Abstract
Aims: The aim of this study was to evaluate the clinical efficacy of Coronary Sinus Reducer implantation in alleviating angina symptoms and improving objective ischaemia parameters and indices of physical capacity.
Methods and results: Patients with refractory angina (Canadian Cardiovascular Society [CCS] class 3-4) were treated with the Reducer. Baseline and follow-up evaluation consisted of clinical assessment including completion of the Seattle Angina Questionnaire (SAQ) and CCS class evaluation, and objective assessment by treadmill exercise test, dobutamine echocardiography and six-minute walk test (6MWT). Overall, 48 patients (40 male) were enrolled. No periprocedural or long-term adverse events were recorded. CCS class diminished from a mean of 3.4±0.5 at baseline to 2.0±1 (p<0.001), and all domains of the SAQ improved significantly following Reducer implantation. Mean exercise duration increased from 03:43±01:30 to 04:36±02:18 min:sec (p=0.025) and 6MWT distance increased from 299.9±97.9 m to 352.9±75.3 m (p=0.002). Ejection fraction (EF%) at stress increased from 51.0±10 to 56.5±10 (p=0.004), and wall motion score index improved from 1.58±0.4 to 1.37±0.3 (p=0.004).
Conclusions: Reducer implantation for the treatment of refractory angina is a simple and safe procedure which significantly alleviates symptoms of angina and improves objective ischaemia parameters and indices of physical function.
Abbreviations
CABG: coronary artery bypass graft
CAD: coronary artery disease
CCS: Canadian Cardiovascular Society
CMR: cardiac magnetic resonance
CRT: cardiac resynchronisation therapy
CS: coronary sinus
EF: ejection fraction
LAO: left anterior oblique
MPRI: myocardial perfusion reserve index
PCI: percutaneous coronary intervention
RCA: right coronary artery
SAQ: Seattle Angina Questionnaire
6MWT: six-minute walk test
TAVR: transcatheter aortic valve replacement
WMSI: wall motion score index
Introduction
Despite the remarkable progress in the treatment of ischaemic heart disease, a growing number of patients continue to experience severe angina despite optimal medical therapy1-3. Refractory angina is a disabling condition and a major public health problem. It is common not only in patients who are not good candidates for revascularisation, but also in patients following successful revascularisation. The prevalence of angina that persists following successful revascularisation procedures is as high as 25% after one year, and up to 45% after three years2. Moreover, a recently published study failed to show benefit for percutaneous coronary intervention (PCI) over a sham procedure in prolonging exercise duration and relieving angina symptoms in patients with stable coronary artery disease (CAD)4.
Refractory angina might be the presenting symptom of a wide range of clinical entities, including obstructive CAD, microvascular disease, hypertrophic cardiomyopathy, and left ventricular diastolic dysfunction.
Coronary sinus (CS) narrowing by Reducer (Coronary Sinus Reducer™ System; Neovasc Inc., Richmond, BC, Canada) implantation has emerged as a new therapeutic option for the treatment of patients suffering from severe refractory angina pectoris who are not good candidates for revascularisation5-9. The CS Reducer is a stainless steel mesh designed to create a fixed focal narrowing in the lumen of the CS, thus increasing backwards pressure, which may cause a slight dilatation of the arterioles in the ischaemic subendocardial myocardium with a presumed subsequent reduction of subendocardial vascular resistance, and redistribution of blood from the less ischaemic subepicardium to the more ischaemic subendocardium, which may lead to symptoms relief10,11.
Several clinical reports described the feasibility, safety and efficacy of CS narrowing as a treatment for patients suffering from refractory angina5,7,12. Moreover, a prospective, randomised, double-blind, sham controlled clinical trial (the Coronary Sinus Reducer for Treatment of Refractory Angina [COSIRA] trial) demonstrated a significant improvement in symptoms among patients with severe refractory angina (CCS class 3-4) treated with CS narrowing compared with sham procedure-treated patients9. Nevertheless, data regarding improvement in objective parameters of ischaemia and functional capacity following Reducer implantation are still limited7,12.
