Abstract
Aims: Refractory angina is still a major public health problem. The coronary sinus Reducer (CSR) has recently been introduced as an alternative treatment to reduce symptoms in these patients. The aim of this study was to investigate objective improvements in effort tolerance and oxygen kinetics as assessed by cardiopulmonary exercise testing (CPET) in patients suffering from refractory angina undergoing CSR implantation.
Methods and results: In this multicentre prospective study, patients with chronic refractory angina undergoing CSR implantation were scheduled for CPET before the index procedure and at six-month follow-up. The main endpoints of this analysis were improvements in VO2 max and in VO2 at the anaerobic threshold (AT). Clinical events and improvements in symptoms were also recorded. A total of 37 patients formed the study population. The CSR implantation procedure was successful and without complications in all. At follow-up CPET, significant improvement in VO2 max (+0.97 ml/kg/min [+11.3%]; 12.2±3.6 ml/kg/min at baseline vs 13.2±3.7 ml/kg/min, p=0.026), and workload (+12.9 [+34%]; 68±28 W vs 81±49 W, p=0.05) were observed, with non-significant differences in VO2 at the AT (9.84±3.4 ml/kg/min vs 10.74±3.05 ml/kg/min, p=0.06). Canadian Cardiovascular Society (CCS) grade improved from a mean of 3.2±0.5 to 1.6±0.8 (p<0.01), and significant benefits in all Seattle Angina Questionnaire variables were shown.
Conclusions: In patients with obstructive coronary artery disease suffering from refractory angina, the implantation of a CSR was associated with objective improvement in exercise capacity and oxygen kinetics at CPET, suggesting a possible reduction of myocardial ischaemia.
Introduction
Available data from large registries suggest that the number of patients suffering from refractory angina is constantly increasing. It is estimated that 5-10% of patients with a history of ischaemic heart disease suffer from angina, refractory to medical and interventional therapies, and 30% of patients following revascularisation suffer from persistent angina1,2,3,4. These patients present with recalcitrant angina symptoms despite optimal medical treatment, with lack of revascularisation options. In addition, they are considered at higher risk for new hospitalisations and increased incidence of adverse cardiac events1. The coronary sinus Reducer™ (CSR; Neovasc Inc., Richmond, BC, Canada) was recently introduced as a therapeutic option in patients with refractory angina who are not candidates for coronary revascularisation. This hourglass balloon-expandable mesh is implanted in the coronary sinus (CS), creating, once completely covered by ingrowth of tissue, an iatrogenic narrowing with augmented backwards pressure. The narrowing forces redistribution of coronary flow from the non-ischaemic subepicardial areas to the ischaemic subendocardial layers of the myocardium, thus relieving ischaemia and angina symptoms5. Benefits in terms of angina relief and improvements in quality of life have been demonstrated in the majority of patients by the first randomised trial and from “real-life” registries6,7. In addition, data showing improvement in objective evidence of myocardial ischaemia (as shown by enhanced myocardial perfusion at cardiac magnetic resonance imaging [MRI]), and in diastolic function, as well as very long-term follow-up safety and efficacy data have been published8,9,10,11,12,13,14.
Nevertheless, more robust evidence of the effect of the CSR on myocardial ischaemia is required. A cardiopulmonary exercise test (CPET) detects myocardial ischaemia with higher sensitivity than a conventional ECG stress test15. Indeed, patients with exercise-induced silent or symptomatic ischaemia have been found to have lower peak VO2 and oxygen pulse compared with non-ischaemic controls, also in the absence of ECG changes15. In addition, decreased VO2 at the anaerobic threshold (AT) has also been consistently shown to be related to the presence15,16,17,18,19 and the extent20 of myocardial ischaemia. The aim of this study was to investigate objective improvement in effort tolerance and in oxygen kinetics parameters by CPET in patients with refractory angina treated with CSR implantation.
