Abstract
Background: Cardiac stress tests remain the cornerstone for evaluating patients suspected of having obstructive coronary artery disease (CAD). Coronary microvascular dysfunction (CMD) can lead to abnormal non-invasive tests.
Aims: We sought to assess the diagnostic performance of exercise stress tests with indexes of epicardial and microvascular resistance as reference.
Methods: This was a prospective, single-arm, multicentre study of patients with an intermediate pretest probability of CAD and positive exercise stress tests who were referred for invasive angiography. Patients underwent an invasive diagnostic procedure (IDP) with measurement of fractional flow reserve (FFR) and index of microvascular resistance (IMR) in at least one coronary vessel. Obstructive CAD was defined as diameter stenosis (DS) >50% by quantitative coronary angiography (QCA). The objective was to determine the false discovery rate (FDR) of cardiac exercise stress tests with both FFR and IMR as references.
Results: One hundred and seven patients (137 vessels) were studied. The mean age was 62.1±8.7, and 27.1% were female. The mean diameter stenosis was 37.2±27.5%, FFR was 0.84±0.10, coronary flow reserve was 2.74±2.07, and IMR 20.3±11.9. Obstructive CAD was present in 39.3%, whereas CMD was detected in 20.6%. The FDR was 60.7% and 62.6% with QCA and FFR as references (p-value=0.803). The combination of FFR and IMR as clinical reference reduced the FDR by 25% compared to QCA (45.8% vs 60.7%; p-value=0.006).
Conclusions: In patients with evidence of ischaemia, an invasive functional assessment accounting for the epicardial and microvascular compartments led to an improvement in the diagnostic performance of exercise tests, driven by a significant FDR reduction.
Introduction
Cardiac stress testing remains the cornerstone for evaluating patients suspected of having coronary artery disease (CAD)1. Guidelines recommend stress testing for patients with an intermediate probability of CAD12. Nevertheless, the performance of this approach is limited by the moderate accuracy of non-invasive functional tests in detecting obstructive CAD3. This results in a high proportion of patients with stress tests suggestive of myocardial ischaemia without obstructive lesions on conventional angiography. In clinical practice, these are considered false-positive stress tests4.
Invasive coronary angiography is limited in assessing the presence of CAD. Diffuse coronary atherosclerosis may present with near-normal angiograms5. Diffuse coronary atherosclerosis without focal stenosis at angiography causes a graded, continuous pressure fall that contributes to myocardial ischaemia6. In addition, high resistance at the level of the coronary microcirculation can also lead to ischaemia, and coronary microvascular dysfunction (CMD) is recognised as a cause of positive stress tests indicating ischaemia without obstructive epicardial coronary artery disease (INOCA)78.
Non-invasive stress tests have been validated with invasive coronary angiography as a reference that was considered the gold standard for stenosis assessment for many years3. Coronary physiology-derived indexes such as fractional flow reserve (FFR) are superior to angiography for clinical decision-making about revascularisation9. Moreover, the assessment of the index of microvascular resistance (IMR) in patients with INOCA has been shown to enhance patients’ management, resulting in improved quality of life10. The proportion of patients considered to have false-positive stress test results with abnormalities in the epicardial or microvascular compartments that are only detectable by an invasive coronary physiology diagnostic procedure (IDP) remains unknown. The present study aimed at determining the diagnostic accuracy of cardiac stress tests using both FFR and IMR as clinical references.
Methods
Study design
The UZ Clear (Redefining the Diagnostic Performance of Non-invasive Tests for the Detection of Coronary Artery Disease) study was an investigator-initiated, single-arm, multicentre, prospective study of patients presenting with chest pain with an intermediate probability of CAD. Intermediate pretest probability of CAD was defined based on the European Society of Cardiology Guidelines as a score between 15% and 85% based on age, sex, and the nature of symptoms2. All patients had a positive exercise stress test and were referred for an invasive evaluation. Patients underwent a study protocol with an IDP consisting of measurements of FFR and IMR in at least one coronary vessel irrespective of the presence or severity of epicardial stenosis. Obstructive CAD was defined as diameter stenosis (DS) >50% by quantitative coronary angiography (QCA). Exclusion criteria were acute coronary syndrome, known coronary artery disease, previous myocardial infarction, previous revascularisation, and abnormal baseline electrocardiogram (ECG). A complete list of inclusion and exclusion criteria is shown in Supplementary Table 1. All data were centrally collected and analysed by the core laboratory (CoreAalst BV, Aalst, Belgium). The study protocol was approved by the investigational review board or ethics committee at each participating centre. All patients signed informed consent before the study procedures. The study was sponsored by Universitair Ziekenhuis Brussel (Brussels, Belgium) with unrestricted grants from Abbott.
