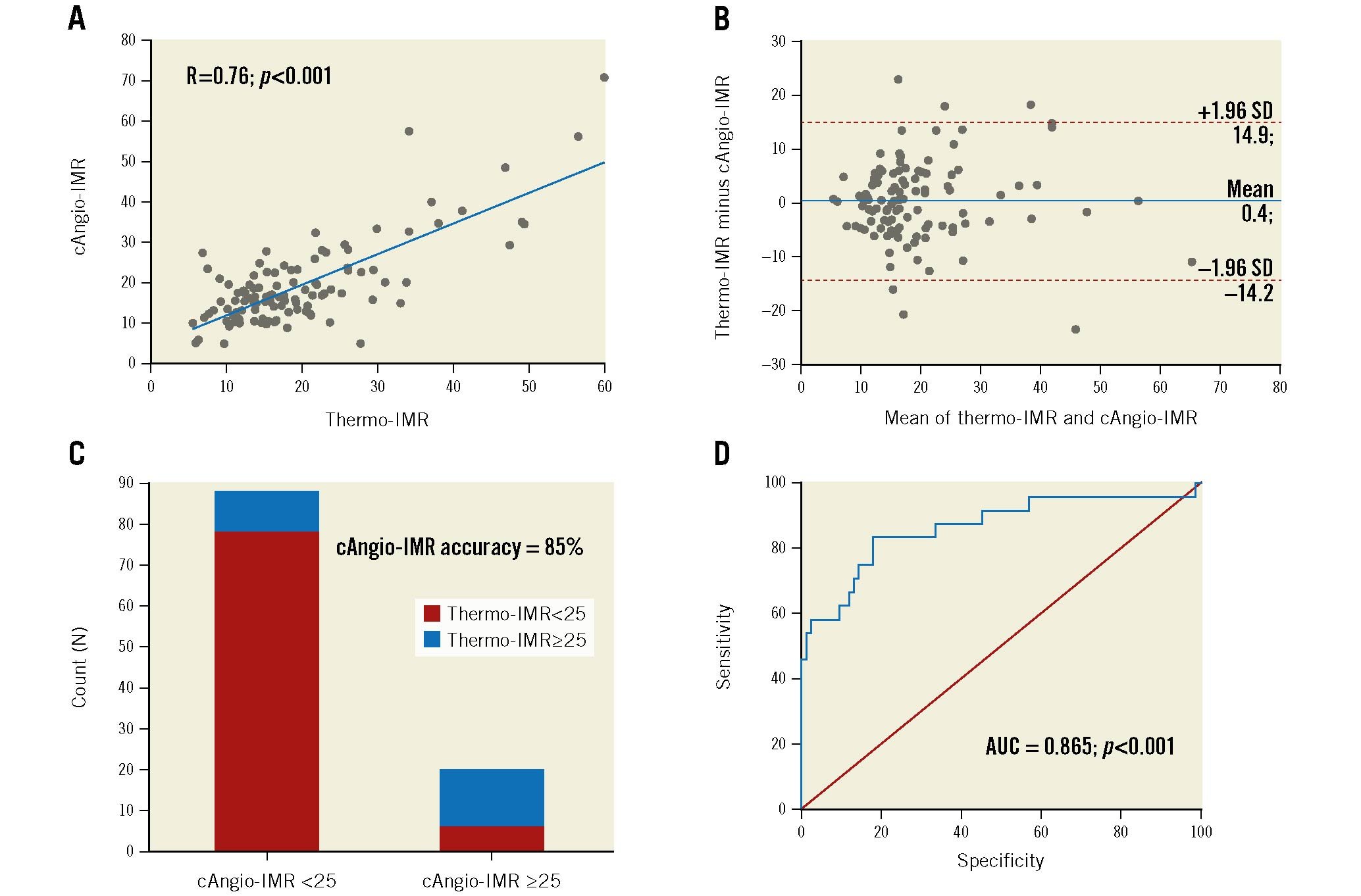
Figure 3. Diagnostic yield of cAngio-IMR. A) Scatterplot with regression line displaying the association between cAngio-IMR and thermo-IMR values. B) Bland-Altman analysis for agreement assessment between cAngio-IMR and thermo-IMR. C) Dichotomic concordance between both methods using the cut-off 25. D) Discriminatory power of cAngio-IMR for detecting high thermo-IMR (≥25) according to the receiver operator characteristic analysis. cAngio-IMR: contrast-flow angiography-derived index of coronary microcirculatory resistance; AUC: area under the curve; R: Pearson correlation coefficient; SD: standard deviation; thermo-IMR: thermodilution-derived index of coronary microcirculatory resistance
Comparison of different angiography-derived methods for estimating coronary microvascular resistance
Hyperaemic angiographies were suitable for angiography-derived microcirculatory analysis in 89% of patients. Among these, aAngio-IMR provided a significantly lower diagnostic yield compared to cAngio-IMR (AUC 0.65 [95% CI: 0.55 to 0.74] vs 0.85 [95% CI: 0.77 to 0.92]; p=0.0007) (Figure 4). Additionally, the difference between contrast-flow QFR (cQFR) and fixed-flow QFR (fQFR) (i.e., cQFR minus fQFR), another proposed surrogate for the assessment of coronary microvascular resistance11, was also inferior to cAngio-IMR in identifying increased coronary microcirculatory resistance as per thermo-IMR ≥25 (AUC 0.71 [95% CI: 0.61 to 0.80] vs 0.85 [95% CI: 0.77 to 0.92]; p=0.0337) (Figure 4).
