Abstract
Aims: Assessment of microvascular function in patients with ST-elevation acute myocardial infarction (STEMI) may be useful to determine treatment strategy. The possible role of pressure-bounded coronary flow reserve (pb-CFR) in this setting has not been determined. In this study we aimed to compare pb-CFR with thermodilution-derived physiology including the index of microcirculatory resistance (IMR) and CFRthermo in a consecutive series of patients enrolled in the OxAMI study. Moreover, we aimed to assess the presence of microvascular obstruction (MVO) and myocardial injury on cardiovascular magnetic resonance (CMR) imaging performed at 48 hours and six months in STEMI patients stratified according to pb-CFR.
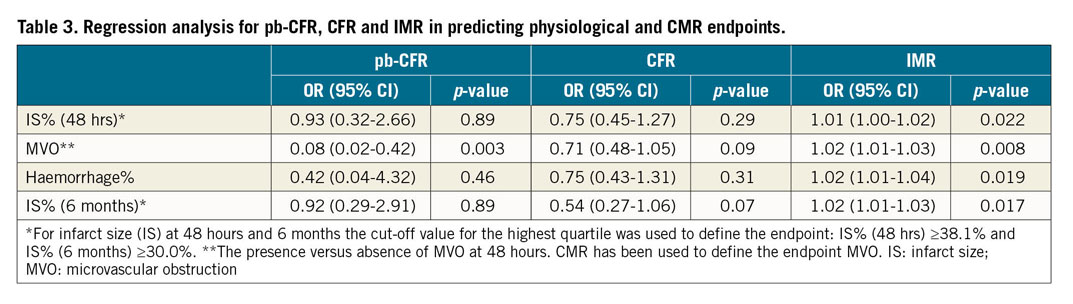
Methods and results: Thermodilution-pressure-wire assessment of the infarct-related artery was performed in 148 STEMI patients before stenting and/or at completion of primary percutaneous coronary intervention (PPCI). The extent of the myocardial injury was assessed with CMR imaging at 48 hours and six months after STEMI. Post-PPCI pb-CFR was impaired (<2) and normal (>2) in 69.9% and 9.0% of the cases, respectively. In the remaining 21.1% of the patients, pb-CFR was “indeterminate”. In this cohort, pb-CFR correlated poorly with thermodilution-derived coronary flow reserve (k=0.03, p=0.39). The IMR was significantly different across the pb-CFR subgroups. Similarly, significant differences were observed in MVO, myocardium area at risk and 48-hour infarct size (IS). A trend towards lower six-month IS was observed in patients with high (>2) post-PPCI pb-CFR. Nevertheless, pb-CFR was inferior to IMR in predicting MVO and the extent of IS.
Conclusions: Pb-CFR can identify microvascular dysfunction in patients after STEMI. It provided superior diagnostic performance compared to thermodilution-derived CFR in predicting MVO. However, IMR was superior to both pb-CFR and thermodilution-derived CFR and, consequently, IMR was the most accurate in predicting all of the studied CMR endpoints of myocardial injury after PPCI.
Introduction
Coronary physiology is a useful tool to assess the extent of coronary microvascular dysfunction in patients with ST-elevation acute myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention (PPCI)1.
The presence of microvascular obstruction (MVO) or high values of index of microcirculatory resistance (IMR) have been associated with poor myocardial reperfusion after PPCI, larger infarct size and worse long-term clinical outcome1,2,3. Moreover, STEMI patients with high IMR are at increased risk of post-procedural and in-hospital complications compared with patients with low post-PPCI IMR4.
However, the use of coronary physiology to assess the extent of microvascular dysfunction in STEMI patients remains limited in routine clinical practice, partly because of the complexity of the available techniques to assess coronary flow and coronary resistance in the catheterisation laboratory5.
Recently, pressure-bounded coronary flow reserve (pb-CFR) has been proposed to estimate CFR using standard pressure-wire technology, obviating the need for intracoronary thermodilution or Doppler-velocity measurements6. pb-CFR demonstrated a good correlation with Doppler and thermodilution-derived CFR (CFRthermo) although its value to predict clinical outcomes remains uncertain6,7,8.
The diagnostic accuracy of pb-CFR in detecting the extent of coronary microvascular dysfunction and predicting myocardial injury has not been assessed in patients with STEMI. In this study, we aimed to compare pb-CFR with thermodilution-derived physiology including IMR and CFRthermo in a consecutive series of patients enrolled in the Oxford Acute Myocardial Infarction (OxAMI) study. Moreover, we aimed to assess the presence of MVO and myocardial injury on cardiovascular magnetic resonance imaging (CMR) performed at 48 hours and six months in STEMI patients stratified according to pb-CFR.