The primary objective was to determine the false discovery rate (FDR) of exercise stress tests using an IDP with indexes of epicardial (FFR) and microvascular resistance as clinical references. The secondary objective was to assess the impact of an IDP accounting for the presence of CMD on the accuracy of exercise stress tests.
Exercise stress tests
Exercise tests were performed according to local protocol using a bicycle ergometer. In brief, patients were at rest for 2 minutes on the bicycle before starting the ramp protocol at 25 watts, with increases of 10-25 watts every minute. The recovery phase lasted for 2 minutes while pedalling without resistance and another 2 minutes at rest. ECG, blood pressure and heart rate were continuously recorded. Assessment of eligibility based on ischaemia severity was made locally, but an independent core laboratory also read the stress studies. A positive exercise stress test was defined as the development of either a downslope or horizontal ST depression ≥1 mm in at least two adjacent leads or the development of angina or arrhythmias.
Invasive diagnostic procedure
After administering intracoronary nitroglycerine, coronary angiograms were acquired in two projections separated by at least 30 degrees. Three-dimensional (3D) QCA was performed for all cases using CAAS Workstation 8.2 (Pie Medical Imaging). Invasive coronary angiography was performed following local protocols in the participating hospitals, and coronary function tests were performed as an adjunctive procedure. The IDP was performed in at least one coronary artery with a recommendation to perform multivessel evaluation when feasible. The left anterior descending coronary artery was the preferred target vessel; however, if technical factors precluded guidewire-based assessment of this artery (e.g., a tortuous anatomy), the left circumflex or right coronary artery were selected. In the case of multiple measurements per patient, either the lowest FFR or highest IMR was used for analysis. A coronary wire with a pressure and temperature sensor (PressureWire X; Abbott Vascular) was advanced to the mid-distal segment of the coronary artery. The bolus thermodilution technique with three x 3 cc saline injections at rest and hyperaemia was used for the assessment of coronary flow reserve (CFR; abnormal <2.0) and IMR (abnormal ≥25), and the lowest ratio of distal to aortic pressure was used to calculate FFR (abnormal ≤0.80) during intravenous infusion of adenosine (140 mg/kg/min)11. In patients with significant lesions, the revascularisation mode and techniques were left to the operator’s discretion. Cases with chronic total occlusions or subocclusive lesions were considered as having an abnormal FFR (≤0.80). Pressure and temperature tracings were examined by the core laboratory to evaluate quality, curve artefacts, and hyperaemia stability. Pressure and temperature tracings were analysed using CoroFlow 3.5 (Coroventis).
Statistical analysis
Continuous variables with normal distribution are presented as mean±SD and non-normally distributed variables as median (interquartile range). Categorical variables are presented as counts and percentages. UZ Clear was powered to detect a reduction of 25% in the FDR of cardiac exercise tests utilising FFR and IMR as clinical references, as compared to conventional QCA. Using McNemar's test with a type I error (alpha) of 5% and type II error (power) of 90%, it was determined that 114 patients were required. FDR was defined as false-positive exercise tests divided by all positive tests. False-positive exercise tests were defined using four clinical references, i.e., a DS >50%, an FFR ≤0.80, an IMR ≥25, and a combination of FFR and IMR. In the case of multiple physiological measurements, the lowest FFR or highest IMR were used for analysis. False discovery rates were compared using McNemar’s test. A p-value <0.05 was considered significant. All analyses were performed using R statistical software (R Foundation for Statistical Computing).
Results
From December 2019 to November 2021, 339 patients with a positive exercise stress test were screened for eligibility in three centres in two countries. Figure 1 shows the flowchart of the study. Recruitment was stopped after inclusion slowed due to the COVID-19 pandemic. One hundred and seven patients were included in the final analysis.
Baseline patient characteristics are shown in Table 1. The mean age was 62.1±8.7, and 27.1% were female. There was a moderate prevalence of cardiovascular risk factors in keeping with the mean pretest probability of CAD (23.7±12.7%). Antianginal therapies consisted of beta blockers in 37.4% of patients and calcium-channel blockers in 17.8% (Table 1). The core lab confirmed 91.6% of the exercise test results to be suggestive of ischaemia. The mean exercise time was 7.9±2.9 min, maximum load 147±51 watts, and mean ST depression 1.6±0.6 mm (Table 2). Details of additional testing are provided in the Supplementary Table 2.