Methods
This is a prospective, two-centre, international registry conducted at Antwerp Cardiovascular Center, Ziekenhuis Netwerk Antwerpen (ZNA) Middelheim (Antwerp, Belgium) and Tel Aviv Medical Center, Tel Aviv University Medical School (Tel Aviv, Israel). All consecutive patients referred to the study centres for evaluation for CSR implantation were considered for CPET before the procedure and scheduled for a follow-up CPET at six months when eligible. All patients had evidence of reversible myocardial ischaemia at non-invasive imaging stress tests, left ventricular ejection fraction of more than 25%, and no option for revascularisation according to the local Heart Team decision. Indication for CSR implantation included age >18 years, obstructive coronary artery disease with chronic refractory angina, and Canadian Cardiovascular Society (CCS) grade II to IV despite maximally tolerated anti-anginal medical therapy for at least 30 days before screening. Medical therapy included beta-blockers, calcium channel blockers, nicorandil, ivabradine, and short-acting/long-acting nitrates used at maximum tolerated doses. Clinical outcome was established with variation in CCS score and in quality of life as assessed with the Seattle Angina Questionnaire (SAQ). By protocol, the same anti-angina medical treatment was maintained before CSR implantation and at follow-up, to avoid possible confounders in clinical/CPET benefits.
DEVICE AND IMPLANTATION PROCEDURE
The Reducer’s mechanism of action and implantation technique have been described in detail elsewhere5. In short, the Reducer is a stainless steel balloon-expandable mesh designed to establish narrowing of the CS. It is available in a single size, adaptable to the tapered anatomy of the CS by the balloon inflation pressure (diameter 3 mm in the mid portion, 7-13 mm at both ends). The procedure consists of selectively cannulating the CS from the right internal jugular vein, generally achieved with a diagnostic multipurpose catheter. A dedicated 9 Fr guiding catheter is exchanged over a wire and used to deliver the Reducer. Implantation is performed by inflating the semi-compliant balloon in order to conform adequately to the CS anatomy. A final angiogram is always performed to confirm proper positioning of the device.
Dual antiplatelet therapy was maintained for six months after the implantation.
CARDIOPULMONARY EXERCISE TEST
Cardiopulmonary exercise testing was carried out on an electromagnetic bicycle ergometer (Ergometrics 800S; SensorMedics, Yorba Linda, CA, USA), using a standardised protocol in the two study centres. Each patient was examined with the same protocol in the pre-implantation evaluation and at six-month follow-up. Breath-by-breath minute ventilation (VE), carbon dioxide production (VCO2), and oxygen consumption (VO2) were measured using a Medical Graphics metabolic cart (ZAN; nSpire Health GmbH, Oberthulba, Germany). Peak VO2 was defined as the highest averaged 30-second VO2 during exercise. Whenever possible, the test was conducted, by protocol, until the patient’s exhaustion.
The AT is calculated according to the modified V-slope method. The slope of the ventilation versus the volume of exhaled carbon dioxide (VCO2) relationship (VE/VCO2 slope) was evaluated, excluding, when present, its final non-linear portion due to acidotic ventilatory drive. Heart rate reserve was calculated as the difference between the predicted maximal heart rate, based on age, and the measured heart rate at peak VO2. The O2 pulse was determined by dividing the VO2 by the simultaneously measured heart rate. Blood pressure was measured at rest and every two minutes during the exercise and recovery phases.
STATISTICAL ANALYSIS
Baseline and outcome data were analysed using descriptive statistics. Numerical values were expressed as mean±standard deviation (SD) or median (interquartile range [IQR]), as appropriate. Categorical variables were expressed as percentages. Comparisons of measured outcomes were performed using Fisher’s exact test to compare binary and categorical variables and a paired Student’s t-test for continuous variables. A two-tailed probability value of p<0.05 was considered statistically significant. All statistical analyses were performed using SPPS, Version 22.0 (IBM Corp., Armonk, NY, USA).
Results
During the study period, a total of 94 patients underwent CSR implantation in the two study centres. Of these, 37 patients were eligible to participate and were included in the present study (13 in the centre of Antwerp and 24 in the centre of Tel Aviv). Most of the patients treated with CSR were referred to us from different hospitals. This represented the major reason for not participating in the present study; other reasons consisted of inability to perform the CPET and presence of a pacemaker.