Methods
Patients with STEMI admitted to the Oxford Heart Centre for PPCI were prospectively considered for enrolment in the OxAMI study (REC number 10/H0408/24). The study protocol was approved by the local ethics committee and the study was conducted in accordance with the Declaration of Helsinki.
Details of the OxAMI study have been described previously1. The diagnosis of STEMI required chest pain lasting at least 30 minutes, within 12 hours from onset of symptoms, and ST-segment elevation of >2 mm (0.2 mV) in at least two contiguous leads on ECG. Symptom duration >12 hours, presence of severe haemodynamic instability, severe left main disease, contraindications to adenosine infusion, balloon angioplasty without stent implantation and general contraindications to CMR were all exclusion criteria for this analysis.
PPCI was performed in a standard fashion and decisions about direct stenting technique, thrombectomy and glycoprotein IIb/IIIa adoption were all left to the operator’s discretion. All patients were loaded with dual antiplatelet therapy. Weight-adjusted unfractionated heparin or bivalirudin was adopted as antithrombotic regimen. Angiographic thrombus score was graded from 0 to 5 after the passage of the guidewire, as described previously9.
CORONARY ANGIOGRAPHY
Coronary flow was graded using the standard Thrombolysis In Myocardial Infarction (TIMI) criteria10. Myocardial blush grade at the end of the procedure was evaluated according to van ’t Hof11. Angiographic no-reflow was defined as TIMI flow grade <3 and/or TIMI flow grade 3 with myocardial blush grade <2 at completion of the procedure. Two interventional cardiologists blinded to clinical and outcome parameters performed the angiographic analyses, and differences were resolved by consensus.
INVASIVE CORONARY PHYSIOLOGY MEASUREMENTS
Indices of coronary physiology of the infarct-related artery were assessed after flow restoration (before stenting) and/or at completion of PPCI. IMR was defined as the mean distal pressure multiplied by the mean transit time (Tmn) at hyperaemia as previously described1 using a coronary PressureWire™ (Abbott/St. Jude Medical, St. Paul, MN, USA). When measured before stent implantation, the IMR value was corrected for collateral flow by coronary wedge pressure (Pw), measured during prolonged balloon inflation, as follows:
CFRthermo was defined as the ratio of hyperaemic to resting coronary flow and was calculated using the equation:
PRESSURE-BOUNDED CORONARY FLOW RESERVE
The concept of pb-CFR has been proposed to estimate CFR applying a fundamental fluid dynamics equation that quantifies the pressure gradient induced across a lesion in an epicardial coronary vessel:
where ΔP is the pressure gradient across the lesion, Q is coronary flow, f is the friction coefficient and s is the separation coefficient. f and s are geometric and rheologic properties of the lesion and the vessel.
Pb-CFR assumes that, at one extreme, the lower bound of CFR is calculated as  , assuming that all the energy losses across the stenosis may be explained by separation forces and, on the other extreme, the upper CFR bound is calculated as the ratio between ΔP at hyperaemia and ΔP at rest, assuming that the energy losses may be due to friction across the lesion6. In other words, pb-CFR defines the interval between the minimum and the maximum possible CFR values as follows:
, assuming that all the energy losses across the stenosis may be explained by separation forces and, on the other extreme, the upper CFR bound is calculated as the ratio between ΔP at hyperaemia and ΔP at rest, assuming that the energy losses may be due to friction across the lesion6. In other words, pb-CFR defines the interval between the minimum and the maximum possible CFR values as follows:
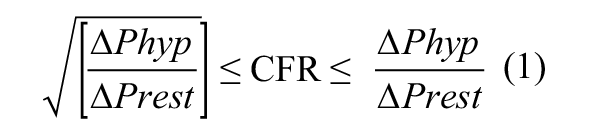
As reported by Ahn at al, the equation can also be rewritten as:
Since Pd/Pa was available in 100% of the cases we adopted equation (2) to derive pb-CFR (Supplementary Figure 1).
Pb-CFR was considered abnormal when both the upper and the lower bounds of pb-CFR were <2 and normal when both the upper and the lower bounds were >2. In all other cases, pb-CFR was considered indeterminate, as previously described6,8. Patients with resting Pd/Pa >0.98 were excluded from the analysis.
CARDIOVASCULAR MAGNETIC RESONANCE IMAGING PROTOCOL AND ANALYSIS
CMR was performed using a 3.0 Tesla magnetic resonance scanner (either MAGNETOM Trio™ or MAGNETOM® Verio; Siemens Healthcare, Erlangen, Germany) within 48 hours after PPCI and at six-month follow-up. The CMR protocol has been reported previously12 and is described in detail in Supplementary Appendix 1.
