
Abstract
Aims: The Oxford Acute Myocardial Infarction PICSO (OxAMI-PICSO) study aimed to assess the efficacy of index of microcirculatory resistance (IMR)-guided therapy with pressure-controlled intermittent coronary sinus occlusion (PICSO) in anterior ST-elevation myocardial infarction (STEMI).
Methods and results: Patients with anterior STEMI treated with primary percutaneous coronary intervention (pPCI) were enrolled. Pre-stenting IMR was measured and PICSO treatment delivered if pre-stenting IMR was >40. No PICSO treatment was considered in patients with a pre-stenting IMR ≤40. The control group was derived from a historical cohort of STEMI patients with pre-stenting IMR >40 enrolled in the observational OxAMI study. IMR was measured after completion of pPCI in all patients and within 48 hours in PICSO patients and controls. Cardiac magnetic resonance imaging was performed per protocol for infarct size (IS) assessment within 48 hours after pPCI and at six months. A total of 105 patients were enrolled (25 PICSO, 50 controls with pre-stenting IMR >40, 30 with pre-stenting IMR ≤40). Compared to controls, patients treated with PICSO had a lower IMR at 24-48 hours (24.8 [18.5-35.9] vs. 45.0 [32.0-51.3], p<0.001) and lower IS at six months (26.0% [20.2-30.0] vs. 33.0% [28.0-37.0], p=0.006).
Conclusions: An IMR-guided treatment with PICSO in anterior STEMI is feasible and may be associated with reduced IS and improved microvascular function.
Abbreviations
AAR: area at risk
ATI: age – thrombus burden – index of microcirculatory resistance
AUC: area under the curve
cMRI: cardiac magnetic resonance imaging
CS: coronary sinus
IMR: index of microcirculatory resistance
IRA: infarct-related artery
IS: infarct size
LGE: late gadolinium enhancement
MBG: myocardial blush grade
MSI: myocardial salvage index
MVO: microvascular obstruction
OxAMI: Oxford Acute Myocardial Infarction
PICSO: pressure-controlled intermittent coronary sinus occlusion
pPCI: primary percutaneous coronary intervention
STEMI: ST-elevation myocardial infarction
TIMI: Thrombolysis In Myocardial Infarction
Introduction
Prompt restoration of coronary blood flow of the infarct-related artery (IRA) by primary percutaneous coronary intervention (pPCI) is the current gold standard treatment for patients with ST-elevation myocardial infarction (STEMI)1. However, the conventional revascularisation strategy, combining coronary stenting with state-of-the-art antithrombotic and antiplatelet therapy, can still be associated with a poor clinical outcome in some patients.
These patients, accounting for up to 40% of cases, have evidence of no reflow, a condition related to severe post-procedural coronary microvascular injury2. Consequently, to improve the outcomes in STEMI patients, it is desirable to identify as early as possible patients likely to have a suboptimal result with a conventional revascularisation strategy and then consider them for additional or alternative therapies.
The index of microcirculatory resistance (IMR) is a pressure wire-derived parameter assessing the functional status of the coronary microcirculation. It has been used in STEMI patients and demonstrates a significant association with microvascular injury and long-term clinical outcome3. Notably, recent evidence supports its feasibility to assess the degree of coronary microvascular impairment before proceeding to stenting2. In this regard, it has been shown that a pre-stenting IMR greater than 40 units can at an early stage identify, alone or in combination with other clinical variables, high-risk STEMI patients who could benefit from additional therapeutic strategies in addition to conventional stenting4,5.
Pressure-controlled intermittent coronary sinus occlusion (PICSO®) (Miracor Medical SA, Awans, Belgium) is a therapeutic strategy proposed for STEMI patients. PICSO consists of a balloon-tipped catheter which is placed in the coronary sinus (CS). The balloon inflates and deflates cyclically leading to an intermittent CS pressure increase, which could lead to an improved perfusion of the ischaemic area mainly by redistributing blood flow from the remote myocardium to the infarcted area6.
The Oxford Acute Myocardial Infarction – Pressure-controlled Intermittent Coronary Sinus Occlusion (OxAMI-PICSO) study (NCT03473015) aimed to assess the feasibility of an IMR-guided PICSO strategy in a high-risk cohort of patients with anterior STEMI, selected using a pre-stenting procedural IMR >40.