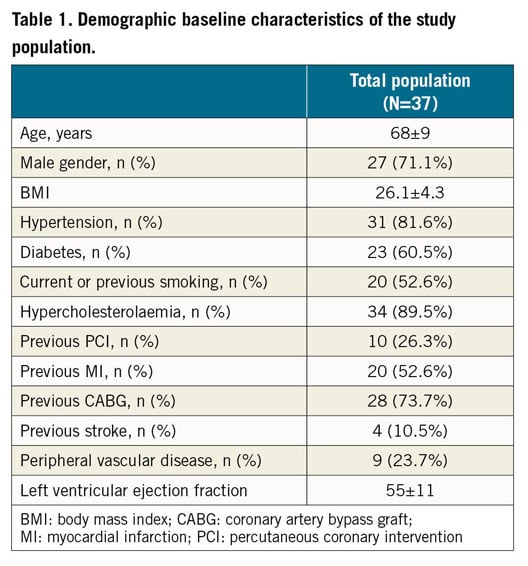
Demographic baseline characteristics of the study population are shown in detail in Table 1. Briefly, the majority of patients were male, with a mean age of 68±9 years, and a history of previous coronary artery bypass grafting (CABG) in more than 70% of cases. All suffered from chronic angina CCS class III (73%) or IV (24.3%), except one (2.6%) who was in CCS class II (Table 2). The implantation procedure was successful and uncomplicated in all patients.
CLINICAL OUTCOME
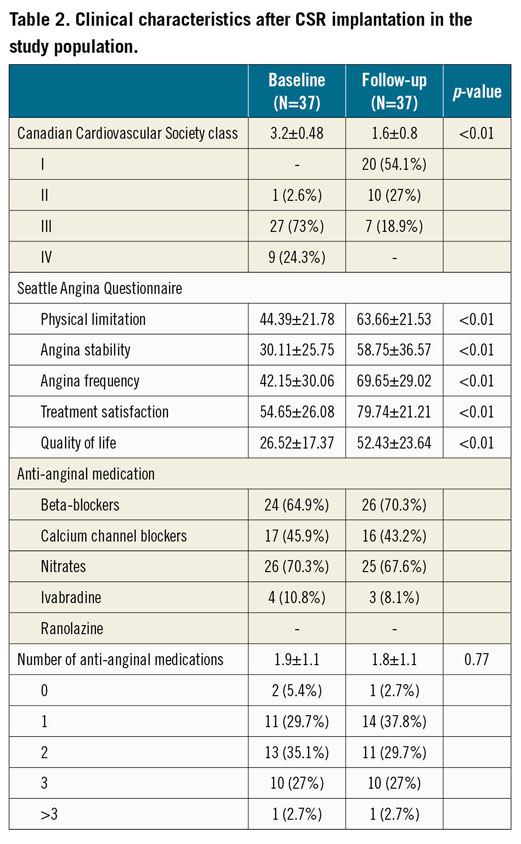
All patients presented at the scheduled six-month follow-up visit. Improvement in angina symptoms was observed in 32 patients (86.5%), with a mean improvement in CCS class at follow-up of 1.6±0.8 (Table 2). As per protocol, only very limited differences in anti-anginal medications were recorded, with a mean of 1.9±1.1 drugs per patient at baseline versus 1.8±1.1 at follow-up (p=0.77) (Table 1, Table 2). In particular, the rate of use of beta-blockers was comparable at baseline and at follow-up. No adverse cardiovascular events were reported during the follow-up period. Baseline and follow-up Seattle Angina Questionnaires for assessment of quality of life were available for 31 patients (84%), showing consistent and significant improvement in all variables of the questionnaire (all p<0.01) (Table 2).
