CASE SUMMARY
BACKGROUND: A 66-year-old male with crescendo angina pectoris with persisting disabling angina despite optimal medical therapy. Coronary angiography in the referral hospital showed a stenosis of intermediate severity in the first diagonal branch.
INVESTIGATION: Physical examination, electrocardiogram, exercise testing, transthoracic echocardiogram, coronary angiography, functional stenosis severity assessment.
DIAGNOSIS: Depletion of coronary vasodilatory reserve in the presence of a focal stenosis of intermediate severity superimposed on a background of small vessel disease.
MANAGEMENT: Stenting of the stenosis in the diagonal branch to increase vasodilatory reserve.
KEYWORDS: coronary autoregulation, coronary flow velocity reserve, discordance, fractional flow reserve, functional lesion severity assessment
PRESENTATION OF THE CASE
A 66-year-old male presented to the outpatient clinic of a referral hospital with typical crescendo angina pectoris. His angina markedly limited his physical activity, and was classified as New York Heart Association (NYHA) Class III. Risk factors for coronary artery disease included insulin-dependent diabetes mellitus, hypertension, obesity and smoking. Exercise electrocardiography was positive and showed downsloping ST segments in II, III, AvF, V5, V6. Transthoracic echocardiography demonstrated moderately dilated left and right atria, and a mildly hypertrophic left ventricle with diastolic dysfunction, but normal systolic function. Coronary angiography was performed in the referral hospital because of the positive exercise test, and persistence of disabling angina pectoris despite optimal medical therapy with aspirin 100 mg daily, pravastatin 10 mg daily, bisoprolol 5 mg daily, isosorbide mononitrate 100 mg daily and nifedipine 90 mg daily. Blood pressure at the referral hospital was found to be 194/65 mmHg at a heart rate of 64 beats per minute, his serum glucose level was 11.2 mmol/l and no information was available on total cholesterol, HDL and LDL.
At angiography, a visually intermediate stenosis (50%) in the first diagonal branch was documented. In accordance with the subsequent multidisciplinary Heart Team discussion, the patient was referred to our institution for physiological stenosis severity assessment to guide decision making on potential percutaneous coronary intervention. Cardiac catheterisation was performed according to routine procedures and, accordingly, the patient stopped caffeine intake at least eight hours prior to the procedure. Notably, at cardiac catheterisation, the patient had a blood pressure of 180/75 mmHg at a heart rate of 77 beats per minute. After intracoronary administration of nitroglycerine (200 μg), a ComboWire® (Volcano Corp., San Diego, CA, USA) was positioned distal to the stenosis in the first diagonal branch. A stable Doppler flow signal was acquired by flipping the tip of the ComboWire (Figure 1, Moving image 1), and obtaining the Doppler signal retrogradely. Intracoronary pressure and blood flow velocity were recorded during resting conditions, as well as during hyperaemia induced by the administration of an intracoronary bolus of adenosine (40-60 μg) to obtain the fractional flow reserve (FFR) as well as the coronary flow velocity reserve (CFR).

Figure 1. Coronary angiogram showing a visually intermediate stenosis (50%) in the first diagonal branch (white arrow). In addition, combined pressure and Doppler flow velocity recordings were acquired using a ComboWire® (Volcano Corp.) positioned distal to the stenosis. A stable Doppler flow signal was established by flipping the tip of the ComboWire, and obtaining the Doppler signal retrogradely.
Notably, discordant results of FFR and CFR were obtained, where FFR was normal at 0.90 (deferral threshold of >0.80), whereas CFR at 1.7 was vastly below the interventional threshold (deferral threshold of >2.0). Because of these ambiguous results in the presence of typical angina symptoms and inducible ischaemia on exercise ECG, combined pressure and flow velocity parameters, the hyperaemic stenosis resistance index (HSR), defined as the pressure gradient across the stenosis (Pa-Pd) divided by the averaged peak velocity (APV), and the hyperaemic microvascular resistance index (HMR), defined as the distal pressure (Pd) divided by the averaged peak velocity (APV), were additionally evaluated. Both HSR and HMR are readily available on the ComboMap® system (Volcano Corp., San Diego, CA, USA). HSR was found to be low, 0.27 mmHg∙cm∙s–1 (deferral threshold ≤0.8 mmHg∙cm∙s–1)1, and HMR was high, 2.6 mmHg∙cm∙s–1 (reference values ranging from 1.85-2.05 mmHg∙cm∙s–1)2-4 (Figure 1, Moving image 1).