Methods
STUDY DESIGN
OxAMI-PICSO is a single-centre, investigator-initiated study, prospectively enrolling patients with anterior STEMI admitted for pPCI at the Oxford Heart Centre from August 2015 to September 2017. The study protocol was approved by the local ethics committee (REC 15/SC0167) and conducted in accordance with the Declaration of Helsinki.
Main inclusion criteria were clinical presentation for PCI with stenting for anterior STEMI and left anterior descending artery as the clear culprit vessel. Main exclusion criteria were previous STEMI, previous coronary artery bypass grafting, and presentation with cardiogenic shock. A full list of inclusion and exclusion criteria can be found in Supplementary Appendix 1. Figure 1 summarises the study design.
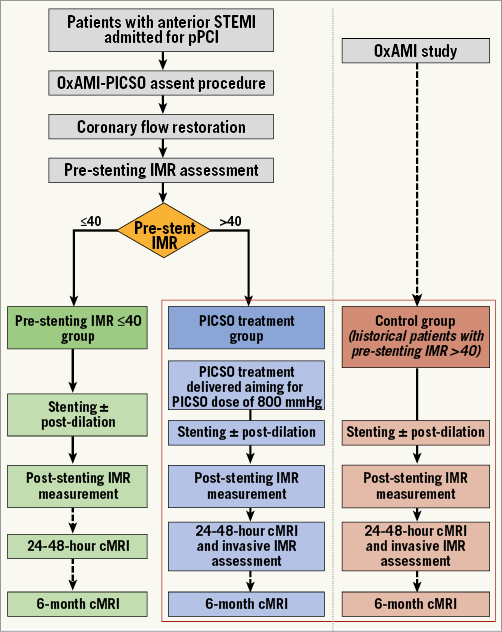
Figure 1. OxAMI-PICSO study design. cMRI: cardiac magnetic resonance imaging; IMR: index of microcirculatory resistance; OxAMI: Oxford Acute Myocardial Infarction; PICSO: pressure-controlled intermittent coronary sinus occlusion; pPCI: primary percutaneous coronary intervention; STEMI: ST-elevation myocardial infarction
After verbal assent to take part in the study and following prompt restoration of flow in the infarct-related artery (IRA), via balloon predilation plus/minus thrombus aspiration, IMR was measured before proceeding to stenting. Patients with a pre-stenting IMR >40 were formally considered for inclusion in the OxAMI-PICSO study and, if still in agreement, were treated with PICSO before proceeding to stenting. At the end of the procedure, IMR was remeasured. After full written informed consent, patients were considered for cardiac magnetic resonance imaging (cMRI) and for a second assessment of IMR within 48 hours from the index procedure. A second cMRI scan was scheduled at six-month follow-up.
Patients with a pre-stenting IMR ≤40 units and patients with an IMR >40 unwilling to be treated with PICSO or in case of PICSO unavailability were enrolled in the parallel running observational Oxford Acute Myocardial Infarction (OxAMI) study (REC 10/H0408/24)2. As in OxAMI-PICSO, also in the OxAMI study, IMR is measured in all patients at completion of pPCI and within 48 hours from the index procedure if the pre-stenting IMR is >40. Similarly, cMRI is performed within 48 hours and at six-month follow-up.
Notably, between December 2015 and September 2016, all anterior STEMI had to be enrolled solely in the OxAMI study, since recruitment to OxAMI-PICSO had to be provisionally paused. This was due to an expired CE mark on the device, requiring a new submission to the local ethics committee for approval, which ultimately allowed resumption of recruitment into the OxAMI-PICSO study.
pPCI was performed according to international guidelines in all patients. Decisions about thrombectomy, glycoprotein IIb/IIIa inhibitor adoption and post-dilation were all left to the operators’ discretion.
DEFINITION OF GROUPS
According to pre-stenting IMR and PICSO therapy, three groups of patients were ultimately considered: 1) patients with a pre-stenting IMR >40 treated with PICSO, 2) controls with a pre-stenting IMR >40 not treated with PICSO (formally enrolled in the OxAMI study), 3) patients with a pre-stenting IMR ≤40 not treated with PICSO (formally enrolled in the OxAMI study).