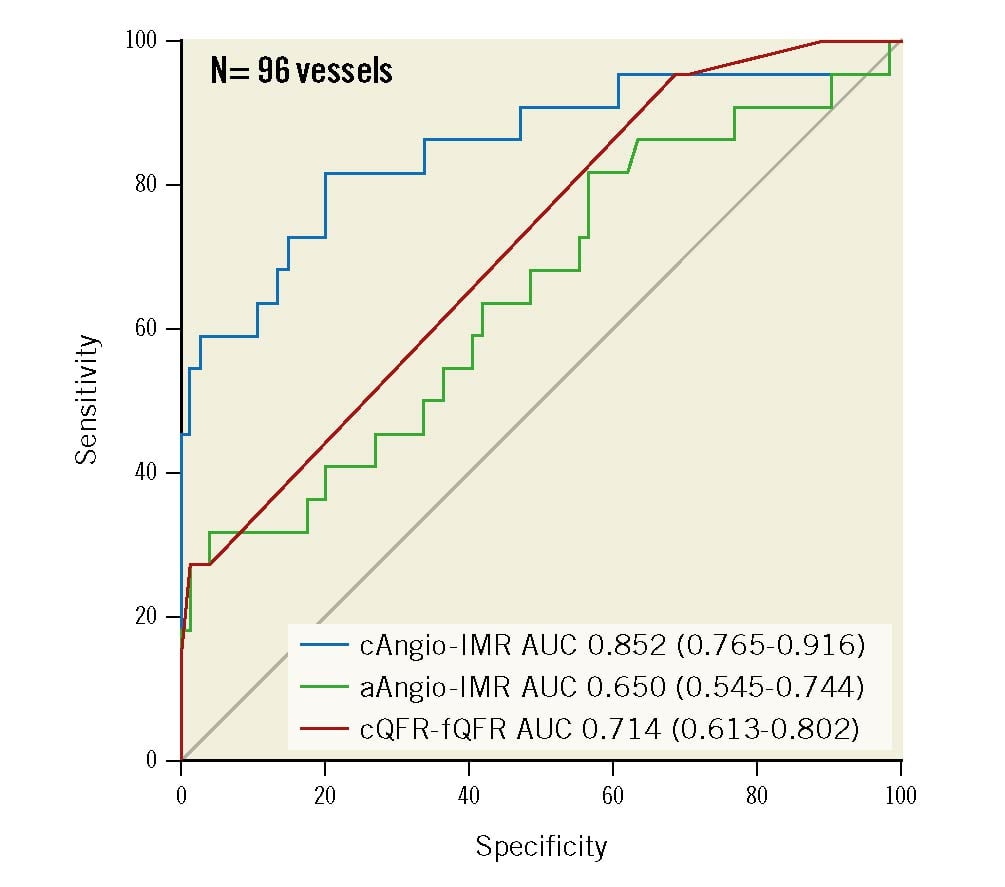
Figure 4. Comparison of different angiography-derived methods for estimating coronary microcirculatory resistance. The figure shows the comparison between cAngio-IMR, aAngio-IMR and cQFR minus fQFR for identifying increased coronary microcirculatory resistance according to thermo-IMR ≥25. aAngio-IMR: adenosine-flow angiography-derived index of coronary microcirculatory resistance; AUC: area under the curve; cAngio-IMR: contrast-flow angiography-derived index of coronary microcirculatory resistance; cQFR: contrast-flow QFR; fQFR: fixed-flow QFR; QFR: quantitative flow ratio
Association between coronary microcirculatory resistance and non-invasive myocardial ischaemic testing
NIT was available in 81 patients (78%), for whom a treadmill stress test was the predominant test (80%). Overall, a positive NIT suggesting myocardial ischaemia was obtained in 57 patients (70%). No significant association was found between NIT and increased coronary microvascular resistance either by thermo-IMR or cAngio-IMR: median thermo-IMR 15 (12, 24) in patients with negative NIT vs 18 (14, 23) in patients with positive NIT (median difference 1.26, 95% CI: â2.76 to 5.07; p=0.5281); median cAngio-IMR 17 (12, 23) in patients with negative NIT vs 17 (13, 23) in patients with positive NIT (median difference 0.09, 95% CI: â4.21 to 4.24; p=0.9588) (Figure 5A). Vice versa, the frequency of positive NIT was similar among patients with low or high thermo-IMR (71% vs 67%; p=0.6982) and among patients with low or high cAngio-IMR (70% vs 71%; p=0.9825) (Figure 5B). Similar results were obtained for coronary flow reserve (CFR): 2.9 (1.9, 3.6) vs 2.7 (1.9, 3.8) in patients with negative and positive NIT, respectively (median difference 0.00, 95% CI: â0.60 to 0.70; p=0.9587).
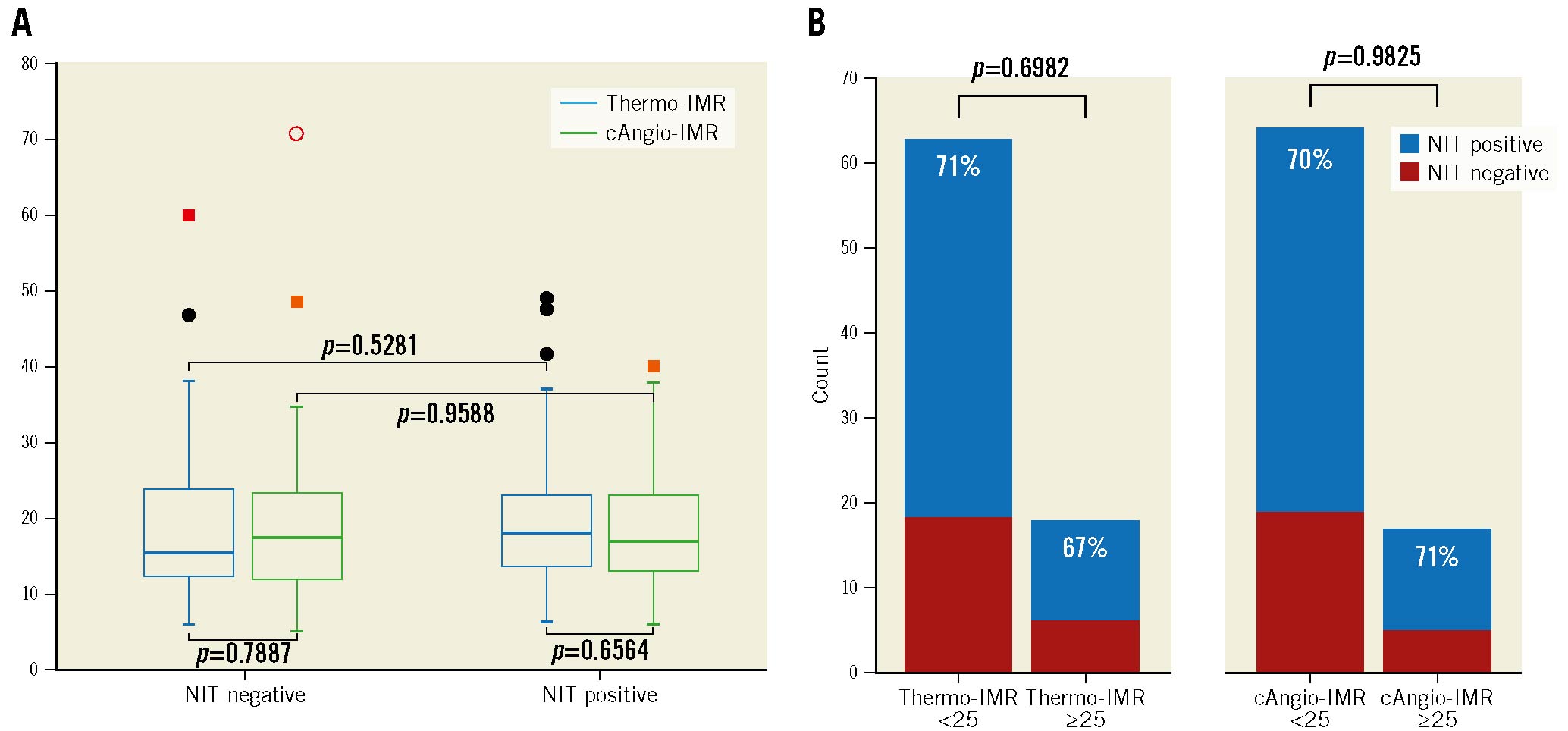
Figure 5. Association between NIT and coronary microcirculatory resistance. A) Box and whisker plots comparing the distribution of thermo-IMR and cAngio-IMR between patients with negative and positive NIT. B) Bars depicting the frequency of positive and negative NIT among patients with low or high microvascular resistance as assessed by thermo-IMR and cAngio-IMR. cAngio-IMR: contrast-flow angiography-derived index of coronary microcirculatory resistance; NIT: non-invasive stress testing; thermo-IMR: thermodilution-derived index of coronary microcirculatory resistance.