Cvi42 image analysis software (Circle Cardiovascular Imaging Inc., Calgary, Canada) was used for image analysis.
STATISTICAL ANALYSIS
Normally distributed variables are reported as mean±SD, and the Student’s t-test used for comparisons. Non-parametric distributions are reported as median (interquartile range), and the Mann-Whitney test used for unpaired data. Differences between groups were compared with one-way ANOVA or the Kruskal-Wallis test as appropriate. Fisher’s exact chi-square test was used for binary variables. Correlation between variables was tested by the Spearman-rho method.
Cohen’s kappa coefficient method and % agreement were used to assess the agreement between pb-CFR and CFRthermo. Receiver operating characteristic (ROC) curve analysis was used to test the diagnostic performance of physiological variables to predict the extent of microvascular dysfunction and myocardial injury after STEMI. In calculating ROC curves for IS, the cut-off value for the highest quartile was used to define the endpoint (IS% [48 hrs] ≥38.1% and IS% [6 months] ≥30.0%). Areas under the ROC curve were compared using the DeLong method.
In cases with repeated pre- and post-stent physiological assessment, the variations of IMR were measured using a non-parametric Wilcoxon test and variations in pb-CFR were assessed using McNemar’s test. Patients were classified as good responders or partial/poor responders to stenting according to the final IMR value ≥40 U, as described previously1.
For regression and ROC curve analysis, pb-CFR was used as a binary categorical variable in the analysis, excluding patients with indeterminate results.
Statistical analysis was performed using SPSS, Version 25.0 (IBM Corp., Armonk, NY, USA) and MedCalc statistical software, version 15.8 (MedCalc, Mariakerke, Belgium). All tests were two-tailed and a p-value <0.05 was considered statistically significant.
Results
One hundred and sixty-five patients presenting with STEMI underwent coronary physiological assessment of the infarct-related artery during PPCI as part of the OxAMI study. Pb-CFR was available in 148 patients (before and/or after PPCI) and was measured before stenting in 112 patients and at completion of PPCI in 123 patients. Eighty-seven (87) patients had both pre- and post-stenting pb-CFR data. CMR was available in all the cases (100%) at 48 hours and in 109 (74%) patients at six months of follow-up.
PB-CFR IN THE INFARCT-RELATED ARTERY BEFORE STENTING (IMMEDIATELY AFTER FLOW RESTORATION)
After flow restoration, pb-CFR was <2 in 89/112 (79.5%) patients, >2 in 5/112 (4.5%) patients and indeterminate in 18/112 (16.0%) patients (Supplementary Table 1).
No significant difference in CFRthermo was observed in patients stratified according to pb-CFR (Supplementary Table 2).
Notably, significant differences in pre-stenting IMR were observed stratifying the patients according to pb-CFR (Supplementary Table 2).
CORRELATION BETWEEN PRE-STENTING PB-CFR AND THE EXTENT OF MYOCARDIAL INJURY AFTER STEMI
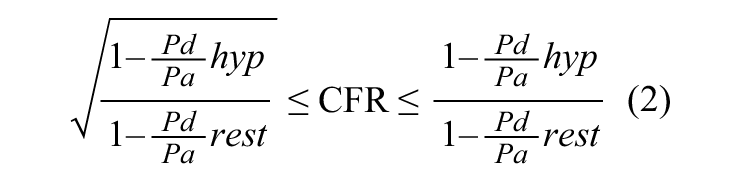
Pre-stenting pb-CFR >2 was associated with smaller myocardial area at risk percentage (AAR%) (Figure 1). Moreover, a trend towards smaller infarct size at 48 hours and six months was observed in patients with pre-stenting pb-CFR >2 (Figure 1, Supplementary Table 1).
Figure 1. Differences in IMR, MVO, myocardial AAR% and 48-hour IS% in patients stratified according to pre-stenting or post-stenting pb-CFR. A) Pre-stenting. B) Post-stenting, measured at completion of PPCI. *indicates overall p-value
At ROC curve analysis, pre-stenting pb-CFR demonstrated inferior but not statistically different diagnostic value compared to pre-stenting IMR in predicting the infarct size at 48 hours (AUCpb-CFR=0.53 [0.42-0.64] vs AUCIMR=0.63 [0.52-0.73], p=0.12), the final infarct size at six months (AUCpb-CFR=0.54 [0.42-0.67] vs AUCIMR=0.64 [0.52-0.76]; p=0.17) and the presence of intramyocardial haemorrhage (AUCpb-CFR=0.50 [0.32-0.68] vs AUCIMR=0.60 [0.41-0.77]; p=0.35). Moreover, the performance of pb-CFR in predicting the presence of MVO was inferior but marginally non-statistically different compared with IMR (AUCpb-CFR=0.52 [0.41-0.63] vs AUCIMR=0.64 [0.53-0.74], p for AUC comparison=0.052).