Procedural characteristics are shown in Table 3. The most common interrogated vessel was the left anterior descending artery (LAD; 68.6%); 24% of the patients had multivessel interrogation. Overall, 60.7% of patients presented with non-obstructive coronary arteries; the mean DS was 37.2±27.5%. Among all patients, the mean FFR was 0.84±0.10, CFR 2.74±2.07, and IMR 20.3±11.9. The relationship between FFR, IMR, and QCA is shown in Figure 2 and Supplementary Table 3-Supplementary Table 5. There were no adverse events related to the IDP.
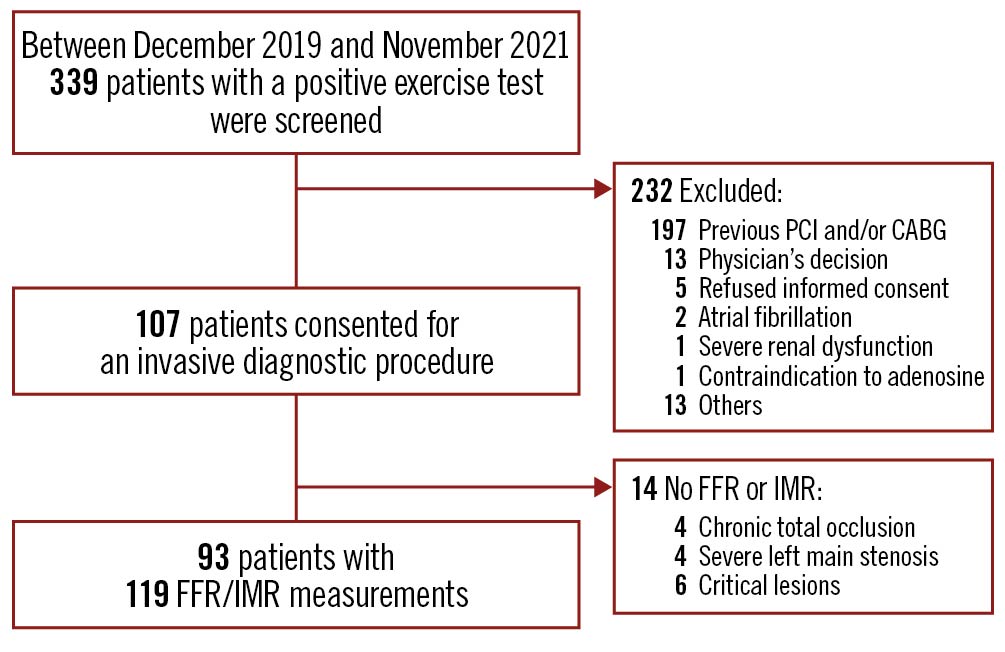
Figure 1. Study flowchart. In 14 patients, invasive physiology measurements were not performed because of either a total occlusion or sub-occlusive lesion. CABG: coronary artery bypass graft surgery; FFR: fractional flow reserve; IMR: index of microvascular resistance; PCI: percutaneous coronary intervention
Table 1. Patient characteristics.
| Variables | Overall |
|---|---|
| Number of patients | 107 |
| Age, yrs | 62.1±8.7 |
| Gender, male | 78 (72.9) |
| Weight, kg | 79.8±14.5 |
| Height, cm | 172.5±10.0 |
| BMI, kg/m2 | 26.9±4.97 |
| Dyslipidaemia | 72 (67.3) |
| Hypertension | 59 (55.1) |
| Diabetes mellitus | 17 (15.9) |
| Current smoker | 8 (7.6) |
| Peripheral artery disease | 5 (4.7) |
| Clinical presentation | |
| Typical chest pain | 32 (29.9) |
| Atypical chest pain | 39 (36.4) |
| Non-angina symptoms | 20 (18.7) |
| Dyspnoea | 16 (15.0) |
| CCS class* | |
| Stable angina CCS I | 11 (11.2) |
| Stable angina CCS II | 23 (23.5) |
| Stable angina CCS III | 2 (2.0) |
| Stable angina CCS IV | 4 (4.1) |
| Pretest probability of CAD, % | 23.7±12.7 |
| Creatinine, mg/dl | 0.91±0.18 |
| Creatinine clearance | 82.4±23.9 |
| Left ventricular ejection fraction, % | 59.1±5.73 |
| Medication | |
| Angiotensin-converting enzyme inhibitor | 38 (35.5) |
| Beta blocker | 40 (37.4) |
| Nitrates | 5 (4.7) |
| Calcium-channel blocker | 19 (17.8) |
| Digoxin | 0 (0) |
| Statins | 60 (56.1) |
| Diuretics | 16 (15.0) |
| Aspirin | 53 (49.5) |
| P2Y12 inhibitors | 10 (9.3) |
| Values presented as mean±SD or n (%). *Only available for 40/107 patients. BMI: body mass index; CAD: coronary artery disease; CCS: Canadian Cardiovascular Society | |
Table 2. Exercise test characteristics
| Variables | Overall |
|---|---|
| Exercise stress test | 107 (100) |
| Exercise stress test results by core laboratory | |
| Positive | 98 (91.6) |
| Negative | 9 (8.4) |
| Exercise time, seconds | 479±172 |
| Time to ST-segment deviation, seconds | 351±153 |
| ST-segment deviation, mm | 1.61±0.67 |
| Anginal symptoms during stress test | |
| No angina | 97 (90.7) |
| Non-limiting angina | 10 (9.3) |
| Dyspnoea | 7 (6.5) |
| Supraventricular contraction | 2 (1.9) |
| Ventricular arrhythmia | 0 (0) |
| Values presented as mean±SD or n (%). | |
Table 3. Procedural characteristics.