Discussion
The results of our study demonstrate the feasibility and value of contrast-flow angiography-derived index of coronary microcirculatory resistance (cAngio-IMR) in the diagnostic work-up of patients with suspected INOCA, providing accurate measurements of microcirculatory resistance as determined with wire-based IMR (Central illustration). By simplifying the physiological assessment of the coronary microcirculatory resistance, this method may contribute to the adoption of guideline recommendations for the diagnosis and management of patients with microvascular angina.
Over the last years, the role of coronary microcirculation as a key component of myocardial ischaemia in non-obstructive coronary artery disesase (CAD) has been increasingly recognised12. The CorMicA trial found that in INOCA patients a tailored medical therapy according to ICFT results in better quality of life compared to empirical treatment3. Other studies have already reported a long-term worse prognosis in patients with non-obstructive CAD but persistent angina13, as well as in patients with impaired microcirculatory vasodilation (i.e., low CFR or high microvascular resistance)14. Together, the evidence gathered over the last years for a physiology wire-based CFR and/or microcirculatory resistance assessment in patients with persistent symptoms despite non-obstructive CAD has reached a class II, level of evidence A recommendation in the latest European clinical guidelines on chronic coronary syndromes2. Unfortunately, the adoption of coronary microcirculatory assessment with ICFT into real practice is hampered by similar reasons to those causing low penetration of FFR15.