PB-CFR IN THE INFARCT-RELATED ARTERY AT COMPLETION OF PRIMARY PCI
At completion of PPCI, 86/123 (69.9%) patients presented a pb-CFR <2 and 11/123 (9.0%) patients had a pb-CFR >2. In the remaining 26/123 (21.1%) patients pb-CFR was indeterminate. Clinical, angiographic and imaging characteristics of patients stratified according to the post-PPCI pb-CFR are presented in Table 1 and Supplementary Table 3. Patients with pb-CFR >2 at completion of PPCI presented a trend towards a lower frequency of the left anterior descending (LAD) artery as the culprit vessel, higher TIMI flow post stenting and lower peak troponin levels.
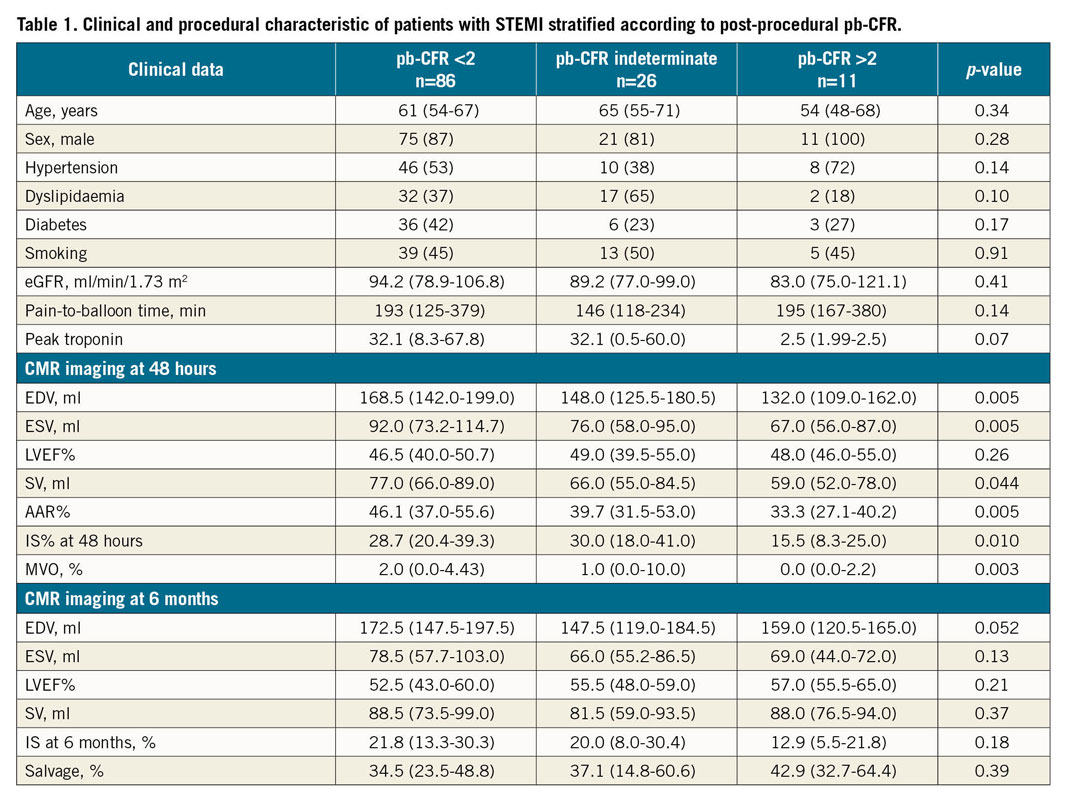
No significant difference was observed in CFRthermo across the pb-CFR groups (Table 2). Moreover, a poor agreement was observed between pb-CFR and CFRthermo (k=0.031, p=0.39; % agreement=65%) (Supplementary Figure 2).