In the present study, we evaluated subjective indices of angina and quality of life, as well as objective parameters of ischaemia, at baseline and six months following Reducer implantation.
Methods
Presented here is a prospective, non-randomised, open-label registry study of consecutive patients undergoing Reducer implantation in the Tel Aviv Medical Center, Tel Aviv, Israel. The study was approved by the national and the local institutional ethics committees. All participants signed a written informed consent for participation in the study.
PATIENT SELECTION
Patients suffering from severe disabling angina despite optimal medical therapy (CCS class 3 or 4), with objective evidence of myocardial ischaemia of the left coronary arteries territory by perfusion scan and/or by dobutamine echocardiography, and ejection fraction ≥30%, who were deemed non-candidates for surgical or percutaneous coronary revascularisation were enrolled. Excluded were patients with one or more of the following: recent (within three months) myocardial infarction, PCI or coronary arterial bypass grafting (CABG), life-threatening rhythm disorders, decompensated heart failure, severe valvular heart disease. Patients with an EF <30% who may require cardiac resynchronisation therapy (CRT) implantation, and patients with a mean right atrial pressure higher than 15 mmHg were also excluded.
THE CS REDUCER DEVICE
The Reducer has previously been described in detail6,8,13. Briefly, it is a stainless steel, balloon-expandable, hourglass-shaped mesh, designed to be introduced into the CS through the right internal jugular vein. A few weeks following implantation, the Reducer is covered by tissue13. Only then, when the narrowing is established, and the blood flow is directed through the narrowed centre, is pressure gradient generated. The diameter at the narrowed mid portion of the Reducer is 3 mm, and it can reach diameters of 7-13 mm at both ends using an inflation pressure of 2 to 4 bars.
THE REDUCER IMPLANTATION PROCEDURE
The technical aspects of the Reducer implantation procedure have been reported previously6. In short, following pre-treatment with aspirin and clopidogrel and under local anaesthesia, a 6 Fr diagnostic multipurpose or Amplatz Left (AL-1) catheter is introduced into the CS through the right internal jugular vein, under fluoroscopic guidance. Following angiography of the coronary sinus in a 30-degree left anterior oblique (LAO) angulation, the optimal site for implantation is determined according to the CS diameter and to avoid side branch bifurcation. In patients in whom the CS diameter is >13 mm, implantation of the Reducer is contraindicated as it may result in insufficient oversizing and migration of the device. The diagnostic catheter is then replaced (over the wire) with a pre-shaped 9 Fr guiding catheter, and IV heparin is administered. The Reducer, crimped on a balloon, is then introduced over the wire in the guiding catheter into the CS, positioned at the desired site, and implanted by inflating the delivery balloon to achieve slight oversizing. Post-implantation angiography is performed to ensure appropriate implantation, patency, and appropriate reduction of the lumen diameter. Duel antiplatelet therapy is recommended for six months following the procedure.
BASELINE AND FOLLOW-UP CLINICAL EVALUATION
Baseline and six-month follow-up evaluation consisted of determination of CCS class, patients’ completion of the Seattle Angina Questionnaire (SAQ)14, treadmill stress test, dobutamine echocardiography, and a six-minute walk test (6MWT)15. Clinical evaluation and CCS determination at follow-up were performed by two cardiologists who were not blinded to therapy. SAQs were completed by the patients in a separate room without involvement of the treating staff, and other tests (treadmill test and echocardiography) were performed by technicians and cardiologists who were unaware of the time point of the test in relation to treatment.
SEATTLE ANGINA QUESTIONNAIRE
The scores of the five domains of the questionnaire (physical limitation, angina stability, angina frequency, treatment satisfaction and quality of life) were calculated, and baseline and follow-up scores were compared.
TREADMILL EXERCISE TEST
The Bruce protocol treadmill exercise stress test was used. Total exercise duration (in sec) before, and six months after Reducer implantation was compared.