Recently, several studies have demonstrated the feasibility and accuracy of angiography-derived physiology techniques to assess coronary microcirculatory resistance in different clinical subsets. In STEMI patients, De Maria et al investigated the diagnostic accuracy of QFR-derived angio-IMR for estimating thermo-IMR subtended to culprit vessels, measured immediately after successful primary percutaneous coronary intervention (PCI)16. The authors found a good correlation between angio-IMR and thermo-IMR and a significant association between angio-IMR and microvascular obstruction as detected by cardiac magnetic resonance. Despite its pioneering nature, the study was limited by a low sample size and its applicability by the need of inducing hyperaemia with adenosine in such a particular clinical scenario (i.e., STEMI). In another effort different from De Maria et al, Choi and colleagues investigated the accuracy and prognostic value of resting angiogram-derived angio-IMR computed from pressure-flow dynamics-derived FFR (caFFR) in STEMI7. The authors found a good correlation between angio-IMR and thermo-IMR subtended to infarcted-related arteries after successful primary PCI, and an angio-IMR >40 was found to be an independent predictor of cardiac death or readmission for heart failure over 10 years of follow-up.
Our group has already investigated the feasibility and accuracy of angio-IMR, derived from conventional, resting coronary angiographies (i.e., cAngio-IMR), for estimating wire-based IMR9. We found a good correlation and accuracy of cAngio-IMR in patients with stable intermediate coronary stenosis9. Now we present the diagnostic performance of this novel method in patients with suspected INOCA. In this study, cAngio-IMR had a good correlation and discriminatory power in detecting increased coronary microcirculatory resistance. These results open the possibility of providing important information for clinicians when investigating chest pain in patients without obstructive epicardial coronary stenoses or with apparently normal coronary arteries. According to the European Association of Percutaneous Cardiovascular Interventions (EAPCI) expert consensus on INOCA management12, the identification of structural CMD endotypes should be followed by focusing treatment on diminishing myocardial oxygen consumption, along with treatment of existing cardiovascular risk factors that may account for structural changes in the microvasculature.