INDEX OF MICROCIRCULATORY RESISTANCE
IMR was measured using the thermodilution technique as previously described and was calculated as distal pressure at hyperaemia multiplied by mean transit time at hyperaemia (Supplementary Appendix 2)2.
PRESSURE-CONTROLLED INTERMITTENT CORONARY SINUS OCCLUSION
The PICSOAMI Impulse System consists of the PICSOAMI Impulse Console and PICSO Impulse Catheter (all Miracor Medical). The PICSO Impulse Catheter is an 8 Fr triple-lumen catheter with a low-profile, semi-compliant balloon at the tip. The catheter is placed in the coronary sinus over a 0.032-inch wire by a 10 Fr pre-shaped delivery long steerable sheath (Destino™ Steerable Sheath DS856750/22; Oscor Inc., Palm Harbour, FL, USA) inserted via the femoral vein.
A PICSO dose of 800 mmHg has previously been related with a positive trend for improved myocardial recovery7. For this reason, in the OxAMI-PICSO study, PICSO treatment was delivered to patients, if tolerated, until a minimum PICSO dose of 800 mmHg was achieved.
CARDIAC MAGNETIC RESONANCE IMAGING
cMRI scans were performed within two days after pPCI and at six months using a 3.0 Tesla scanner (either MAGNETOM® Trio Tim® or MAGNETOM® Verio; Siemens Healthcare, Erlangen, Germany). The following parameters were assessed: left ventricular end-diastolic volume, end-systolic volume, ejection fraction, area at risk (AAR), infarct size (IS), myocardial salvage index (MSI), microvascular obstruction (MVO), intramyocardial haemorrhage and IS shrinkage (Supplementary Appendix 3).
STATISTICAL ANALYSIS
Continuous variables were expressed as mean and (±) standard deviation (SD) or as median accompanied by interquartile range (IQR), as appropriate, after checking for normality using the Shapiro-Wilk test. Frequencies were compared using the chi-square test or Fisher’s exact test, as appropriate. Normally distributed continuous variables were compared using the t-test or analysis of variance (ANOVA) with Bonferroni’s post hoc comparisons, as appropriate, whilst non-normally distributed continuous variables were compared using the Mann-Whitney test or Kruskal-Wallis test, as appropriate.
To assess the effect of PICSO on IMR and IS over time in patients with elevated pre-stenting IMR, a mixed design ANOVA model was used after controlling for sphericity with Mauchly’s test of sphericity and for equality of error variances with Levene’s test.
Finally, in patients with a pre-stenting IMR >40, a binary logistic regression model was used to calculate the odds ratio (OR) for predictors of IMR >40 at 24-48 hours and IS >24% at six months8. In both models, besides PICSO treatment, age – thrombus burden – index of microcirculatory resistance (ATI) score, TIMI flow 0 at presentation, ischaemic time, abciximab and bivalirudin adoption were included as covariates.
All statistical analyses were performed using SPSS, Version 24.0 (IBM Corp., Armonk, NY, USA) and a p-value <0.05 was considered statistically significant.
Results
CLINICAL AND PROCEDURAL CHARACTERISTICS
The patient flow chart is displayed in Supplementary Figure 1. A total of 105 patients were ultimately enrolled and distributed as follows: 25 patients with a pre-stenting IMR >40 formally enrolled in the OxAMI-PICSO study and successfully treated with PICSO; 50 control patients with a pre-stenting IMR >40 not treated with PICSO and enrolled in the OxAMI study; 30 patients with pre-stenting IMR ≤40 not treated with PICSO and enrolled in the OxAMI study.