ECHO DOBUTAMINE
A 16-segment quantitative analysis was used for wall motion score calculation. The wall motion of each segment at rest and during peak dobutamine infusion was graded according to a score (1 - normal, 2 - hypokinetic, 3 - akinetic, 4 - dyskinetic, 5 - aneurysmatic)16. The summed wall motion scores of myocardial segments divided by the number of segments was defined as wall motion score index (WMSI). Baseline and six-month WMSI at rest and stress, as well as ejection fraction (EF%) at rest and stress were compared.
STATISTICAL ANALYSIS
All data are displayed as mean (±standard deviation) and/or median (with interquartile range [IQR]) for continuous variables. The paired t-test was used to evaluate the statistical significance between baseline and six-month parameters. All the analyses were considered significant at a two-tailed p-value of <0.05.
Results
Overall, 75 patients were referred for screening and 48 patients (40 males, mean age 66.8±8.9) with severe angina were enrolled between August 2011 and November 2017 (details of the screening procedure and screen failures are presented in Figure 1). The procedure was successful in 46 (96%) patients and failed in two (4%) due to an unsuitable CS anatomy. In one case, the CS was too wide and in the other case the operator failed to perform a deep intubation of the CS due to the presence of valves. In these two patients, no procedure-related complications were observed. Among the remaining 46 patients the procedure was uneventful, apart from one case of device migration, due to a wide CS. In that case, the Reducer was successfully retrieved into a 22 Fr sheath which was inserted into the right femoral vein using an AndraSnare AS-25 (Andramed GmbH, Reutlingen, Germany). Another device was then successfully implanted deeper in the CS without any adverse consequences.
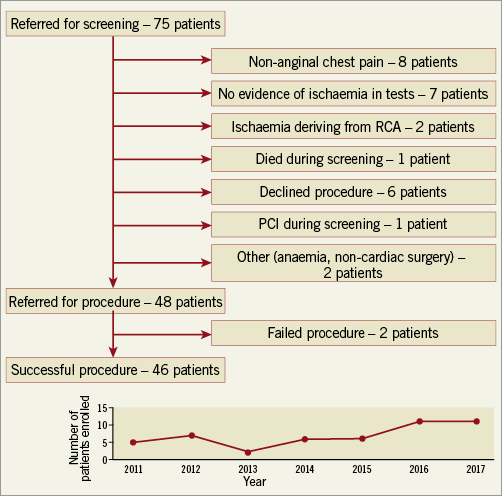
Figure 1. Screening procedure and screen failures.
SAFETY
No procedure- or device-related events were observed during a median follow-up period of 12.5 months (range 2-32 months). Three patients were lost to follow-up for the six-month evaluation but were known to be alive, while four other patients have not yet completed the six-month evaluation. During the follow-up period, three patients died. No deaths were related to the device or the procedure; one patient died >1 year after implantation following a gradual general physical deterioration, one patient died suddenly several months following implantation at the age of 86, and another patient who was diagnosed with severe aortic stenosis several months following Reducer implantation underwent transapical transcatheter aortic valve replacement (TAVR) and died in the hospital several days following the procedure.
During the follow-up period, three patients underwent PCI for new coronary lesions due to their underlying, progressive CAD. One patient presented with unstable angina and the other two presented with stable angina. Lesions were located in the right coronary artery (RCA) in two patients and in the circumflex artery in the third case.