Of note, in this population we found a relatively low prevalence of structural CMD endotypes: 22% of patients had a high microvascular resistance, 29% had a low CFR, and 10% had a combination of both mechanisms. Conversely, most patients with NIT performed prior to invasive coronary angiography had a positive result (77%). The significant difference between NIT and microcirculatory resistance results may be read in several ways; i) the heterogeneous NIT methods used for assessing myocardial ischaemia, mainly a treadmill stress test, may explain such a wide discordance, although this mirrors real clinical practice and clinical cardiologist preferences when facing assessment of chest pain (at least in our centre); ii) it is well known that women are more likely to have false-positive exercise test results even in presence of normal coronary angiography17; and iii) the fact that neither thermo-IMR nor angio-IMR provide information on the presence of other mechanisms of myocardial ischaemia, including vasospastic angina. In any case, our study reveals a low power of NIT, mainly treadmill stress tests, to determine the presence of increased coronary microcirculatory resistance. This contrasts with the good discriminatory power of the novel method cAngio-IMR for the detection of high microvascular resistance suggesting microvascular remodelling in patients with suspected INOCA.
Finally, we found that cAngio-IMR has a better diagnostic performance than aAngio-IMR in INOCA patients. These results are partially opposed to another recently published study8. Some explanations for these findings could rely on differences in the methodologies used for deriving angio-IMR (their non-hyperaemic angio-IMR derivation does not account for simulation of mean aortic pressure during hyperaemia), technical differences when performing coronary angiographies (i.e., manual injection of dye vs using a power injection system), and the clinical subset (INOCA vs other subsets). Furthermore, hyperaemic angiographies are technically more challenging because they require some ability to achieve an optimal coronary opacification under hyperaemic conditions (i.e., tachycardia, difficult breathing, inotropism, etc.). It is also important to highlight that pioneering studies of QFR have already demonstrated no difference in the diagnostic performance between resting and hyperaemic coronary angiographies18. The better diagnostic yield of cAngio-IMR observed in the present study could certainly facilitate a wide adoption of coronary microcirculatory resistance assessment in INOCA patients by avoiding not only coronary instrumentation with physiology wires but also the need of artificial hyperaemia.
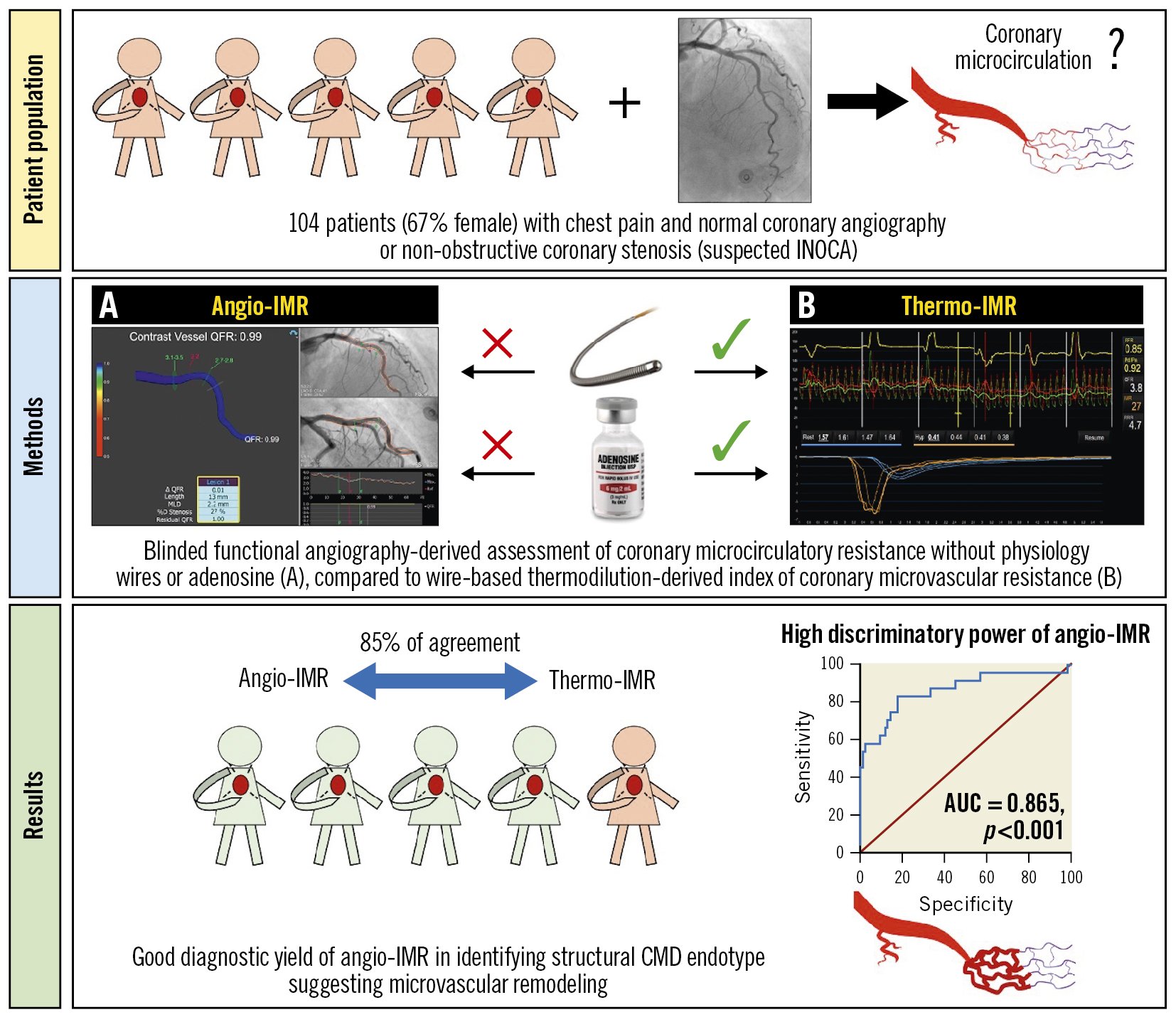
