Introduction
The coronary sinus (CS) Neovasc Reducer™ (NR) System (Neovasc Inc., Richmond, BC, Canada) is a balloon-expandable stainless steel mesh, which is implanted in the CS to create a controlled narrowing of the lumen and a pressure gradient across it. Although the mechanism underlying its effectiveness is not understood, the device is intended to increase coronary venous pressure, thus improving perfusion to ischaemic territories of the myocardium by forcing redistribution of blood from the less ischaemic subepicardium to the more ischaemic subendocardium. It is currently indicated for the treatment of refractory angina in patients unsuitable for coronary revascularisation, resulting in an improvement in symptoms in 70-85% of patients1 (Supplementary Figure 1). The reason why 15-30% do not gain clinical benefit is still unknown.
In view of the heterogeneous nature of the venous system in human hearts, the presence of alternative venous drainage systems to the CS may be crucial in determining whether patients might benefit from this intervention. On the basis of our experience regarding implantation in more than 100 patients to date, we propose here two paradigmatic clinical cases in support of this hypothesis and a simple method to predict responders to NR implantation to stimulate further research on the topic, while waiting for further and more robust data.
Methods
Right atrial pressure (RAP), corresponding to baseline CS pressure, is measured and recorded before NR implantation. The NR System (balloon catheter with a pre-mounted scaffold) is advanced over a 0.035” wire into the CS and the device is deployed by inflating the delivery balloon for at least 60 seconds at 4-6 atmospheres to achieve a 10-20% oversizing of the device. During deployment of the NR, with the balloon inflated and occlusive of the CS, the 0.035” wire is removed and the CS wedge pressure is measured through the lumen of the balloon catheter. Dipyridamole stress cardiac magnetic resonance (CMR) perfusion study (Philips Ingenia 1.5T scanner; Philips, Best, the Netherlands) with assessment of myocardial perfusion reserve index (MPRi) using dedicated software (Intellispace Portal v.8; Philips) was performed before and three months after NR implantation to assess myocardial ischaemia objectively. MPRi is derived from maximal upslopes of stress to rest myocardial contrast signal intensity time curves, normalised to left ventricle input [(myocardial upslopestress/LV cavity upslopestress)/(myocardial upsloperest/LV cavity upsloperest)]. MPRi values of >2 were reported in a reference population2.
Results
Both patients underwent uneventful NR implantation for refractory angina due to diffuse left anterior descending (LAD) artery disease unsuitable for revascularisation procedures. The patients’ left and right ventricular function parameters are summarised in Supplementary Table 1.
Patient 1 was a 58-year-old female with Canadian Cardiovascular Society (CCS) Class III refractory angina. At the stress CMR she demonstrated a reversible perfusion defect in the LAD artery distribution territory and her baseline MPRi was 1.26 (Figure 1, upper left A-E). Baseline systolic RAP was 8 mmHg, CS systolic wedge pressure was 60 mmHg, and the difference was 52 mmHg (Figure 2A). At three-month follow-up, she reported reduction in angina (CCS I), demonstrated an increase in the global MPRi to 1.51 (p=0.008) (Figure 1, upper left D & E), and an improvement in the Seattle Angina Questionnaire (SAQ) (Figure 1, lower left).
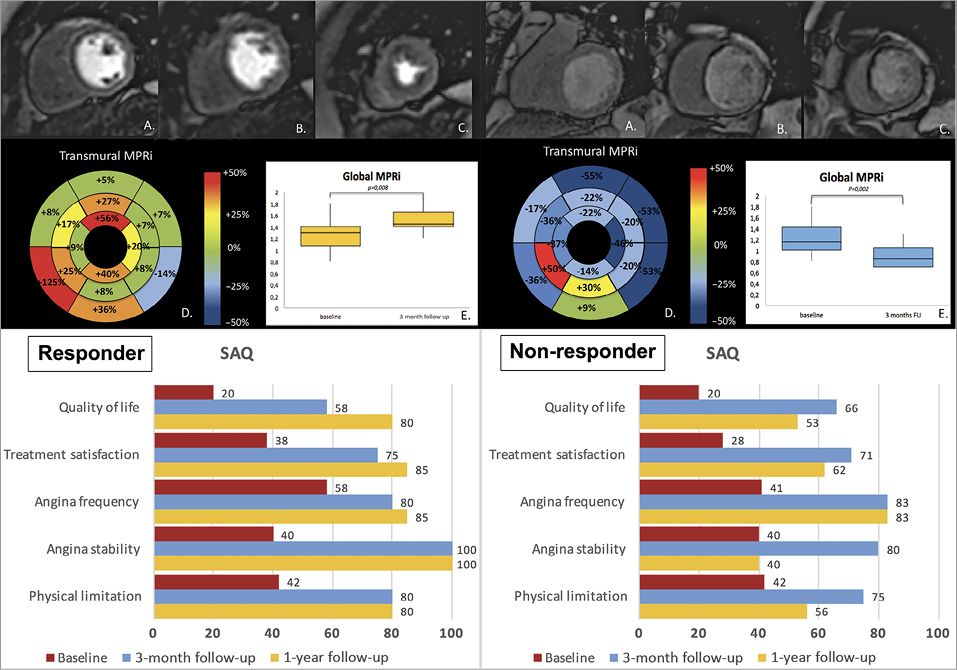
Figure 1. Stress perfusion CMR and SAQ scores. Upper left: first-pass perfusion CMR images from base to apex (A-C) before Reducer implantation showing a subendocardial perfusion defect involving the anterior wall and septum from the base (A) to the apex (C) and the inferior apical wall (C). Bull’s-eye plot of the percentage of MPRi modification after Reducer implantation shows an increase (+35% with respect to baseline), mainly due to a significant increased perfusion in ischaemic territories (D & E). Lower left: SAQ score variations. Upper right: first-pass perfusion CMR images from base to apex (A-C) before Reducer implantation showing a transmural perfusion defect involving the mid-apical septum (B & C) and the anterior apical wall (C). Bull’s-eye plot of the percentage of MPRi modification after Reducer implantation in each myocardial segment shows a reduction of myocardial perfusion in most segments (D & E). Lower right: SAQ score variations.