| Variables | Overall |
|---|---|
| Vessels interrogated | 137 |
| LAD | 94 (68.6) |
| LCx | 25 (18.2) |
| RCA | 17 (12.4) |
| LMT | 1 (0.7) |
| Vessels assessed FFR and IMR | 119 |
| One vessel | 97 (81.5) |
| Two vessels | 18 (15.1) |
| Three vessels | 4 (3.4) |
| Diameter stenosis, % | 37.2±27.5 |
| Patients with diameter stenosis >50% | 42 (39.3) |
| FFR | 0.84±0.10 |
| Patients with FFR ≤0.8 | 40 (37.4) |
| CFR | 2.74±2.07 |
| Tmn at rest, seconds | 0.53±0.20 |
| Patients with CFR ≤2.0 | 35 (43.2) |
| IMR | 20.3±11.9 |
| Tmn at hyperaemia, seconds | 0.30±0.17 |
| Patients with IMR ≥25.0 | 22 (20.6) |
| Patients with FFR ≤0.8 or IMR ≥25.0 | 58 (54.2) |
| Patients with INOCA | 67 (62.6) |
| Patients with IMR ≥25.0 | 18 (26.9) |
| Patients with CFR ≤2.0 | 21 (34.4) |
| Values presented as mean±SD or n (%). CFR: coronary flow reserve; FFR: fractional flow reserve; IMR: index of microvascular resistance; INOCA: ischaemia with non-obstructive coronary artery disease; LAD: left anterior descending; LCx: left circumflex; LMT: left main trunk; RCA: right coronary artery; Tmn: mean transit time | |
Primary and secondary objectives
In total, 42 (39.3%) patients showed a DS >50%, whereas haemodynamically significant stenosis (FFR ≤0.80) was present in 40 (37.4%). Coronary microvascular dysfunction (IMR ≥25) was detected in 20.6%, while disease in both the epicardial and microvascular compartments was present in 3.7% of patients with an intermediate probability of CAD and positive exercise tests (Figure 3). The FDR with the classical QCA criteria of 50% DS was 60.7%. There was no significant reduction of the FDR by measuring FFR (60.7% vs 62.6%; p=0.803). In contrast, the addition of IMR significantly reduced the proportion of false-positive stress tests compared to both QCA and FFR (p<0.05 for both). The combination of QCA and IMR provided a similar reduction in the FDR (Central illustration). The assessment of the FDR with other QCA diameter stenosis cut-offs is shown in Supplementary Figure 1. A case example of the incremental diagnostic value of the IMR is shown in Figure 4.
In 67 patients with INOCA (FFR>0.80 and/or QCA DS ≤50%), the mean IMR was 21.2±12.8 and mean CFR 3.0±2.2. In this group, the prevalence of CMD was 26.9%. In the overall population, 33 patients underwent revascularisation procedures (28, percutaneous coronary intervention [PCI] and 8, coronary artery bypass graft surgery). Details of the PCI are shown in Supplementary Table 6.