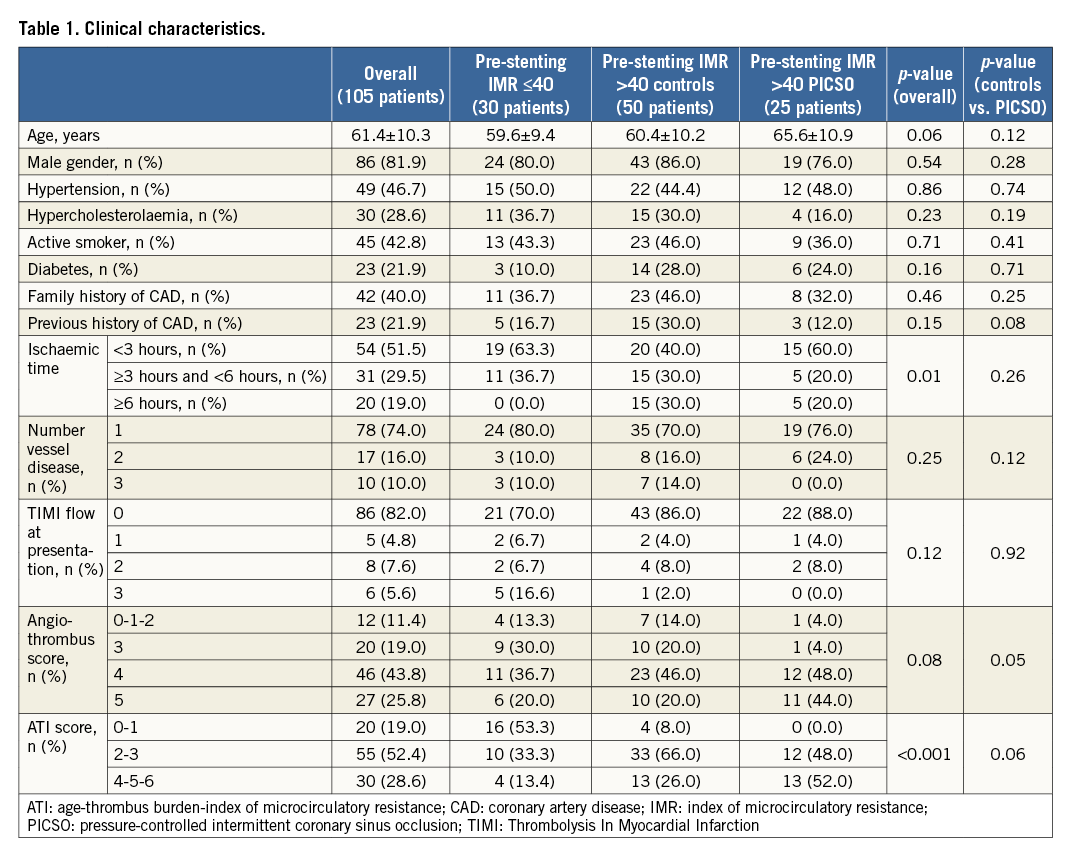
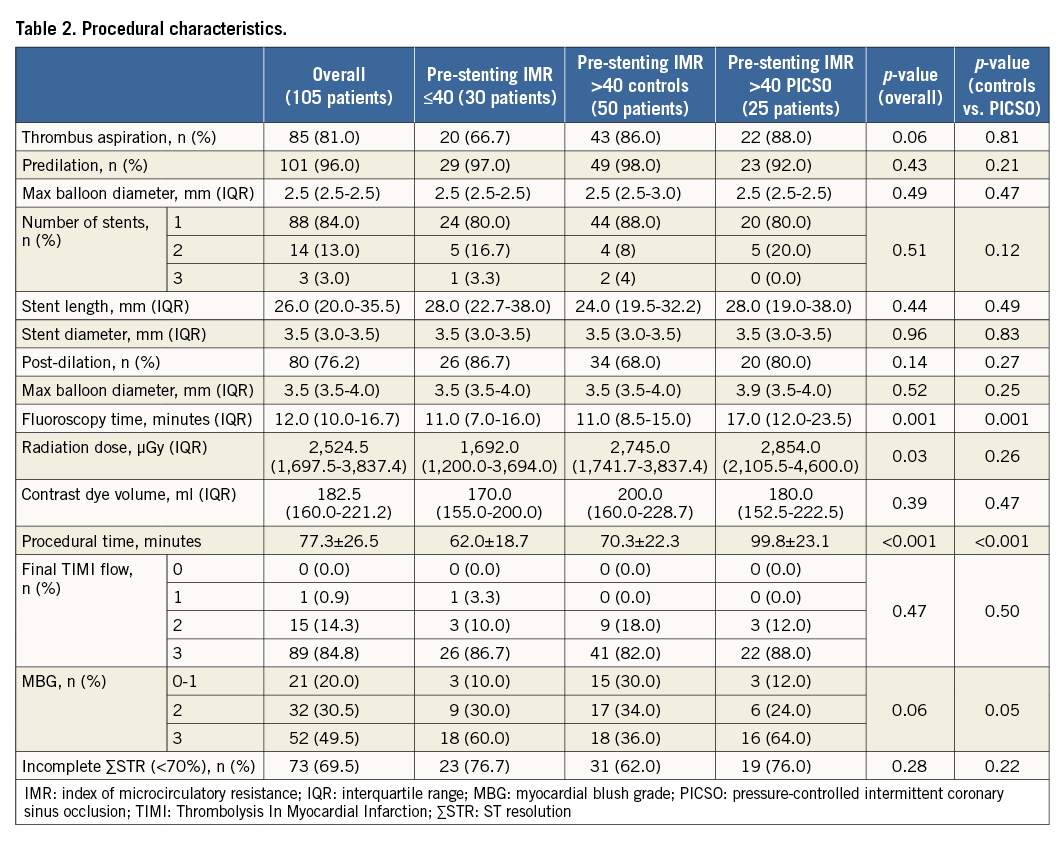
Clinical and procedural characteristics are reported in Table 1, Table 2, and Supplementary Table 1, and stratified according to the three main groups.
PICSO treatment was successfully delivered in 25 patients with only two cases in which PICSO therapy could not be delivered because of technical issues (kinking in the pneumatic tubes for helium shuttling). PICSO treatment was associated with longer procedural and fluoroscopic times, but not with larger volume of contrast dye or radiation dose (Table 2). The prolonged procedural time can be ascribed mainly to the time required to deliver the target PICSO dose of 800 mmHg (33.0±10.6 minutes) rather than to the time needed to insert the device in the CS (15.0 minutes [8.5-22.5]) (Supplementary Table 2).
No device-related complications and no clinical events were reported throughout the duration of the study.
EFFECT OF PICSO ON IMR
Pre- and post-stenting IMR were available in all 105 patients. Notably, no significant difference was observed in pre-stenting IMR values between PICSO patients and controls with an initial IMR >40 (p=0.40) (Supplementary Table 3, Figure 2). After stenting, IMR was not statistically different