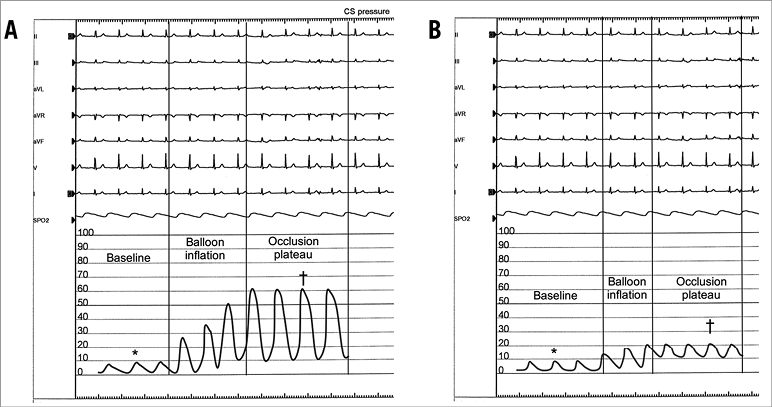
Figure 2. CS pressure measurements. A) Note the high increment in CS pressure values during balloon occlusion in the responder patient, reaching a plateau after 2-3 cardiac cycles, due to systolic squeezing of the venous blood pool. B) Note the scarce increment in CS pressure in the non-responder patient, as compared to the responder patient. All reported values are systolic CS pressures. *baseline systolic pressure; †wedge systolic pressure
Patient 2 was a 65-year-old male who underwent NR implantation for refractory angina (CCS IV). Similarly to patient 1, stress CMR showed a reversible perfusion defect in the LAD artery distribution territory and his baseline MPRi was 1.22 (Figure 1, upper right A-E). Baseline systolic RAP was 3 mmHg and CS systolic wedge pressure was 20 mmHg; the difference was 17 mmHg (Figure 2B). At three-month follow-up, he reported reduction in angina (CCS I) and increments in SAQ scores (Figure 1, lower right). However, CMR at three-month follow-up did not show any myocardial ischaemia improvement (MPRi decremented to 0.9, p=0.002).
At 12 months, patient 1 still presented in CCS I and the SAQ scores were higher than at baseline and at three months. On the other hand, patient 2 complained of a relapse of severe angina (CCS III) and a worse quality of life (as detected by SAQ scores) (Figure 1, lower panels). A contrast-enhanced computed tomography scan performed in patient 2 at 12-month follow-up excluded two potential causes of his worsening: coronary artery disease progression and thrombosis of NR with consequent CS occlusion (Supplementary Figure 2).
Discussion and limitations
A greater increase of CS pressure during CS occlusion as compared to the baseline value is expected in patients with high CS flow and poor alternative venous drainage systems. Conversely, a lower difference between baseline systolic RAP and CS systolic wedge pressure is expected in patients with a well-developed alternative venous drainage system, who are the ones who will more likely not benefit from NR implantation.
The two reported cases seem to support this hypothesis, showing objective myocardial ischaemia improvement only in the patient with significant CS pressure rise during its occlusion.
Although the patient without significant rise in CS wedge pressure (patient 2) had an initial clinical improvement, he did not show any MPRi improvement at three months and, consistently, lost clinical benefits at 12-month follow-up, suggesting a transient placebo effect (as high as 30% in published studies on refractory angina based on subjective endpoints such as angina).
No specific cut-off pressure to predict the efficacy of the device exists and there is still uncertainty about the correct way to interpret CS pressure wave variations. We chose CS systolic pressure, as it showed the most pronounced rise during CS balloon occlusion. However, two main co-determinants of CS systolic pressure need to be taken into account: intra-myocardial systolic pressure and CS pressure dependency on anterograde arterial blood flow (inflow dependency), both of which can affect measured values. The relative importance of these factors and how their variability among subjects could impact on observed values is not known.
Conclusions
This simple technique may be a promising, rapid and simple qualitative method to assess the expected clinical benefit from Neovasc Reducer implantation and provides interesting pathophysiological insights into the device mechanism of action.
| Impact on daily practice Answering the question why 15-30% non-responders are a constant across the literature and finding novel non-invasive ways to explore CS haemodynamics may help clinicians to select patients to undergo Neovasc Reducer implantation, avoiding useless procedures and risks. |
Conflict of interest statement
S. Banai is Medical Director of Neovasc, Inc. F. Giannini is a consultant for Neovasc Inc. The other authors have no conflicts of interest to declare.
Supplementary data
Supplementary Table 1. Patient characteristics.
Supplementary Figure 1. Reducer efficacy data from currently published studies. Note how a figure of 15-30% non-responders is consistent across all the studies.
Supplementary Figure 2. Contrast-enhanced CT scan reconstructions of CS and Reducer device. Note how the device appears viable and free of thrombosis on simple (A), 2D (B) and 3D (C) reconstructions.
To read the full content of this article, please download the PDF.