How would I treat?
THE INVITED EXPERTS’ OPINION
In this 66-year-old diabetic patient with chest pain, tailored medical therapy should be advocated along with the control of all risk factors, a drastic loss of weight, regular and intense physical exercise, and reassurance of the patient and his family. While stenting of this stenosis would be particularly easy, and even though the placebo effect of “fixing a coronary blockage” cannot be excluded, revascularisation cannot be justified in this patient. The reasons are the following:
1. The truly ischaemic nature of the chest pain is questionable. The invalidating complaints (CCS III) are extremely unlikely to be related to a mild stenosis in a small diagonal branch. The complaints are reported to be “crescendo” suggesting instability of the process, while all clinical data point towards a chronic condition (left ventricular hypertrophy [LVH], diabetes, arterial hypertension [AHT], the morphology of the stenosis in the diagonal branch). The authors themselves were unsure about the nature of the complaints, otherwise one may wonder why a stress test was performed in a patient with four major risk factors and “typical crescendo angina”. The results of this stress test should be considered aspecific: no chest pain occurred (while this diabetic patient is reported to have CCS III symptoms), and downsloping ST depressions were observed –a typical finding in LVH– from the inferolateral leads, when they would have been from the anterolateral leads in order to be ascribed to the diagonal branch.
2. There is certainly room to improve the medical therapy: a pressure of 180/80 mmHg and a heart rate of 77 bpm suggest insufficient beta-blockade. The association of long-acting calcium entry blockers should be considered to preclude (paradoxical) vasoconstriction.
3. Revascularisation of lesions with an FFR greater than 0.80 has no prognostic implications, especially not in a small diagonal branch.
4. A CFR value of 1.7 associated with an FFR value of 0.90 indicates largely predominant microvascular disease. The latter is not surprising in the presence of diabetes, obesity, LVH and AHT. An FFR of 0.90 means that optimal stent implantation would increase maximal flow by 10%. In this case CFR would reach 1.87, a value that is still too low to ascertain the absence of ischaemia. In contrast to a common erroneous belief, this has nothing to do with “discordant” values.
5. The long, diffuse infiltration of the stiff-looking mid and distal LAD, a vessel supplying a markedly larger myocardial mass, is actually more concerning than the mild stenosis in the small diagonal branch. Therefore, after measuring the diagonal branch, it would have been interesting to quantify the haemodynamics of the LAD. An abnormal FFR in the LAD would not be surprising, and would justify the placement of a LIMA with its well-known prognostic implications, especially in a diabetic patient.
Conflict of interest statement
B. De Bruyne reports that his institution receives grant support and consulting fees on his behalf from St. Jude Medical. The other author has no conflicts of interest to declare.
How would I treat?
THE INVITED EXPERT’S OPINION
Several aspects of the data imply that the stenosis is physiologically mild and unlikely to be the cause of the symptoms. The pressure gradient is small at rest and during hyperaemia. Flow velocity tracings show no characteristic phasic flow damping expected from a severe stenosis. The flow velocity reserve of 1.7 is not normal but reduced due to either diffuse disease (a pullback pressure tracing is not provided) or microvascular disease, or a mixture of both, or caffeine preventing hyperaemia.
My measurements indicate a 50% diameter stenosis in a small diameter diagonal branch similar in its widest calibre to the guiding catheter, indicating mild stenosis and severe diffuse disease. Stenosis geometry is smooth without evidence of plaque rupture or clot, thereby making transient thrombosis or emboli unlikely, hence stable disease with more favourable prognosis than acute coronary syndromes.
Is the angina truly refractory? The baseline blood pressure of approximately 180/80 mmHg and heart rate of 77/minute indicate suboptimal medical therapy, but medications are not listed. Reducing the pressure-rate product by medications lowers myocardial oxygen demand and reduces symptoms. Both randomised trials and my clinical experience confirm that the vast majority of patients achieve angina relief with combined lifestyle changes plus optimal medical therapy. Additionally, a wide pulse pressure of 100 mmHg in this case warrants exploration for aortic regurgitation or myocardial disease.
Assuming true refractory angina, several mechanisms can explain angina with low flow capacity and no significant pressure gradient: first, coronary spasm superimposed on this mild stenosis; second, diffuse disease together with a mild stenosis; third, vasodilation blunted by residual caffeine; fourth, microvascular disease due to upstream atherosclerosis or primary vasomotor dysfunction.