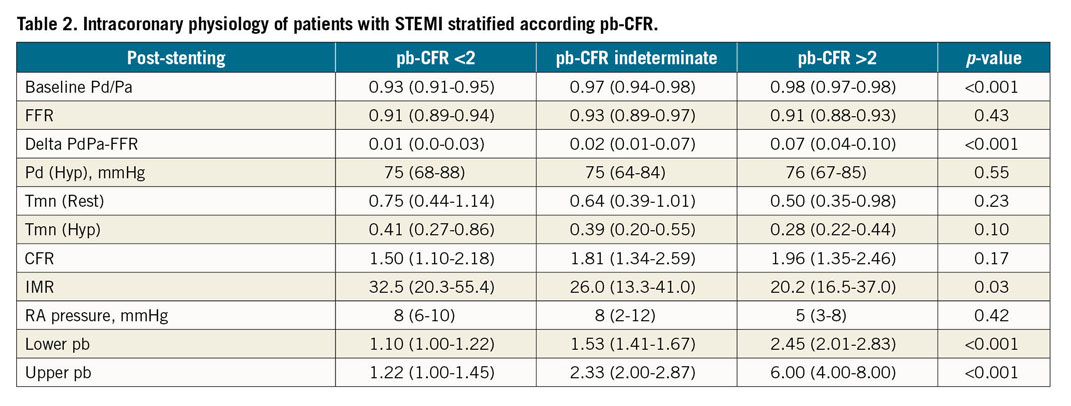
At completion of PPCI, IMR was significantly different across the pb-CFR groups, with pb-CFR >2 associated with lower IMR values (Table 2).
We found no interaction between binary pb-CFR and culprit vessel (p for interaction=0.601).
Significant variations were observed in IMR values before and after stenting (44.0 [28.4-80.0] to 28.7 [16.7-50.6], p<0.001). Notably, an overall improvement was observed in pb-CFR values at completion of PPCI (p<0.001) (Figure 2A, Supplementary Appendix 2). According to final IMR value <40 U, 54/87 (62%) patients were classified as good responders to stenting. In this subgroup, pb-CFR significantly improved at completion of PCI (p=0.007) (Figure 2B, Supplementary Appendix 2). Conversely, no significant variations in pb-CFR were observed in patients categorised as partial or poor responders to stenting according to final IMR ≥40 U (Figure 2C). Notably, good responders to stenting presented smaller IS% at 48 hours and six months, less MVO% and greater myocardial salvage compared with partial/poor responders to stenting (Supplementary Table 4, Supplementary Figure 3).
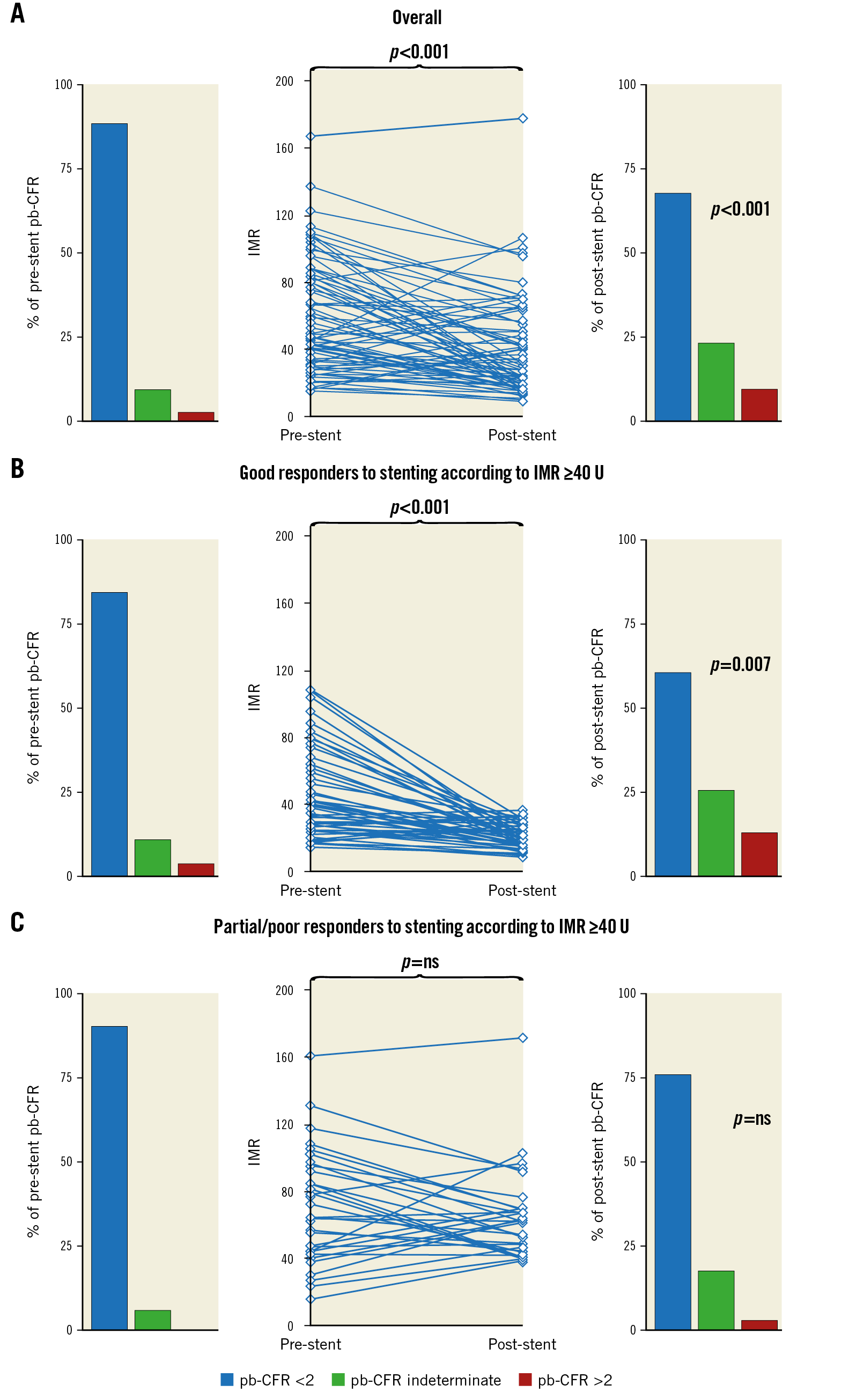
Figure 2. IMR and pb-CFR variations before and after stenting. Overall IMR and pb-CFR variations before and after stenting (panel A). Patients with both pre- and post-stenting physiological measurements were classified, according to the final IMR, as good responders to stenting (post-PPCI IMR <40 U) (panel B) or partial/poor responders (post-PPCI IMR ≥40 U) (panel C). Pb-CFR improved significantly in good responders but not in partial/poor responders to stenting.
CORRELATION BETWEEN PB-CFR AT COMPLETION OF PPCI AND THE EXTENT OF MYOCARDIAL INJURY AFTER STEMI
Post-PCI pb-CFR was significantly associated with the myocardial AAR% and the extent of myocardial injury at 48 hours after STEMI (Figure 1). A trend towards smaller infarct size at six months was observed in patients with pb-CFR >2. Notably, IMR and CFRthermo outperformed pb-CFR in predicting the extent of final IS (Table 3, Supplementary Table 5, Supplementary Table 6).