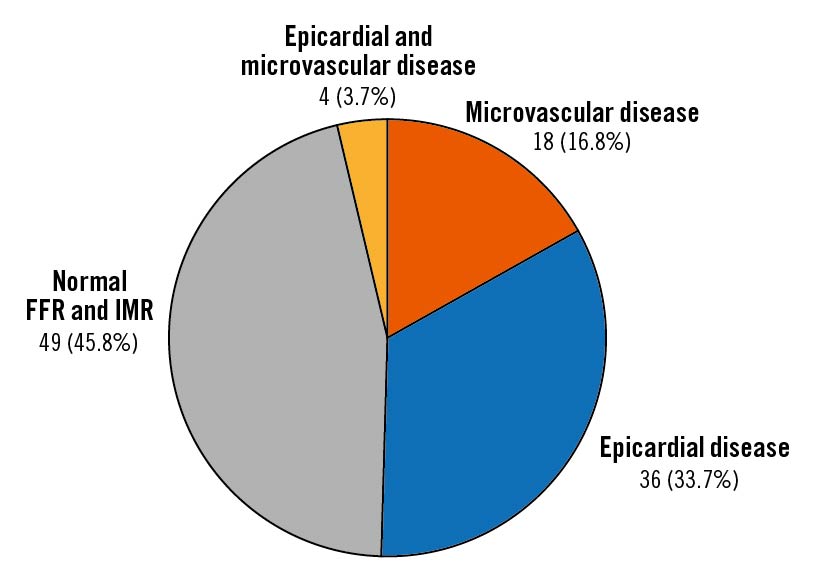
Figure 3. Distribution of invasive coronary physiology findings. Overall, in 54.2% of patients, evidence of haemodynamically significant epicardial or microvascular disease was found. In 16.8% of patients, coronary microvascular dysfunction (IMR ≥25) was observed. In 33.7%, a significant lesion based on FFR (≤0.80) was detected, whereas in 3.7% an alteration of both epicardial and microvascular domains was noticed. FFR: fractional flow reserve; IMR: index of microvascular resistance
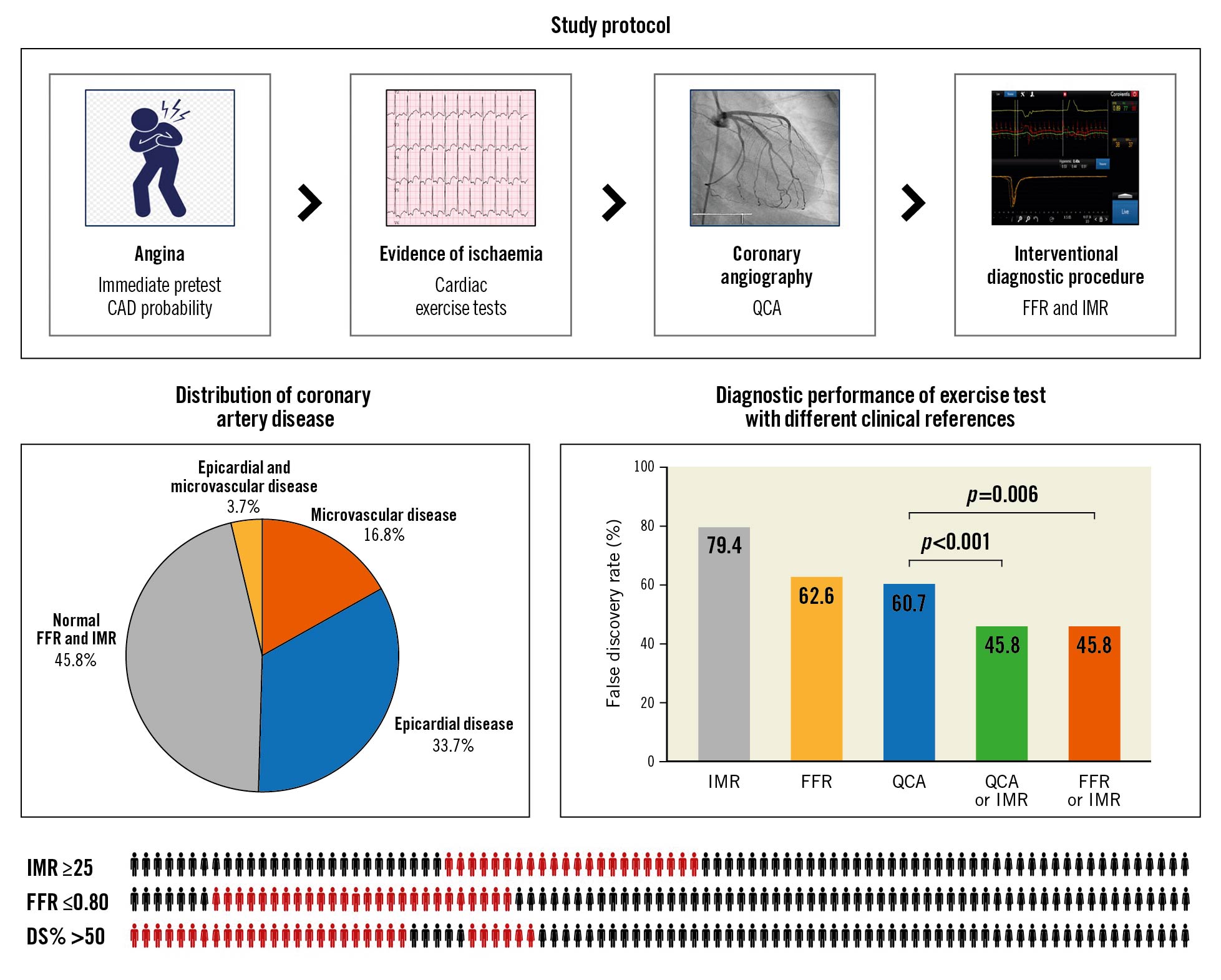
Central illustration. Study protocol and main results. The study protocol included symptomatic patients with an intermediate probability of coronary artery disease (CAD) and evidence of ischaemia. The study was to determine the diagnostic accuracy of exercise stress testing using both FFR and IMR as clinical references. Approximately half of the patients had evidence of epicardial or microvascular CAD. An invasive diagnostic procedure accounting for both epicardial and microvascular compartments improved the diagnostic performance of exercise tests through a significant reduction in the false discovery rate. The bottom of the figure shows the individual results of the index of microvascular resistance, fractional flow reserve, and quantitative coronary angiography. The red icon represents abnormal tests based on the metric-specific cut-offs. CAD: coronary artery disease; DS%: percentage diameter stenosis; FFR: fractional flow reserve; IMR: index of microvascular resistance; QCA: quantitative coronary angiography
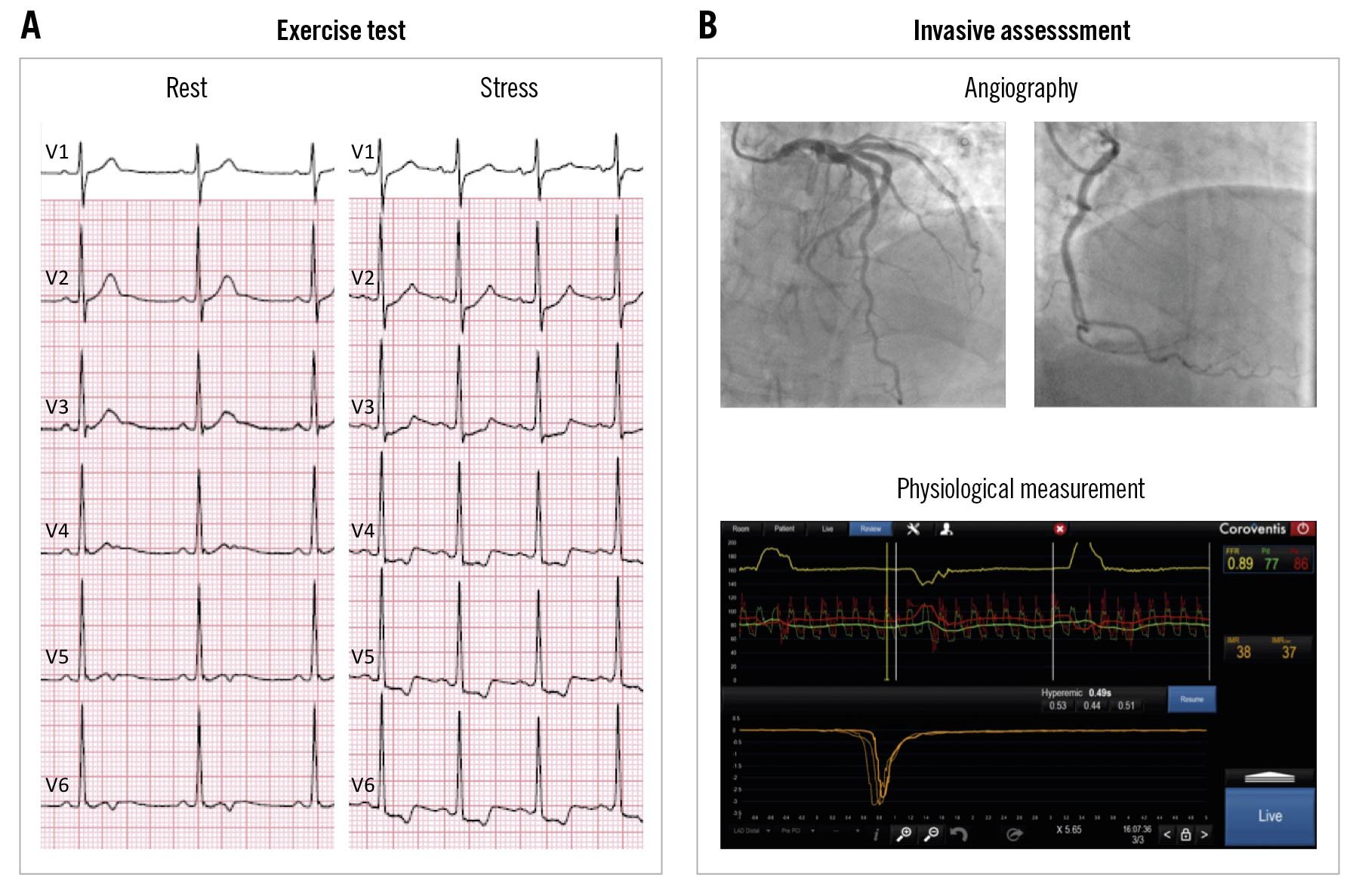
Figure 4. Case example of a positive exercise test and coronary microvascular dysfunction. A 54-year-old male with dyslipidaemia presenting with typical angina. A) The exercise test with an electrocardiogram in rest and during exercise. The test was considered positive due to ST depression of 2 mm and chest pain during exercise. B) Coronary angiography showed no obstructive coronary artery disease. The invasive diagnostic protocol showed an FFR of 0.89 and an IMR of 38. Therefore, the patient was diagnosed with microvascular angina. FFR: fractional flow reserve; IMR: index of microvascular resistance