CARDIOPULMONARY EXERCISE TEST (CPET)
All patients performed the CPET with the same protocol at baseline and at six-month follow-up. Full results of the CPETs are shown in Table 3. Both at baseline and at follow-up, the exercise was interrupted due to physical exhaustion in 64% of patients, while the onset of anginal symptoms was the reason for the test interruption in the remaining 36% (p=NS). Significant ST-segment changes suggestive of ischaemia were detected in 43% of baseline CPETs, while 28% were positive at the follow-up test (p=NS).
An overall better performance was observed at follow-up CPET, with significant improvements in terms of exercise workload (+12.9 W [+34%]; 68±28 W at baseline vs 81±49 W at follow-up, p=0.05), VO2 max (+0.97 ml/kg/min [+11.3%]; 12.2±3.6 ml/kg/min at baseline vs 13.2±3.7 ml/kg/min at follow-up, p=0.026) (Figure 1) and VCO2 at AT (0.64±0.29 L/min at baseline vs 0.79±0.24 L/min at follow-up, p=0.04). Of note, improvements in VO2 max and VO2 at AT occurred in 78.4% of patients. An illustrative case of CPET performance at baseline and after CSR implantation is shown in Figure 2.
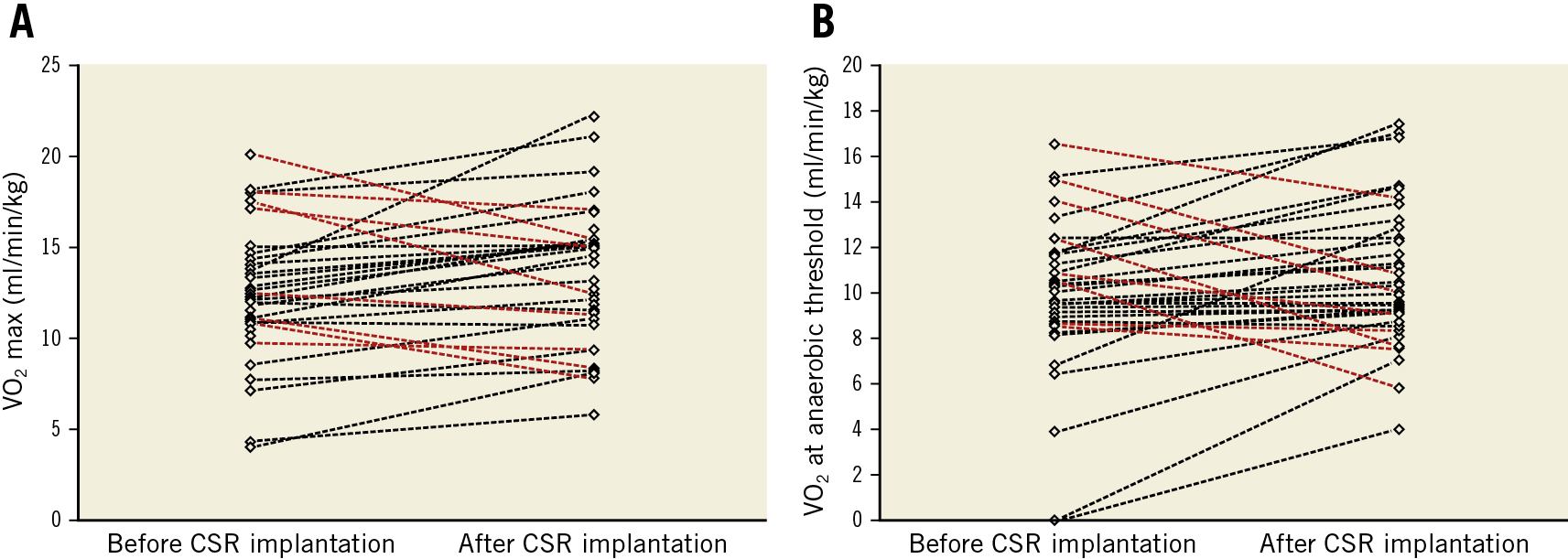
Figure 1. Distribution and improvements of VO2 max (A) and VO2 at AT (B) in the study population, before and after CSR implantation. Red lines indicate patients with lower values of VO2 max or VO2 at AT at follow-up when compared with baseline values, while black lines show the improvements in these parameters.