No significant differences were observed in the left ventricular ejection fraction (LVEF) across pb-CFR groups six months after STEMI (Figure 3).
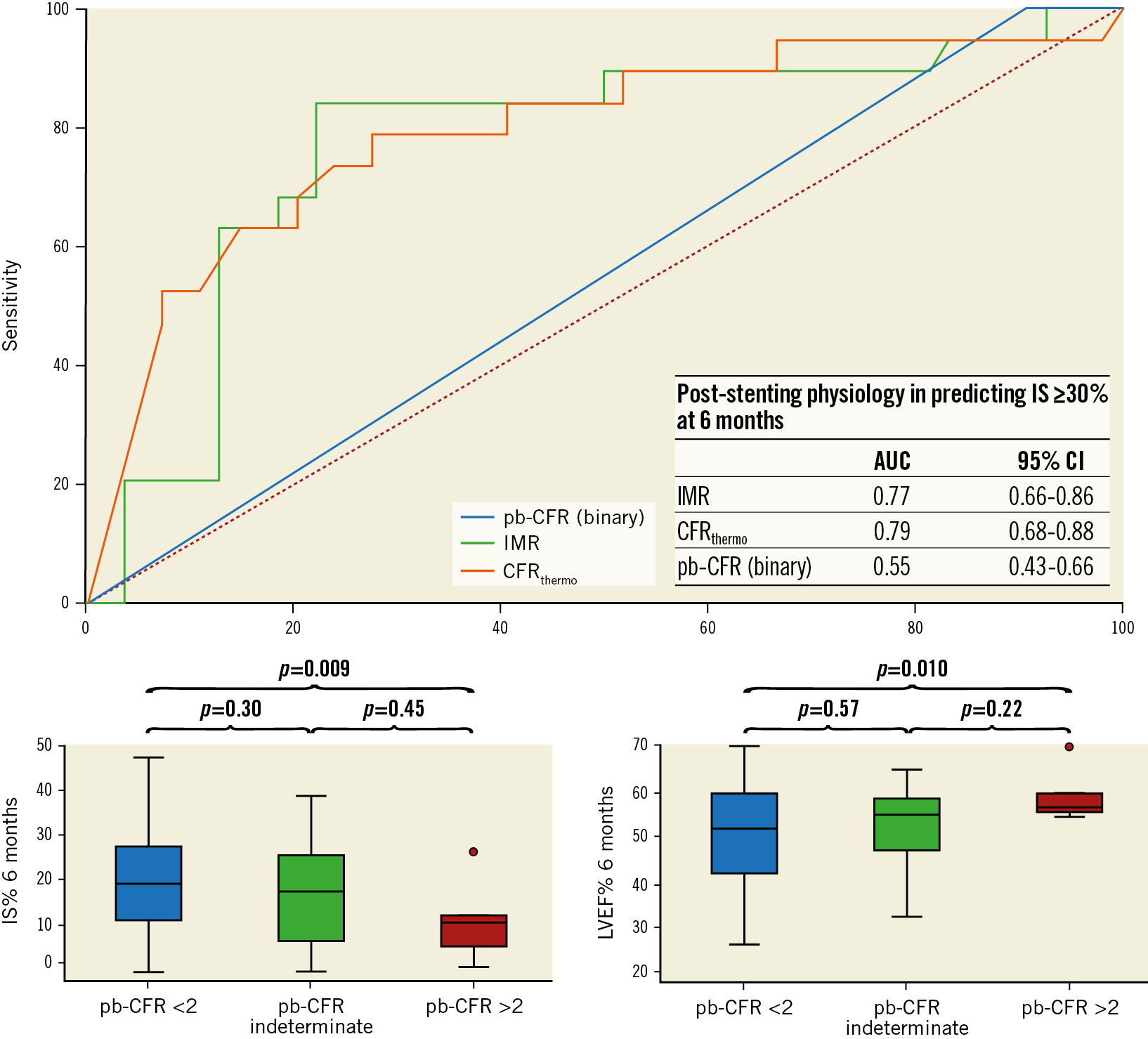
Figure 3. Diagnostic accuracy of physiological indices in predicting the final infarct size at six months after STEMI. IMR and CFRthermo presented a significantly higher AUC at ROC curve analysis compared with pb-CFR in predicting an IS ≥30.0% at CMR. In the lower panel, a trend towards smaller IS% at six months was observed for patients with post-PPCI pb-CFR >2. Conversely, no difference in left ventricular ejection fraction (LVEF%) was observed between the groups.
Post-PPCI pb-CFR was significantly associated with the presence of MVO (Table 1, Figure 1). Using regression analysis, pb-CFR outperformed CFRthermo in predicting the presence of MVO (OR=0.08; 95% CI: 0.02-0.42, p=0.003) (Table 3) but presented only modest diagnostic accuracy at ROC curve analysis (AUC=0.63 [0.52-0.73], p=0.003). Nonetheless, a pb-CFR >2 demonstrated high sensitivity (96.7% [88.5%-99.6%]) and fair negative predictive value (81.8% [48.2%-97.7%]) in excluding the presence of MVO.
Pb-CFR was inferior compared to IMR in predicting the presence of haemorrhage and the extent of IS% at 48 hours and six months (Table 3, Figure 3). Using alternative cut-offs other than 2 for pb-CFR (1.5 or 2.5) to define microvascular dysfunction did not improve the prognostic role of the index regarding CMR endpoints (Supplementary Table 7).
Discussion