BASELINE AND FOLLOW-UP CLINICAL EVALUATION
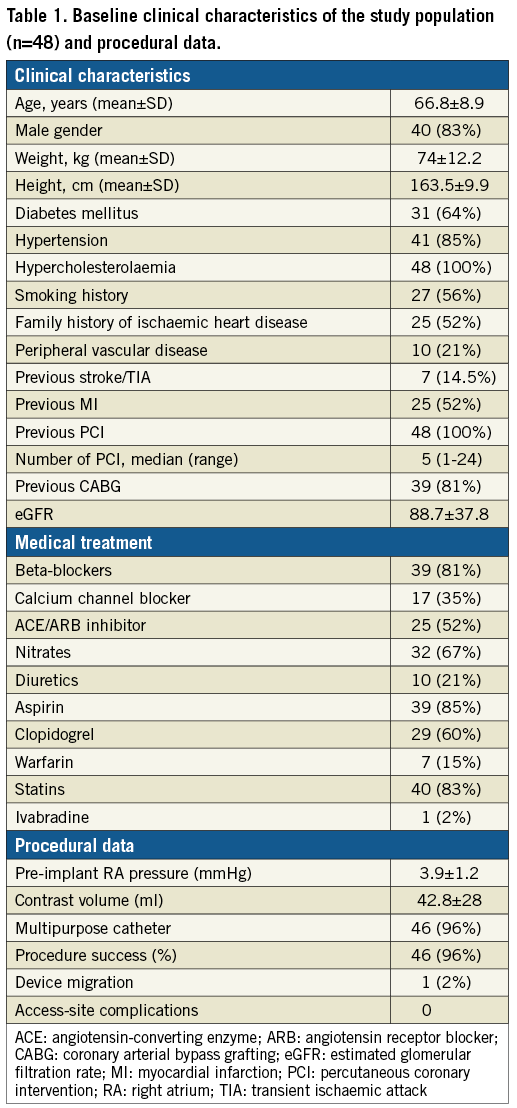
Baseline clinical characteristics and procedural data are presented in Table 1. The study population is characterised by a high prevalence of cardiac risk factors and previous myocardial infarctions and many previous revascularisation procedures. At baseline, patients had symptoms of angina at minimal effort or at rest.
CCS CLASS AND SEATTLE ANGINA QUESTIONNAIRE
Overall, 33/39 (85%) patients reported relief of symptoms expressed as at least one CCS class improvement following the procedure and 19/39 (48%) reported improvement of at least two CCS classes. Mean angina score expressed by CCS class decreased from 3.4±0.5 to 2.0±1 (p<0.001) at six months (n=39 patients) and 1.9±0.9 (n=24) at one year following Reducer treatment (Figure 2). All domains of the SAQ improved significantly six months after Reducer implantation (Table 2, Figure 3).
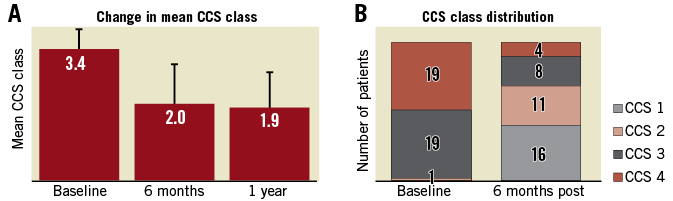
Figure 2. Improvement in CCS class following Reducer implantation. A) Change in mean CCS class at six months and one year. B) CCS class distribution at baseline and six months.
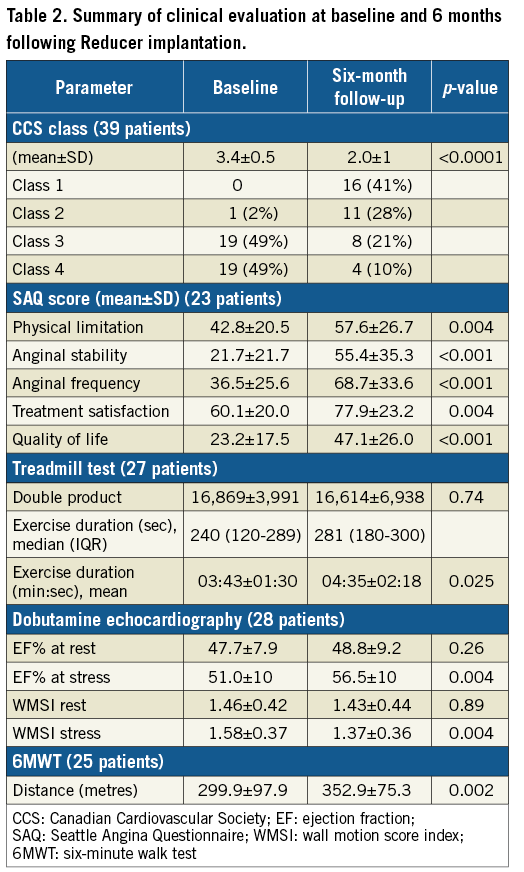
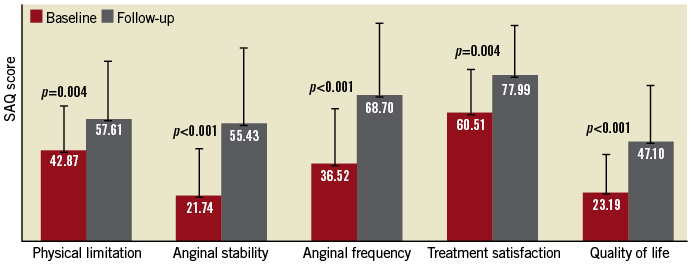
Figure 3. Seattle Angina Questionnaire scores at baseline and six months following Reducer implantation.