between PICSO patients and controls with an initial IMR >40 (p=0.40). Conversely, patients with a pre-stenting IMR ≤40 had a significantly lower IMR after stenting compared to both PICSO patients (p=0.002) and controls with an initial pre-stenting IMR >40 (p<0.001) (Supplementary Table 3, Figure 2).
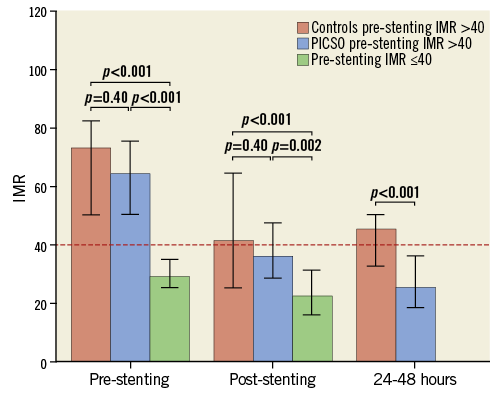
Figure 2. Effect of PICSO treatment on IMR. Graph shows trend over time of IMR in the three groups of patients. Dotted red line highlights the threshold of 40 units for IMR. Data are reported as median, error bars represent interquartile range. IMR: index of microcirculatory resistance; PICSO: pressure-controlled intermittent coronary sinus occlusion
IMR was reassessed after 24-48 hours post pPCI in 20/25 PICSO patients and in 31/50 controls with a pre-stenting IMR >40. Interval time from index procedure to IMR reassessment did not differ between PICSO and controls (27.3±5.3 hours vs. 25.9±4.3 hours, p=0.30). Notably, IMR measured after 24-48 hours was significantly lower in PICSO patients compared to controls (24.8 [18.5-35.9] vs. 45.0 [32.0-51.3], p<0.001), with a smaller proportion of patients in the PICSO group presenting an IMR >40 after 24-48 hours from the index procedure (10.0% vs. 64.5%, p<0.001).