Central illustration. Diagnostic yield of angiography-derived assessment of coronary microcirculatory resistance in patients with suspected myocardial ischaemia and non-obstructive coronary arteries (INOCA): study design and summary results. angio-IMR: angiography-derived index of coronary microcirculatory resistance; AUC: area under the curve; CMD: coronary microvascular dysfunction; thermo-IMR: thermodilution-derived index of coronary microvascular resistance
Limitations
This study is not powered to evaluate the association between angio-IMR and clinical outcomes. As a single-centre study with a relatively low sample size, future larger and multicentre studies are warranted to assess the diagnostic yield of angio-IMR in this specific clinical subset. Most studies were performed in the LAD, which mirrors the usual preferred target vessel for physiology evaluation in INOCA patients, due to its large myocardial mass and coronary dominance. The accuracy of angio-IMR was evaluated in angiograms obtained with a power injection system according to local clinical practice; the effect of manual contrast injections is unknown. Recommendations for the acquisition of optimal image quality are described in Supplementary Appendix 1B. Finally, the use of coronary angiography-derived physiology techniques to explore other domains of microcirculatory function like coronary flow reserve and vasospasm has not been explored in the present study.
Conclusions
The evaluation of coronary microcirculatory resistance in patients with INOCA syndrome using cAngio-IMR from coronary angiography is feasible and accurate. By circumventing the need for coronary instrumentation and hyperaemic drugs, cAngio-IMR may facilitate the assessment of coronary microcirculatory resistance in patients with suspected INOCA.
Impact on daily practice
In patients with suspected myocardial ischaemia and non-obstructive coronary arteries (INOCA), the identification of increased coronary microcirculatory resistance as a cause of coronary microcirculatory dysfunction with angio-IMR is feasible and accurate. By circumventing the need of coronary instrumentation with physiology wires and hyperaemic drugs, this method may help in assessing the coronary microcirculation in INOCA patients.
Funding
This is an investigator-driven study and financial support from third parties was not requested.
Conflict of interest statement
H. Mejía-Renteríahas received consultancy fees from Medis Medical Imaging; and speaker fees from Philips and Abbott. T. van de Hoef has received institutional research grants from Philips and Abbott; and has received consultancy fees from Philips. A. Travieso has received an unconditional educational grant from Philips. N. Gonzalo has received consultancy and speaker fees from Abbott, Boston Scientific, and Philips. J. Escaned has received consultancy and speaker fees from Abbott and Philips; and speaker fees from Medis Medical Imaging. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.