Before going to the cathlab, I routinely perform quantitative stress PET perfusion imaging in all patients to quantify precisely either adequate or ischaemic low flow in the distribution of every coronary artery or their sub-branches and/or whether quantitative perfusion is globally reduced indicating severe diffuse disease. Caffeine levels are obtained in all my patients undergoing PET, to confirm the precise global and regional coronary flow capacity as a specific reliable indication for PCI or not, on every specific artery or branch.
In my practice, such patients rarely reach the catheterisation laboratory since I am able to distinguish among the above possibilities in the vast majority of cases. In this case, I would have stopped the diagnostic angiogram, done the quantitative PET imaging, ruled out valve disease and adequately treated the patient to lower BP to 120 and HR to 55 or lower. Only then, after review of patient preference, would I have proceeded with percutaneous coronary intervention on the grounds of: i) refractory spasm superimposed on mild structural stenosis paralleling no ischaemia by PET, or ii) mild stenosis superimposed on diffuse disease, where the combined disease may cause ischaemia with insignificant pressure gradient but relief of angina due to improving coronary flow, even modestly, in the face of diffuse disease paralleling globally reduced stress perfusion and CFR by PET.
Conflict of interest statement
K.L. Gould receives internal funding from the Weatherhead PET Center for Preventing and Reversing Atherosclerosis. He is also the 510(k) applicant for cfrQuant approved by the FDA. He has arranged that all his royalties permanently go to a University of Texas (UT) scholarship fund. UT has a commercial non-exclusive agreement with Positron Corporation to distribute and market cfrQuant in exchange for royalties. However, he retains the ability to distribute cost-free versions to selected collaborators for research. Additionally, K.L. Gould has signed a non-financial, mutual non-disclosure agreement with Volcano Corporation and St. Jude Medical (makers of FFR pressure wires) to discuss coronary physiology projects, and has research support from these companies to his institution unrelated to any aspect of this manuscript.
How did I treat?
ACTUAL TREATMENT AND MANAGEMENT OF THE CASE
Despite a normal FFR, percutaneous coronary intervention of the intermediate stenosis in the first diagonal branch was performed. The decision was governed by the combination of typical crescendo angina pectoris irresponsive to optimal medical therapy, a vastly positive exercise test highly specific for inducible myocardial ischaemia, and the presence of a low CFR and high HMR, indicating a compromised coronary microvasculature operating at the limits of its vasodilatory reserve. After predilatation at 10 atmospheres, a drug-eluting endothelial progenitor cell-capturing stent (Combo™ Stent; OrbusNeich Medical, Fort Lauderdale, FL, USA) 2.5 mm×13 mm was placed and post-dilated at 14 atmospheres. Post-procedurally, physiological measurements were repeated to evaluate the result of the revascularisation. Blood pressure and heart rate remained unchanged at 190/80 mmHg and 70 beats per minute, respectively. FFR and CFR both improved and were now concordantly normal, with an FFR of 0.96 and a CFR of 2.4. HSR and HMR improved as well, with an HSR of 0.04 mmHg∙cm∙s–1, and an HMR of 2.0 mmHg∙cm∙s–1 (Figure 2, Moving image 2). According to standard practice, clopidogrel 75 mg daily was added to the patient’s medical therapy to establish DAPT.
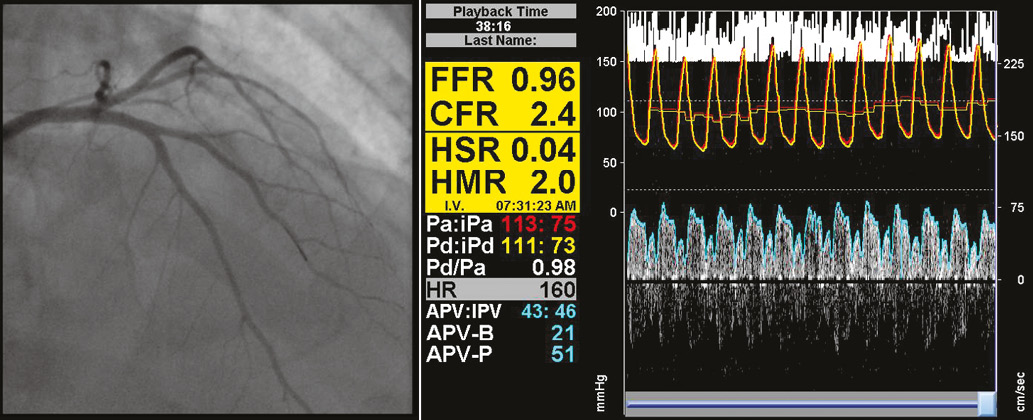
Figure 2. Coronary angiogram showing the visual result after PCI was performed of the intermediate stenosis in the first diagonal branch. In addition, combined pressure and Doppler flow velocity recordings were repeated using a ComboWire® (Volcano Corp.). A stable Doppler flow signal was established by flipping the tip of the ComboWire (Figure 1), and obtaining the Doppler signal retrogradely.