Discussion
The main findings of the present study can be summarised as follows: (1) approximately half of the patients presenting with chest pain with intermediate pretest probability of CAD and positive stress tests had evidence of epicardial or microvascular CAD; (2) in INOCA patients, the prevalence of CMD was 27%; and (3) an invasive functional assessment accounting for both epicardial and microvascular compartments led to an improvement in the diagnostic performance of exercise tests through a significant reduction in the false discovery rate.
Non-invasive diagnostic testing is a core component of the evaluation of stable patients presenting with chest pain. The American and European guidelines recommend non-invasive cardiac assessment for patients with an intermediate pretest likelihood of CAD12. While recent guidelines emphasise the role of coronary computed tomography (CT) angiography as a first-line test, the exercise ECG stress testing is the lowest-cost procedure and is widely accessible. In the International Study of Comparative Health Effectiveness With Medical and Invasive Approaches (ISCHEMIA) trial, 25% of the randomised patients were screened using exercise stress tests12. The diagnostic accuracy of exercise electrocardiography test-induced ST depression has been compared to coronary angiography diameter stenosis and has shown wide variability in sensitivity and specificity, ranging from 23% to 100% and 17% to 100%, respectively3. An important limitation of these studies is that coronary angiography DS of 50% was used as the diagnostic gold standard. In the Fractional Flow Reserve Guided PCI Plus Optimal Medical Treatment (OMT) Versus OMT (FAME II) trial, 19% of lesions with DS <50% showed haemodynamic significance, while 65% of lesions with DS between 50-70% had an FFR>0.8013. Consequently, conventional angiography is limited in predicting the haemodynamic effects of epicardial stenosis. In the present study, all patients had a reversible ST-segment