The dogma “time is muscle”, with a timely reperfusion of acutely occluded coronary arteries, has salvaged myocardium, reduced mortality and prevented crippling consequences in patients with acute coronary syndromes (ACS)1. Very early on, the adverse effects of a sudden uncontrolled reperfusion with an increase in oxygen, pressure and temperature of reflowing blood into previously ischaemic areas were recognised2, later being characterised as ischaemia-reperfusion injury3. Recently, in this journal, the existence of incomplete recovery, underlying pathophysiology of reperfusion and clinical consequences of microcirculatory obstruction was elegantly debated4. Importantly, after myocardial infarction, regional myocardial dysfunction is in part due to a global increase of myocardial impedance and circulating microparticles, thus reducing myocardial and consequently venous flow5 including cardiac vein flow and has been established as a prognostic parameter for patient survival6. Obviously, cardiac veins are an integral part in the process of microvascular obstruction, and washout of debris and toxic accumulations is essential to the healing process7. Recently, in this journal, De Maria et al8 described a substantial reduction of microvascular resistance by pressure controlled intermittent coronary sinus occlusion (PICSO). PICSO has shown potential to salvage ischaemic myocardium and has been associated with inducing the expression of vasoactive substances including adenosine9.
The origins of the transcoronary sinus interventions, such as PICSO, can be traced back to the surgical Beck’s procedure that arterialised the coronary venous vasculature10. After we developed the concept of PICSO in the early 1980s, several well-known individuals in cardiology and cardiac surgery including Alice Jacobs, Dave Faxon, Sam Meerbaum, Eliot Corday, Harold Lazar, Wolfgang Schreiner and Friedl Neumann, among many others, investigated this procedure. The results were published in a series of symposia11-14. One of the important features of this intervention is the retrograde access to deprived microcirculation, allowing optimal performance of haemoglobin puffer systems, restoration of basic nutrition to damaged cells and washout of obstructing thrombi from the microcirculation. Occluding venous outflow temporarily redistributes venous flow from normal perfused areas towards the deprived zones. Systolic pressure increase in the venous compartment creates plasma skimming in the venous microcirculation, since blood density increases in larger veins, perfusion of venules with plasma increases and reaches the microcirculation predominantly in the occluded artery territory. Plasma skimming seems to be one of the central actions of this procedure, elegantly described by Kenner and Moser using continuous haematocrit measurements in the coronary circulation15. This increase in pressure has been documented by a pressure increase in the occluded epicardial artery (Figure 1A)15. Upon sudden release of the occlusion, a rapid decline in venous pressure and a concomitant fall in blood density removes excessive myocardial water and even thrombotic debris from the microcirculation (Figure 1B). Repetitive occlusion release cycling of PICSO creates a net washout effect, reducing the water content of the myocardium. A bimodal appearance of myocardial oedema in the reperfused heart and a second peak of enzyme release as a reaction to sudden reperfusion has been shown in experiments mimicking acute coronary syndromes, as well as after global cardiac arrest in cardiac surgical patients16,17. Although the concept of bimodal oedema waves has been criticised by Berry et al18, our group also found a second wave of injury after elective global cardiac arrest in cardiosurgical patients16. Theoretically, manipulating the oedema formation process may also influence interpretation of myocardial salvage in clinical trials. Consequently, any intervention modifying the primary area at risk, and eventually also the second reactive peak to reperfusion, changes measurements during early MRI studies.