These findings were further confirmed by the mixed design ANOVA model showing an overall significant effect of time on IMR reduction in both PICSO patients and controls (p-value for time effect <0.001). More importantly, both PICSO (p-value for PICSO effect=0.004) and PICSO-time interaction (p-value for interaction=0.002) had a significant effect on IMR values (Supplementary Figure 2, Supplementary Figure 3).
No correlation was observed between PICSO dose and IMR (Supplementary Figure 4).
EFFECT OF PICSO ON ACUTE INFARCT SIZE AND MICROVASCULAR OBSTRUCTION
An acute cMRI scan within 48 hours was performed on 63/105 patients (time from pPCI to scan 31.2±11.1 hours) (Supplementary Table 4). Patients with a pre-stenting IMR ≤40 had a significantly lower IS and less evidence of MVO and intramyocardial haemorrhage (overall p<0.001, p=0.002 and p=0.004, respectively).
Acutely, compared to controls with a pre-stenting IMR >40, PICSO patients had a similar extent of area at risk (AAR) (p=0.21), IS (p=0.42), MVO occurrence (p=0.08), MVO extent (p=0.36), intramyocardial haemorrhage occurrence (p=0.12) and extent (p=0.36) (Supplementary Table 4). A similar trend was observed when IS was assessed using peak troponin I and troponin I area under the curve (AUC) (Supplementary Figure 5).
EFFECT OF PICSO ON FINAL INFARCT SIZE
A follow-up cMRI scan at six months was performed in 54/105 patients (time from pPCI to scan 190.9±39.0 days). A total of nine patients with initially acute cMRI missed the follow-up cMRI scan (Supplementary Table 4).
Compared to untreated controls, patients treated with PICSO presented a significantly smaller IS (26.0% [20.2-30.0] vs. 33.0% [28.0-37.0], p=0.006) (Supplementary Table 4, Figure 3). Notably, IS did not differ between PICSO patients and patients with an initial pre-stenting IMR ≤40 (p=0.11) (Supplementary Table 4, Figure 3).
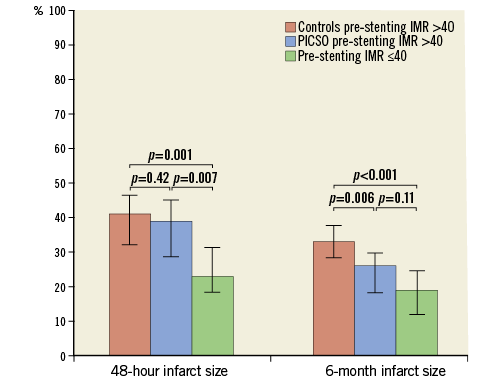
Figure 3. Effect of PICSO treatment on infarct size. Graph shows trends of IS in the three groups of patients. Data are reported as median, error bars represent interquartile range. IS: infarct size; PICSO: pressure-controlled intermittent coronary sinus occlusion
These findings were further confirmed in the mixed design ANOVA model, showing a significant effect of time (p-value for time effect <0.001) and PICSO treatment (p-value for PICSO=0.01) on IS (Supplementary Figure 6).
No correlation was observed between PICSO dose and IS (Supplementary Figure 7).
PREDICTORS OF 24-48 HOUR IMR AND FOLLOW-UP INFARCT SIZE
In patients with an elevated pre-stenting IMR, PICSO treatment was the only parameter significantly and inversely associated with an IMR >40 at 24-48 hours (OR 0.10, 95% CI: 0.02-0.56, p=0.009, model R2=0.35) and with an IS >24% at six months (OR 0.24, 95% CI: 0.10-0.98, p=0.04, model R2=0.27) (Figure 4).