depression, and 39% had DS >50%; of these patients, 80% had abnormal FFR. To the best of our knowledge, the present study is the first to assess the diagnostic performance of an exercise electrocardiography test with FFR as a reference standard; this contemporary methodological approach did not improve the diagnostic performance of the exercise tests.
Coronary microvascular dysfunction is one of the contributing mechanisms to INOCA7. CMD limits myocardial perfusion and can lead to abnormal non-invasive tests. Moreover, a non-invasive test indicative of ischaemia is a key criterion for diagnosing microvascular angina. Consequently, testing for CMD is recommended for patients who have chest pain, an abnormal result of stress testing and coronary arteries without obstructive coronary artery disease11. In this population, the prevalence of CMD reported by studies using CFR as a diagnostic criterion ranges from 30% to 50%. IMR is a contemporary invasive method proxy of microvascular resistance. A high IMR (>40) has been associated with microvascular obstruction by cardiovascular magnetic resonance imaging and with worse clinical outcomes after primary PCI1315. In stable patients, an IMR ≥25 is considered a diagnostic criterion for CMD11. In this study, 27% of cases without obstructive CAD had evidence of CMD (Supplementary Table 4). The inclusion of IMR as part of the clinical standard for performance evaluation of the exercise tests led to a 25% reduction in FDR (p-value <0.001), thereby reclassifying 1 out of 5 patients otherwise considered as having false-positive tests. The diagnosis of CMD has been shown to impact patients’ quality of life. In the British Heart Foundation’s CORonary MICrovascular Angina (CorMicA) Trial, among patients with non-obstructive CAD, microvascular angina based on IMR was present in 52% of patients10. The IDP with associated medical therapy improved angina and quality of life, persisting up to 1 year after diagnosis16. Moreover, establishing a diagnosis in this subgroup of patients may reduce downstream cardiac and non-cardiac tests and decrease resource utilisation.