Pb-CFR measured before and after stent placement has poor correlation with CFRthermo in this cohort of patients with STEMI undergoing PPCI. However, pb-CFR was associated with the extent of microvascular dysfunction assessed both in the catheterisation laboratory using IMR and with MVO measured using CMR. In particular, pb-CFR was able to identify a subgroup of patients (pb-CFR >2) who experienced better reperfusion after PPCI with lower IMR, MVO and smaller acute myocardial injury after STEMI.
Unfortunately, despite the advantage of being an easy technique based on a standard pressure wire without additional measurements of transit time or other coronary flow surrogates, pb-CFR is a suboptimal index of microvascular dysfunction in the STEMI population, with inferior diagnostic metrics compared with IMR.
Prompt restoration of coronary flow in the infarct-related artery by PPCI is the standard of care in patients presenting with STEMI. Nevertheless, a significant number of patients do not achieve complete myocardial reperfusion despite an apparently satisfactory angiographic result in the epicardial vessel1. This is mainly related to microvascular injury after PPCI and has been associated with larger infarct size, adverse LV remodelling and increased risk of heart failure and cardiovascular mortality3,12,13,14.
The identification of patients who are less likely to experience optimal reperfusion post PPCI and may be candidates to adjunctive or alternative therapeutic strategies is a field of ongoing research13. Coronary physiological indices, and specifically CFR and IMR, have been extensively investigated as potential tools to identify high-risk patients in the catheterisation laboratory. In particular, IMR has emerged as an accurate index of microvascular function with good predictive value for adverse outcome after STEMI15,16,17, as confirmed by this analysis (Figure 2, Supplementary Table 4).
However, the use of physiological assessment in STEMI is still limited because of the additional technical complexity, the additional procedural time and requirement for dedicated equipment to measure coronary flow using either Doppler or thermodilution techniques5.