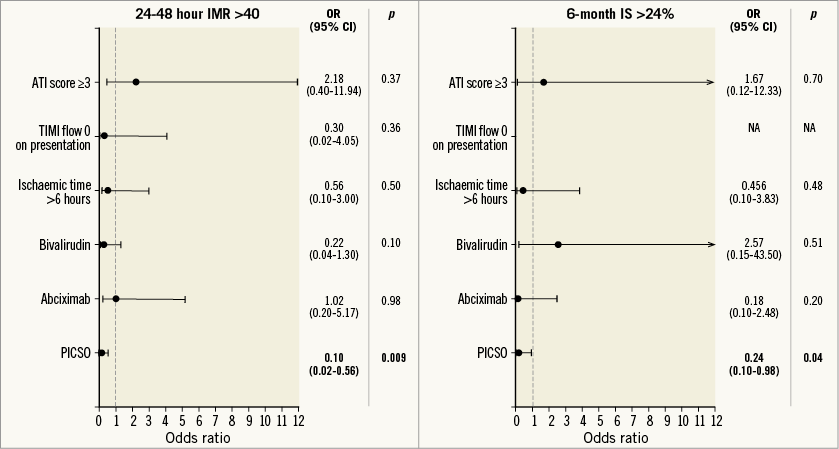
Figure 4. Predictors of IMR >40 at 24-48 hours and of IS >25% at six-month follow-up. The forest plot shows the results of the binary logistic multivariable models for prediction of final IMR and IS. (Graph shows odds ratio and 95% confidence interval for each covariate).
Discussion
Prompt restoration of patency of the IRA by pPCI with stenting has improved the outcome of most STEMI patients. However, suboptimal myocardial reperfusion secondary to no reflow is still observed in up to 40% of cases, with significant implications for long-term prognosis. In order to prove a benefit of novel/additional therapies beyond conventional stenting, early identification of that minority of patients at risk of suboptimal reperfusion is crucial.
In this study, the feasibility of a pre-stenting IMR-based approach to guide novel/additional treatment has been tested and prospectively validated. We observed that patients with a pre-stenting IMR ≤40 treated with conventional pPCI had a good outcome in terms of IMR and cMRI findings. This confirms that these patients were unlikely to benefit from further additional treatment and it allowed a targeted approach to the two thirds of patients with anterior STEMI who were potentially eligible.
With this premise, it was possible to apply pre-stenting IMR to assess the feasibility of PICSO therapy. PICSO is a device for the treatment of STEMI patients with a mode of action of intermittent and cyclical occlusion of the CS. Its efficacy in reducing IS has been shown in animal models and at least three mechanisms have been proposed to explain such an effect: 1) redistribution of blood flow from the remote myocardium to the border zone of the ischaemic myocardium; 2) enhanced washout of noxious, inflammatory factors and embolic material from the microvascular bed (suction effect upon balloon release); 3) improvement in collaterals through release of vascular growth factors as a consequence of venous pressure increase6.
The OxAMI-PICSO study confirms the feasibility of PICSO, extending the initial preliminary results of the Prepare PICSO and Prepare RAMSES studies7,9. No PICSO-related complications were reported and PICSO therapy was delivered in the vast majority of enrolled patients. PICSO treatment was associated with prolonged procedural time, mainly related to the time required to achieve 800 mmHg of dose rather than additional time needed to deliver PICSO into the CS. This confirms the utility of an IMR-guided approach, restricting the PICSO-related prolonged procedural time to only those patients with the highest chance of benefit.
The study shows that IMR-guided and targeted application of PICSO is associated with an early improvement of coronary microvascular function. Whilst IMR was reported to improve over time in all patients, confirming previous evidence about progressive microvascular function recovery over time10, PICSO appeared to accelerate such recovery, with significantly lower IMR at 24-48 hours in PICSO patients.
The benefit of an IMR-guided application of PICSO was confirmed also by cMRI findings. Even though starting from similar IS acutely, PICSO patients had a significantly smaller IS at six months compared to controls. Importantly, high-risk patients treated with PICSO presented an IS extent at six months similar to that observed in low-risk patients with pre-stenting IMR ≤40, demonstrating the potential impact of a targeted application of PICSO therapy. These findings might seem in contrast with those reported in the Prepare RAMSES study, which failed to detect a significant effect of PICSO on IS. However, the unselected inclusion of low-risk patients (40% presented TIMI flow >1 on admission), failure in delivering PICSO treatment in one third of cases, and the PICSO treatment delivered entirely after stenting7 may account for the contrasting results.