The present study has several clinical implications. First, it confirms the modest performance of exercise stress tests to detect CAD even when accounting for the total coronary circulation. Despite the addition of a systematic pressure wire-based assessment of both epicardial and microvascular coronary artery compartments, almost half of the non-invasive test results were not explained by the invasive measurements. In almost half of the patients presenting with symptoms, moderate pretest probability of CAD, and evidence of ischaemia on non-invasive tests, no evidence of epicardial or microvascular disease was found. These results mirror the findings of the American College of Cardiology National Cardiovascular Data Registry, showing that positive results on a non-invasive test in the presence of typical angina yield an obstructive CAD rate of approximately 50%4. Therefore, current strategies, including non-invasive testing, need to be improved to increase the diagnostic yield of coronary angiography4. Second, it highlights the usefulness of an IDP for assessing CMD in patients with evidence of ischaemia in non-invasive tests. The IMR is a relatively accessible technique that is simple to perform and adds approximately 3 to 5 minutes to a diagnostic procedure1517. Based on the high proportion of patients referred to the catheterisation laboratory in whom obstructive CAD is absent, the findings of the present study show that a systematic approach for the evaluation of the coronary microcirculation has the potential to improve clinical care in symptomatic patients with ischaemia.
Limitations
This study has several limitations. First, the diagnostic performance of the exercise stress test was evaluated in terms of FDR; this approach is based on the assumption that CMD is an entity able to induce myocardial ischaemia, and thus, adding IMR to FFR allows for distinguishing populations with different disease endotypes. A classical analytic approach based on sensitivity, specificity, and accuracy would have been preferred; nonetheless, this was not feasible because patients with a negative non-invasive test are usually not referred for invasive coronary angiography. Second, the study protocol did not include acetylcholine endothelial function testing to detect epicardial or microvascular spasms, which has also been associated with abnormal non-invasive tests18. This was due to the limited availability of this drug in Europe. Third, women represented only 27% of the study population; CMD is believed to be more prevalent among women; therefore, the value of microvascular assessment might be even higher in a more balanced population19. Fourth, we cannot exclude selection or workup bias since some patients with abnormal exercise tests might have been referred to another test (e.g., coronary CT angiography). Fifth, we did not perform a systematic physiological assessment in multiple epicardial vessels. Although it was recommended by protocol, this was only accomplished in 19% of cases. Finally, the initial target population was not recruited, and the trial was stopped prematurely. This decision was taken after observing a decreased volume of exercise tests in the participating hospitals due to the COVID-19 pandemic.
Conclusions
Slightly more than half of the patients with non-invasive evidence of ischaemia who underwent an invasive diagnostic procedure had obstructive or microvascular coronary artery disease. A systematic evaluation of the epicardial and microvascular compartments led to a significant false discovery rate reduction. Assessing the coronary microcirculation in stable patients presenting with evidence of ischaemia improved the diagnostic performance of exercise stress tests.
Impact on daily practice
In this prospective study, including symptomatic patients with an intermediate pretest probability of coronary artery disease and positive exercise stress tests, the combination of FFR and IMR reduced the false discovery rate of the exercise test by 25% compared to quantitative coronary angiography. Accounting for the microvascular compartment during invasive physiological assessment in patients with ischaemia led to a significant improvement in diagnostic performance and test interpretation and reclassified 1 in 5 patients otherwise considered as having a false-positive non-invasive test.
Conflict of interest statement
D. Andreini reports receiving research grants from GE Healthcare and Bracco. T. Mizukami reports receiving consulting fees from Zeon Medical, research grants from Boston Scientific, and speaker fees from Abbott, CathWorks, and Boston Scientific. N. Mileva reports receiving speaker fees from Abbott. D. Munhoz reports receiving research grants provided by the CardioPaTh PhD program. E. Barbato reports receiving speaker's fees from Boston Scientific, Abbott, GE Healthcare, Insight Lifetech, and OpSens. B. De Bruyne reports receiving consultancy fees from Boston Scientific and Abbott, research grants from Coroventis Research, Pie Medical Imaging, CathWorks, Boston Scientific, Siemens, HeartFlow, and Abbott, and owning equity in Siemens, GE Healthcare, Philips, HeartFlow, Edwards Lifesciences, Bayer, Sanofi, and Celyad. B. Cosyns reports receiving consulting fees from Philips and Boehringer Ingelheim, participation on the Board of Novartis and Pfizer; is President of the EACVI; and is a board member of the ESC and the Belgian Society of Cardiology. C. Collet reports receiving research grants from Biosensors International, Coroventis Research, Medis Medical Imaging, Pie Medical Imaging, CathWorks, Boston Scientific, Siemens, HeartFlow, and Abbott, and consultancy fees from HeartFlow, OpSens, Abbott, and Philips. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.