At one month telephone follow-up, the patient reported relief of his angina symptoms, despite no material changes in his medical therapy. At one-year clinical follow-up, the patient still reported a relief of his anginal symptoms. He now received amlodipine 5 mg daily, doxazosin 4 mg daily, irbesartan 300 mg daily, and hydrochlorothiazide 12.5 mg daily. Nonetheless, his blood pressure remained elevated at 165/75 mmHg at a heart rate of 68 beats per minute. His total cholesterol was 2.6 mmol/l, HDL was 1.1 mmol/l and LDL was 0.9 mmol/l. No information on the serum glucose level was available at time of follow-up.
Discussion
The limitations of coronary angiography to document the functional significance of coronary artery disease have long been recognised, particularly in stenoses of intermediate angiographic severity. As a result, physiological indices are increasingly being used to guide revascularisation. FFR is the most widely used measure of functional stenosis severity in clinical practice, and has been proven to result in superior clinical outcomes compared to angiography-guided revascularisation5. FFR aims to estimate the flow-limiting effects of a coronary stenosis by means of coronary pressure measurements, and is reported to be governed by the extent of epicardial disease. Nonetheless, the pivotal FAME II study documented that over 70% of FFR-positive stenoses, e.g., stenoses that require PCI according to contemporary clinical practice guidelines (FFR ≤0.80), do not actually require PCI during the first year of follow-up if revascularisation is initially deferred. Moreover, the FAME II investigators documented that, in stenoses with a normal FFR (FFR>0.80), although clinical outcome is favourable, a risk for major adverse cardiac events still exists. Hence, despite the notion of strict cut-off value-based FFR-guided decision making in clinical practice guidelines, functional coronary artery disease severity seems to go beyond coronary pressure.
In the light of an increasing recognition of microvascular disease as an important component in the spectrum of coronary artery disease, it is important to recognise that contemporary coronary-pressure-based assessment of the coronary artery disease by means of FFR has two important limitations: 1) a pressure-only parameter such as FFR is by definition unable to identify the relative involvement of the epicardial vessel and the coronary microcirculation, and 2) coronary pressure measurements may be obscured by the effects of microvascular disease on distal coronary pressure. Despite being long neglected as a functional parameter of the coronary vasculature, CFR is increasingly reported as a measure of combined epicardial and microvascular disease severity. The combination of both FFR and CFR was recently reported to provide a comprehensive evaluation of the pathophysiology of coronary artery disease in a specific patient. In particular, the discordance between FFR and CFR is now recognised as occurring from typical pathophysiological patterns, and specifically as resulting from the relative involvement of the epicardial vessel and the coronary microcirculation. However, the interpretation of discordant results between FFR and CFR in order to guide decision making in the catheterisation laboratory may be more difficult.
The clinical relevance of CFR and FFR discordance
By definition, the pressure drop across the stenosis depends on the flow through the stenosis. The pressure drop increases with increasing coronary flow, and vice versa, and a change in flow thus induces a change in distal pressure, and FFR, in the opposite direction of the change in flow, and CFR. Since coronary flow is in turn dictated by microcirculatory resistance, a change in the latter influences CFR and FFR in opposite directions, potentially causing discordant results. Discordance between CFR and FFR is present in 30-40% of stenoses routinely assessed in clinical practice3, and yields important information on the epicardial and microcirculatory contribution to blood flow impairment.