In our study, a positive effect of PICSO on IS was not detected acutely. Two possible mechanisms may explain this potential discrepancy. Firstly, the very early timing for the first cMRI scan should be acknowledged. At 24-48 hours it has been shown that late gadolinium enhancement tends to overestimate the actual IS. This might have affected the ability to detect a significant difference in IS between PICSO and controls acutely11.
Secondly, the preserved microvascular function observed in PICSO patients may reflect the fact that, even though both PICSO patients and controls started with similar “anatomical IS” and “anatomical extent of MVO”, those treated with PICSO ended up having a smaller IS at six months because of the positive effect of PICSO on coronary microvascular function, reflected by a lower IMR.
Limitations
Firstly, OxAMI-PICSO was a non-randomised study using, as control, patients with available pre-stenting IMR measurement enrolled in the parallel OxAMI study. Even though a propensity score matching could have overcome such a limitation, an analysis on the overall cohorts was preferred in order to maintain a reasonable sample size and statistical power. Such a choice was further justified by the observation that no significant differences in clinical characteristics were reported between PICSO patients and controls. Additionally, the effect of PICSO on outcome measures was confirmed in the multivariable models adjusting for potential confounding variables.
A second limitation is the number of patients without cMRI. This is a common finding in an emergency all-comers design but, while cMRI within 24-48 hours was performed in only 60% of the study population, most of these patients completed follow-up with cMRI at six months (85.7%). This is not a trivial achievement considering the highly demanding design of the study. Additionally, the mixed model ANOVA worked as a sensitivity analysis, confirming the main result of the study.
Thirdly, OxAMI-PICSO did not use the age – thrombus score – index of microcirculatory resistance (ATI) score4 to select high-risk STEMI patients, since it was not yet validated at the time of study design. However, the ATI score was not different between PICSO patients and controls, with PICSO patients presenting a slightly higher risk profile compared to controls (ATI score >3 in 52% of cases vs. 26%, p=0.06).
Conclusions
This study has contributed to further validation of pre-stenting IMR as an early triaging tool for novel/additional treatment in STEMI, showing the ability of PICSO to improve microvascular function and reduce IS in selected high-risk STEMI patients. Because of the design of the study, these results need to be interpreted as hypothesis-generating and warrant further validation in a large randomised clinical trial.
| Impact on daily practice The OxAMI-PICSO study has prospectively shown the feasibility of preprocedural IMR to guide the application of additional treatment options in STEMI patients. This strategy has helped to show, in a non-randomised environment, the potential benefit of PICSO treatment in selected anterior STEMI. |
Funding
Miracor Medical SA supported the OxAMI-PICSO study supplying the PICSO Impulse Console and catheters and partially financing the costs for pressure wires and cMRI. The OxAMI study is supported by the British Heart Foundation (grant CH/16/1/32013), the BHF Centre of Research Excellence, Oxford (RG/13/1/30181), and the National Institute for Health Research Oxford Biomedical Research Centre.
Conflict of interest statement
A. Banning has received an unrestricted research grant to his institution from Boston Scientific to fund an interventional fellowship. The other authors have no conflicts of interest to declare.
Supplementary data
Supplementary Appendix 1. OxAMI-PICSO study inclusion and exclusion criteria.
Supplementary Appendix 2. Measurement of index of microcirculatory resistance (IMR).
Supplementary Appendix 3. Cardiac magnetic resonance imaging.
Supplementary Figure 1. Patient flow chart.
Supplementary Figure 2. Change in IMR at 24 hours.
Supplementary Figure 3. Temporal trend of IMR in patients with pre-stenting IMR >40.
Supplementary Figure 4. Effect of PICSO dose on IMR.
Supplementary Figure 5. Effect of PICSO treatment on peak troponin I levels and AUC troponin.
Supplementary Figure 6. Temporal trend of IS in patients with pre-stenting IMR >40.
Supplementary Figure 7. Effect of PICSO dose on IS.
Supplementary Table 1. Medical management in OxAMI-PICSO study.
Supplementary Table 2. PICSO procedural details.
Supplementary Table 3. Invasive coronary physiology parameters.
Supplementary Table 4. Cardiac magnetic resonance imaging parameters.
To read the full content of this article, please download the PDF.

