“Flashes of brilliance are slow in coming. So too is their recognition”.
Steven Johnson, 2010.
In a recently published randomised trial on permanent pressure elevation in cardiac veins, Verheye et al reported significant improvement in symptoms and the quality of life in patients with refractory angina who were not candidates for revascularisation1. The implant used, Coronary Sinus Reducer System (Neovasc Inc., Richmond, BC, Canada), is designed to increase the outflow impedance for venous blood, similar to stage I of the Beck’s procedure, the surgical equivalent of the present design, used in the late 1940s and predating coronary artery bypass grafting.
Several competing concepts of transcoronary sinus catheter interventions (TCSI) aiming to recover jeopardised myocardium have evolved from historical concepts such as the Beck’s procedure and some of them have reached the clinical arena, although an unsolved dilemma persists regarding the significance of pressure elevation in cardiac veins and there are questions about mechanisms causing beneficial effects2,3.
Transcoronary sinus catheter interventions are also a good example of longevity, persistence and continuous innovation in translational medicine, since they started off from practical experimental concepts (i.e., arterialisation of cardiac veins) and clinical observations (i.e., temporary relief of cardiac symptoms due to coronary venous pressure elevation in right heart failure). Since retroperfusion of arterial blood and routes to revascularise myocardium were the primary motivation to use the “back door” of the heart, positive results have been missed or neglected in the wake of the coevolution and rapid advancements in the field of coronary artery surgery and interventional cardiology, concepts which are far easier to understand. It is therefore no surprise that evidence of decreased ischaemic burden, regaining of structural integrity, as well as improved long-term clinical outcomes, which have been associated with pressure elevation in cardiac veins, have received inadequate scientific appraisal due to the lack of evidence-supported pathophysiological background4. The obvious periodic loss of interest of the scientific community in these curative concepts reflects the need to update scientific data continuously in a quest to decipher the mode of action of retrograde interventions.
It appears that the situation has now changed for two reasons. First, state-of-the-art treatments of heart disease are still hampered by limitations, and the search for practicable amendments or alternatives continues. Second, recent publications of clinical improvements in TCSI have shifted the focus back to pressure elevation in cardiac veins. Arterialisation and retrograde flow were the early logical target of TCSI, but thorough analysis of experimental and early clinical data underscored the key role of controlled pressure elevation in the coronary venous system5,6. While the positive effects of retroperfusion seemed to depend on the elevation of coronary venous pressure achieved, excessive uncontrolled pressure augmentation was associated with myocardial oedema and detrimental functional outcomes7. Following the logic of these experiments and starting from the observation that relief of symptoms after the Beck’s procedure was absent in a large cohort of non-responders, our group has developed a pressure-controlled intermittent coronary sinus occlusion (PICSO) technique, which operates on a feedback control to limit the pressure elevation in cardiac veins and avoid restricting nutritive flow in coronary arteries (Figure 1)8. Several experimental and clinical studies have reinforced the salvage potential of PICSO. The salvaging aspect with its dual mode of action, redistributing flow towards zones of diminished perfusion and subsequent washout of toxic material, has recently been investigated in a clinical setting of acute coronary syndromes treated with primary PCI, and has been found to reduce infarct size and to clear obstructed microcirculation, as reported by van de Hoef et al in this journal9.
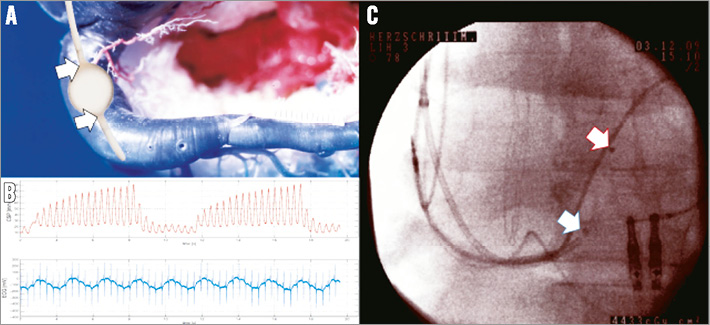
Figure 1. Transcoronary sinus catheter intervention: PICSO (pressure-controlled intermittent coronary sinus occlusion). 70% of venous drainage exits the myocardium via the coronary sinus. Temporary pressure-controlled total occlusion reverses flow from normal perfused cardiac veins towards underperfused zones. A) Schematic of a PICSO catheter is depicted on a corrosion cast of a human coronary sinus. B) Note the gradual beat per beat increase of coronary sinus pressure induced by a temporary balloon occlusion until the venous capacitance is filled. This redistributes flow towards deprived myocardium. Rapid release of the balloon blockade induces washout. Pressure peaks activate coronary venous vascular cells via mechanotransduction and this is believed to induce structural recovery according to our hypothesis “embryonic recall”. C) Coronary sinus PICSO catheter after implantation of a left ventricular electrode. Arrows show the extension of the balloon in the silent zone of the CS.