Pb-CFR offers the advantage of avoiding thermodilution or Doppler velocity measurements and has been demonstrated to provide important information on the relationship between fractional flow reserve (FFR) and CFR6,8. However, Ahn et al showed that pb-CFR was not associated with clinical outcome in a large cohort of patients with stable coronary artery disease8. This result was recently confirmed by Wijntjens et al at long-term follow-up7.
The applicability of pb-CFR is also limited by the fact that it produces an indeterminate result (lower limit <2 and upper limit >2) in those cases that cannot be classified as normal (both limits >2) or abnormal (both limits <2)6,8. In our study, pb-CFR resulted in being “indeterminate” in 21.1% of the cases at completion of PPCI. Notably, the proportion of cases categorised as “indeterminate” is lower than that which has been observed by previous investigators6,7,8. It is of interest that this subgroup of patients presented intermediate-risk characteristics compared with the low and high CFR groups, with lower IMR values and smaller AAR% compared with patients with pb-CFR <2, but larger IS% compared with patients with pb-CFR >2.
In this study, pb-CFR measured in the infarct-related artery was impaired when measured post stenting in the majority of the cases (86/123=69.9%) and, consequently, the value of pb-CFR <2 in identifying cases with high IMR (>40 U) or MVO is limited. However, a lower limit pb-CFR >2 (normal pb-CFR) was significantly associated with lower IMR, smaller MVO and IS% at 48 hours and six months after STEMI.
Limitations
Our study has several limitations. This is a retrospective analysis of the OxAMI study and pb-CFR has been calculated using pre-existing recorded physiological data.
Another limitation of our study is the relatively small sample size and the fact that the prognostic value of pb-CFR has been tested against thermodilution-derived indices and CMR parameters and not against clinical endpoints. Nevertheless, this is the first study to explore the value of pb-CFR in predicting the extent of microvascular dysfunction and myocardial damage in the setting of STEMI patients.
An additional inherent limitation of pressure-derived CFR is the required minimum resting pressure gradient. In fact, in cases with small ΔP at rest, the measurement of pb-CFR might become inaccurate, as the value of √ΔP at rest is in the range of the error of the pressure measurement itself18,19. To overcome this limitation, we excluded those patients with a final resting Pd/Pa >0.98, as described previously. In our series, the overall mean Pd/Pa and FFR were 0.94±0.04 and 0.92±0.05, respectively, and, even in the subgroup of patients with post-PPCI pb-CFR >2, the resting and hyperaemic gradient across the lesion allowed a reliable measurement of pb-CFR (Table 2). Nonetheless, we cannot exclude some degree of inaccuracy in the measurement of post-PCI pb-CFR, especially in those cases with high FFR.
Conclusions
Pb-CFR is a pressure-only derived index of coronary flow reserve. In our study, pb-CFR was impaired (upper limit <2) in 70% of the cases at completion of PPCI and was modestly associated with the extent of microvascular dysfunction and myocardial injury after STEMI. Pb-CFR provided superior diagnostic performance compared to thermodilution-derived CFR in predicting MVO after STEMI. However, IMR was superior to both pb-CFR and thermodilution-derived CFR and, consequently, IMR was the most accurate in predicting all of the studied CMR endpoints of myocardial injury after PPCI.
|
Impact on daily practice Pressure-bounded coronary flow reserve (pb-CFR) is a simple tool to estimate CFR and is calculated using standard pressure-wire technology without the need for thermodilution or Doppler-velocity measurement. Pb-CFR is associated with the extent of microvascular dysfunction and myocardial injury in STEMI. In particular, patients with impaired pb-CFR have significantly higher IMR, MVO, area at risk and infarct size compared with patients with normal pb-CFR. However, pb-CFR is a suboptimal index of microvascular dysfunction in the STEMI population with inferior diagnostic metrics compared with IMR. |
Funding
This study was supported by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre, and by grants from the British Heart Foundation (BHF; CH/16/1/32013) and the Oxford BHF Centre of Research Excellence.
Appendix. Study collaborators
Alessandra Borlotti, PhD; Acute Vascular Imaging Centre, Radcliffe Department of Medicine, University of Oxford, Oxford, United Kingdom. Sam Dawkins, MD, PhD; Oxford Heart Centre, NIHR Biomedical Research Centre, Oxford University Hospitals, Oxford, United Kingdom.
Conflict of interest statement
R. Scarsini has received an education and training grant from EAPCI and served on an advisory board for Abbott. A. Banning has received institutional funding for an interventional fellowship from Boston Scientific. R. Kharbanda is a proctor for Boston Scientific and has received speaker fees from Abbott. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.