Three regions of discordance can be identified by combined measurements of CFR and FFR6. The presence of a near normal FFR (roughly 0.95 or greater) with reduced CFR (<2.0) defines pure small vessel or microcirculatory disease. On the other hand, a reduced FFR (≤0.80) with preserved CFR (>2.0) represents a focal epicardial stenosis with adequate flow reserve above ischaemic thresholds and minimal diffuse or microcirculatory disease: a non-flow-limiting epicardial stenosis. Finally, a preserved FFR (>0.80) with reduced CFR (<2.0) represents a moderate focal epicardial stenosis superimposed on a background of severe diffuse and/or microcirculatory disease. In particular, this presence of microcirculatory disease, regardless of epicardial patency, is associated with a significant increase in fatal events at long-term follow-up7. The patient in the presented case had several risk factors associated with microcirculatory disease (e.g., diabetes, smoking, arterial hypertension, obesity)8. The presence of microcirculatory disease was confirmed by advanced physiological assessment, revealing an abnormal CFR with a normal FFR, which is physiologically explained by a physiologically moderate epicardial stenosis (HSR 0.27 mmHg · cm · s–1), superimposed on substantially increased coronary microcirculatory resistance (HMR 2.6 mmHg ∙ cm ∙ s–1), in the presence of increased myocardial oxygen demand by arterial hypertension indicated by a high baseline averaged peak velocity (24 cm/sec).
Contribution of microcirculatory disease: a diagnostic and therapeutic dilemma
In patients with stable angina, microcirculatory disease may contribute to, or even exclusively determine, the occurrence of myocardial ischaemia. It is likely that microcirculatory disease not only impairs the maximal achievable blood flow, but additionally depletes the coronary vasodilatory reserve. In response to the increase in microvascular resistance, the autoregulatory resistance vessels dilate to allow an increased flow into the microvasculature to maintain adequate flow to the myocardium; ischaemia occurs when myocardial oxygen demand exceeds vasodilatory reserve1. The presence of epicardial stenosis in addition to microvascular disease makes an even stronger appeal to the vasodilatory reserve, thereby further impairing the ability to adjust myocardial flow to an increase in myocardial oxygen demand. Hence, a depleted vasodilatory reserve secondary to the combined functional effects of epicardial and microcirculatory disease is likely to result in ischaemia at the slightest increase in myocardial oxygen demand.
The patient described in this case report indeed showed a depleted vasodilatory reserve in the presence of an intermediate coronary stenosis. In addition, this reserve was further compromised by the presence of arterial hypertension, increasing myocardial demand. The effect of epicardial stenosis alleviation on the magnitude of distal microvascular resistance is currently debated, and hence the applicability of mechanical revascularisation of an intermediate stenosis in the presence of predominant microvascular abnormalities can be argued. However, restoration of perfusion pressure is associated with a decrease in the minimal resistance of the microvasculature, and probably partly restores the vasodilatory reserve by alleviation of the strain on the compensatory autoregulatory vasodilation9. It must be noted that this area of research is evolving, and that no evidence is available which conclusively supports that reduction of microvascular resistance in this setting is associated with alleviation of myocardial ischaemia and its symptoms. Nevertheless, in this patient with evidence and symptoms of inducible myocardial ischaemia despite optimal medical therapy, hypertension, and substantially increased microvascular resistance, alleviation of an intermediate stenosis was associated with partial alleviation of microcirculatory resistance and an improvement in subjective angina complaints at one month, and one-year follow-up.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. Coronary angiogram showing a visually intermediate stenosis (50%) in the first diagonal branch (white arrow). In addition, combined pressure and Doppler flow velocity recordings were acquired using a ComboWire (Volcano Corp.) positioned distal to the stenosis. A stable Doppler flow signal was established by flipping the tip of the ComboWire, and obtaining the Doppler signal retrogradely.
Moving image 2. Coronary angiogram showing the visual result after PCI was performed of the intermediate stenosis in the first diagonal branch. In addition, combined pressure and Doppler flow velocity recordings were repeated using a ComboWire (Volcano Corp.). A stable Doppler flow signal was established by flipping the tip of the ComboWire (Figure1), and obtaining the Doppler signal retrogradely.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Coronary angiogram showing a visually intermediate stenosis (50%) in the first diagonal branch (white arrow). In addition, combined pressure and Doppler flow velocity recordings were acquired using a ComboWire (Volcano Corp.) positioned distal to the stenosis. A stable Doppler flow signal was established by flipping the tip of the ComboWire, and obtaining the Doppler signal retrogradely.
Moving image 2. Coronary angiogram showing the visual result after PCI was performed of the intermediate stenosis in the first diagonal branch. In addition, combined pressure and Doppler flow velocity recordings were repeated using a ComboWire (Volcano Corp.). A stable Doppler flow signal was established by flipping the tip of the ComboWire (Figure1), and obtaining the Doppler signal retrogradely.