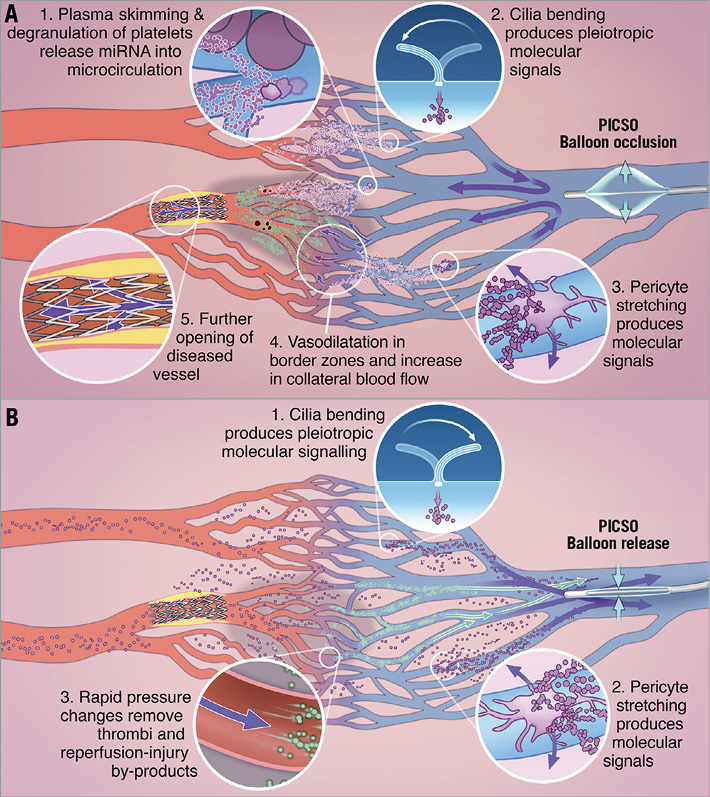
Figure 1. Schematic depiction of coronary circulation during ACS and effects of PICSO, depicting redistribution of flow to deprived myocardium, and washout, but also the effects on plasma skimming and the proposed release of regenerative molecules, via the well-described process of mechanotransduction. A) Balloon inflated in the coronary sinus. 1) Plasma skimming: plasma enters the microcirculation whereas cells remain in larger veins, platelets are degranulated and release miRNA into the circulation which is retroperfused into the myocardium15. 2) & 3) Primary cilia in vascular cells are moved by flow currents, pericytes are temporarily stretched and release pleiotropic molecular signals via mechanotransduction26,27. 4) Flow in border zones improves due to vasodilation and increases collateral flow9. 5) Pressure increases in occluded coronary arteries and rapid changes in pressure induce washout of debris from the occlusion site and dependent microcirculation, thus improving flow via culprit lesions towards deprived myocardium11. B) Balloon released. 1) & 2) Cilia bending and pericyte stretching as described above. 3) Microcirculation emptying caused by rapid pressure change and removal of thrombi and reperfusion injury by-products.
Every day cardiac surgeons are confronted with reperfusion injury after global cardiac arrest. Reducing post-ischaemic damage by temporary modification of the reperfusate, including calcium, potassium, pH, and osmolarity, was reported in the cardiosurgical literature as early as 1981, leading to widespread application of cardioplegia, reducing ischaemic burden after cross-clamping. In an analogous way of modifying reperfusion, several trials using post-conditioning or adding cardioprotective molecules have been undertaken with varying success19. Today, interventional treatment of ACS has arrived at the same crossroads. While early reperfusion has saved numerous lives and limited morbidity, success has plateaued20. In cardiac surgery, in our experience, while testing the position of the retrograde cardioplegia catheter, another aspect of elevating pressures in cardiac veins became evident, since we have observed that brief coronary sinus occlusion cycles with PICSO have had a preconditioning effect. A randomised controlled trial to analyse further this effect for protecting myocardium in cardiac surgical patients is warranted. We therefore feel that it is time to amend the above-mentioned dogma of “time is muscle” to “adjust reperfusion”. As suggested by Angelos et al, hypoxic reperfusion prevents part of the sequelae of uncontrolled reperfusion21. PICSO, with the option to reach the occluded vascular bed with a perfect perfusate, namely venous blood, might be of potential benefit in the setting of ACS. Today, it is clearly established that opening the occluded artery as soon as possible, irrespective of the condition of the dependent perfusion area, improves outcomes. However, it might be preferable to stage reperfusion, to facilitate washout first and clear the microcirculation prior to reperfusion. A retrograde access via coronary veins, “preparing” deprived myocardial areas before peak reperfusion, might be a feasible option that could improve outcome further.
Early clinical observations of PICSO in patients undergoing lysis therapy showed an unanticipated effect on long-term results after PICSO. In the treated group, a statistically significant reduction in restenosis of the culprit lesion treated with balloon dilation only and a significant reduction in major adverse cardiac and cerebrovascular events (MACCE) suggest a benefit of adjusting reperfusion22. Therefore, PICSO effects not only enhance washout and modify the reperfusate, but also seem to induce long-lasting processes of infarct healing.
Aspects of coronary sinus pressure elevation inducing molecular signals have been tested recently in patients with chronic heart failure indicating that, beyond salvage, PICSO may induce regenerative pathways analogous to other methods using mechanotransduction to stimulate regional molecular pathways (Figure 1)23-27. These effects on coronary microcirculation and stimulating additional regenerative capacity suggest that PICSO may have other applications beyond enhancing reperfusion27. Thinking beyond primary PCI to minimise the risk of long-term structural and functional myocardial damage by modifying reperfusion may mark a new era in treating patients with ACS.
Conflict of interest statement
W. Mohl has received funding for PICSO studies from the ATOS I Austrian Science Fund (P13274-Med), the Austrian Federal Ministry of Traffic, Innovation and Technology, Vienna, Austria (BMVIT GZ609.637/000-III/12/2004), and the International Society of Coronary Sinus Interventions; and is a founder of Miracor and the Angel Valve Project (AVVie). The other authors have no conflicts of interest to declare.