TREADMILL STRESS TEST, 6MWT AND DOBUTAMINE ECHOCARDIOGRAPHY STRESS TEST
The results of the tests are presented in Table 2 and Figure 4. Among patients performing the treadmill stress test, mean exercise duration increased from 03:43±01:30 min:sec to 04:35±02:18 min:sec (p=0.025). Mean six-minute walk distance increased from 299.9±97.9 m to 352.9±75.3 m (p=0.002). Dobutamine echocardiography showed improvement in both ejection fraction (EF%) during stress, and WMSI (51.0±10 vs. 56.5±10 and 1.58±0.37 vs. 1.37±0.36, respectively, p=0.004 for both).
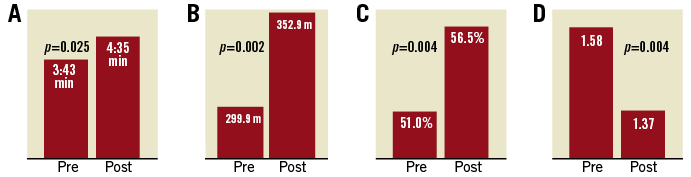
Figure 4. Improvement in physical capacity before and after Reducer implantation. A) Exercise duration. B) Six-minute walk test (6MWT). C) Ejection fraction during stress. D) Wall motion score index (WMSI).
Discussion
The purpose of the present study was to evaluate the impact of Reducer implantation on quality of life and effort capacity in patients suffering from severe disabling refractory angina pectoris. The main findings of the study can be summarised as follows. First, Reducer implantation is feasible and safe, and is associated with significant reduction of angina severity and improvement in quality of life, as reflected by the SAQ. Second, physical capacity and effort tolerance assessed by treadmill exercise duration and by 6MWT improved following Reducer implantation. Third, ischaemic burden, as evaluated by stress echocardiography, was significantly reduced following Reducer treatment.
The CS Reducer emerged as an effective new therapy for patients with refractory angina who until recently were labelled as “no option” patients6,7,17. The COSIRA randomised, double-blind, sham controlled clinical trial demonstrated that, on top of a prominent placebo effect noted in both groups, narrowing of the CS was associated with greater angina relief compared to a sham procedure9. Nevertheless, evidence of improvement in objective parameters of physical capacity and reduction of ischaemic burden following Reducer implantation is still limited. In the first-in-man (FIM) study, Banai et al12 reported a reduction of mean maximal ST depression in nine patients undergoing exercise testing before and after Reducer implantation, and improvement in wall motion score in 8/13 patients undergoing dobutamine echocardiography following Reducer implantation. Similarly, we previously reported promising results in a small group of patients undergoing exercise testing and dobutamine echocardiography before and after treatment with the Reducer7.
The effect of the CS Reducer on myocardial perfusion has also been assessed by measuring myocardial perfusion reserve index (MPRI) using perfusion dipyridamole cardiac magnetic resonance (CMR). Among 16 patients undergoing Reducer implantation with baseline rest-stress CMR and four-month follow-up, global MPRI increased from 1.46±0.40 to 1.80±0.7813.