As was envisaged early on by Verdouw et al6, pressure elevation is the key step in transcoronary sinus interventions aiming at myocardial salvage. This was verified by Syeda et al5, showing a significant correlation between developed coronary sinus pressure and myocardial salvage. In addition, and as predicted by Verdouw et al6, “ventricularisation” of systolic pressure peaks seems to have an unexpected effect on regenerating myocardium by reopening developmental pathways used for endogenous cardiac repair10,11.
PICSO produces these pressure peaks in a controlled range and is presently perceived as having two independent but synergistic mechanisms which aid myocardial salvage and long-term cardiac recovery: first, the dose-dependent salvaging aspect of periodic pressure elevation in cardiac veins and, second, the threshold-dependent impulse to reinitiate cardiac development10. Activation of venous endothelium via mechanotransduction by elevated pressure in cardiac veins may be the main source of the observed improvement in long-term clinical outcomes11,12. This observation may open a completely new avenue in reversing myocardial decay and treating the failing heart.
Patients suffering from myocardial infarction, with no option for revascularisation and heart failure are the most promising clinical candidates to show scalable clinical benefit and efficacy of retrograde access technologies. To evaluate the risk versus benefit ratio, surrogate endpoints as well as equipment have to be optimised not only to allow ease of application in urgent and emergent environments, but also to claim clinical feasibility. Taking into account the two recent reports1,9, the appropriate degree and duration of pressure elevation in cardiac veins have to be established in order to achieve clinical significance2. This might be difficult in acute myocardial infarction since state-of-the-art primary revascularisation procedures are difficult to outpace, and surrogate endpoints as area at risk calculated by MRI depend on post-interventional imaging underestimating the salvage potential of PICSO, since this procedure initiates interstitial fluid mobilisation13. Pivotal proof of clinical significance will be much easier to achieve in patients with severe heart failure and no option for revascularisation with its enormous disease burden and lack of curative therapies. Although recent studies on the implantation of the Coronary Sinus Reducer System or the application of PICSO have shown clinical benefit, various questions regarding the amount and endurance of pressure elevation in cardiac veins still await a definite answer1,12,14. At present, transcoronary sinus catheter interventions have reached broad scientific interest but not a final clinical breakthrough. This is because of several confounding factors including interventional logistics, pathophysiologic considerations and lack of recognition, perhaps better understood looking into the art of origination!
In his book review on sources and qualities of novelty, Sternberg quotes and interprets two respected authors, Steven Johnson and Andrew Robinson, on the motifs of innovation15. He argues that in the end successful innovations are slow in coming and that they often evolve from previously unrelated platforms changing their outfit, even their targets. The evolutionary progress of innovations may emerge from previous errors until they show robustness in principle and are confirmed in a special coevolutionary environment.
Sternberg also quotes Thomas Kuhn when he says that it is one of the great myths of innovation that highly creative work that does not fit into existing academic paradigms tends to be dismissed. It is no surprise therefore that coronary sinus interventions, showing a history of repeated rejection of concepts and misinterpretation of results, share the same fate. It is merely a combination of how an unexpected and difficult to interpret innovation, redirecting a whole research area subdued to paradigm changes and incremental innovation, is perceived, and whether it fits into the routine environment of curative medicine.
Transcoronary sinus catheter interventions are an excellent example of intricate avenues of innovation showing an ongoing paradigm change, since they were created under a completely different determination, namely retrograde arterialisation of the myocardium known as the Beck’s procedure. Building on the changing paradigms of Beck’s concept, periodic controlled pressure elevation in cardiac veins may create the milieu necessary not only to ameliorate the consequences of necro-apoptosis in acute coronary syndromes, but also effectively to re-enter endogenous pathways of structural repair.
Conflict of interest statement
W. Mohl is a founder, board member and stockholder of Miracor Medical Systems, Vienna, Austria. The other authors have no conflicts of interest to declare.