In the present study, we provide additional evidence, among a larger number of patients, of objective improvement in physical capacity and parameters of ischaemia following Reducer implantation (increase in Bruce protocol treadmill stress test exercise duration and 6MWT distance, reduction of wall motion score, and improvement of ejection fraction during dobutamine stress echocardiography). Importantly, our study, as well as all other studies mentioned above, included mainly patients with refractory angina and evidence of ischaemia, related to severe obstructive CAD. Conversely, Giannini et al18 recently reported their first experience with the Reducer for the treatment of refractory angina in eight patients without obstructive CAD. They showed an improvement in CCS class, SAQ domains, 6MWT distance and MPRI, suggesting that the Reducer might be effective not only in patients with obstructive CAD but also in patients with microvascular angina.
The presumed mechanism by which the Reducer lessens ischaemia may be explained as follows. In the healthy heart, blood flow in the subendocardial myocardium is normally higher than in the subepicardial layers of the myocardium. During exercise and increased demand, a physiologic compensatory mechanism causes selective sympathetically mediated vasoconstriction with increased resistance to flow in subepicardial vessels, favouring subendocardial perfusion and allowing an appropriate augmented contractility. However, in the presence of a significant epicardial coronary artery stenosis, this compensatory mechanism becomes dysfunctional and the transmural myocardial perfusion is redistributed towards the subepicardial layers of the myocardium. The normal ratio between subendocardial and subepicardial blood flow is significantly reduced, reflecting shifting of blood from the higher resistant subendocardial blood vessels to the less resistant subepicardial blood vessels. Thus, the perfusion of the subendocardium during stress becomes compromised, causing ischaemia, impaired contractility, reduced ejection fraction and elevated left ventricular end-diastolic pressure (LVEDP), with consequent angina symptoms and shortness of breath19. Elevated LVEDP exerts an external pressure on the subendocardial capillaries and arterioles, which further increases the resistance to flow, contributing to the vicious cycle of subendocardial ischaemia.
Elevating backward pressure in the coronary venous system presumably results in a slight dilatation of the diameter of arterioles that may lead to a significant reduction in vascular resistance in the subendocardium. Consequently, blood flow to the ischaemic subendocardial layers of the myocardium is enhanced, contractility improves, ejection fraction increases and LVEDP decreases. Thus, the result of the decreased subendocardial vascular resistance is redistribution of blood from the less ischaemic subepicardium to the more ischaemic subendocardium, which will lead to symptom relief10,11.
Limitations
We acknowledge several limitations of this report. First, the observational nature of this study precluded us from attenuating the placebo effect, which has been widely reported in previous refractory angina studies. However, the objective improvement demonstrated in this study makes it reasonable to suggest that the clinical benefit attributed to the Reducer outweighs the placebo effect. Second, CCS evaluation was performed by cardiologists who were not blinded to treatment, thus potentially leading to a certain bias. Third, the study includes a relatively small number of patients and, due to the inability of some patients to perform exercise, for some patients we report only the results of the subjective parameters assessed. Moreover, some patients lack SAQ and 6MWT data as these tests were added to the evaluation later in the study. Fourth, as mentioned previously, three patients were lost to follow-up and four others have not yet completed the follow-up evaluation. For these patients, we reported only the procedural data. Finally, we did not have cardiac MRI available for the evaluation of the severity of ischaemia before and after Reducer implantation and therefore used stress echocardiography as an alternative, which is less accurate.
Conclusions
Our study, together with other accumulating data, supports the clinical benefit of the Reducer in alleviating symptoms of angina, improving exercise capacity and quality of life, and reducing myocardial ischaemia in patients with refractory angina who are not good candidates for revascularisation. It remains to be investigated, in larger studies, utilising objective methods of assessment of myocardial ischaemia, whether patients with angina related to other chronic cardiac conditions such as microvascular angina, diastolic dysfunction and hypertrophic cardiomyopathy might also benefit from this innovative therapy.
| Impact on daily practice Refractory angina is a disabling condition which affects patients’ quality of life and has a significant impact upon healthcare resources. Patients suffering from persistent refractory angina are often labelled as “no option” patients. Reducer implantation is a novel therapeutic option intended for patients suffering from this chronic, disabling condition. |
Funding
The study was funded by internal resources.
Conflict of interest statement
S. Banai is the medical director of Neovasc Inc. The other authors have no conflicts of interest to declare.