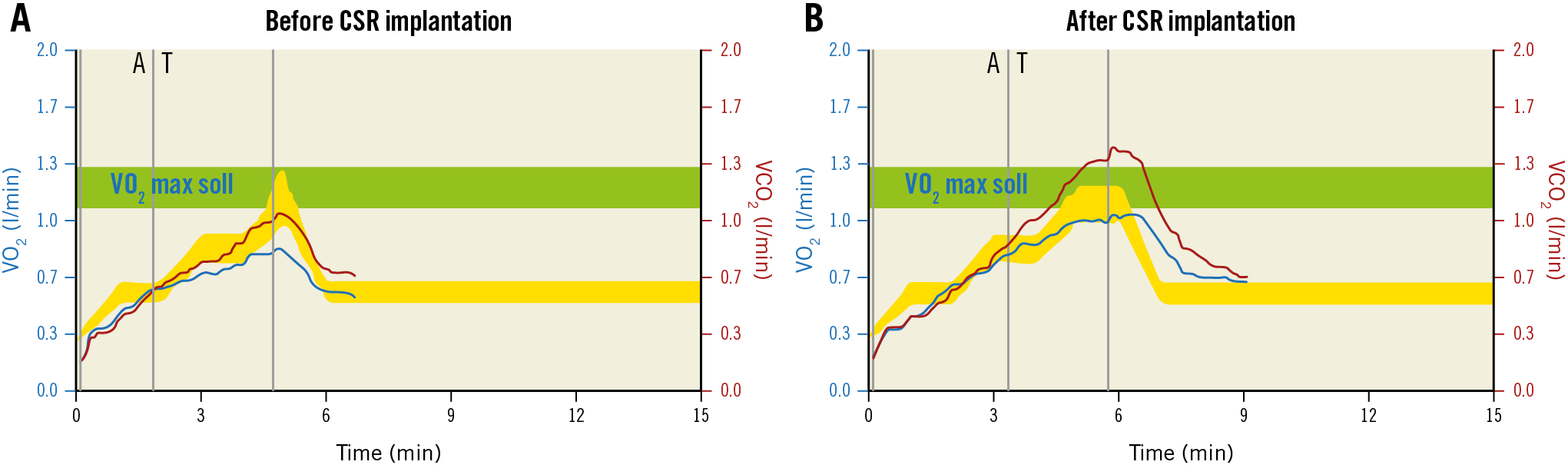
Figure 2. Illustrative cases of CPET before and after CSR implantation. A) Before CSR implantation, with reduced effort tolerance (280 seconds, 52 W), limited VO2 max (14.6 ml/kg/min) and evident change in VO2 slope after the anaerobic threshold, with stable increase in VCO2. This is typical of cardiac limited CPET, where VO2 increases with a stable ΔVO2/ΔWR slope until the myocardium reaches its ischaemic threshold. Then, the ΔVO2/ΔWR slope abruptly decreases while the ΔVCO2/ΔWR slope continues to rise relatively steeply. B) Results from CPET after CSR in the same patient, with slightly higher effort tolerance (342 seconds, 75 W), higher VO2 max (18.1 ml/kg/min) and more physiologic change in VO2 slope. Consistent improvements in CCS class were observed (from CCS IV to CCS I). VO2 max soll: VO2 maximum setpoint
However, improvement in VO2 at AT resulted in being non-significant (9.84±3.4 ml/kg/min vs 10.74±3.05 ml/kg/min, p=0.06). No significant changes were detected for the other parameters in the CPET, including respiratory exchange ratio (Table 3).
CPET IN PATIENTS WITHOUT CLINICAL BENEFITS
A sub-analysis of the CPET outcomes was performed in the four patients who reported lack of CCS improvements at follow-up. Consistently with this, non-significant improvement was observed in VO2 kinetics parameters at follow-up CPET. More specifically, VO2 at AT improved from 9.22±1.99 to 11.2±2.75 ml/kg/min (p=0.07), VO2 max from 11.3±3.11 to 13.22±3.73 ml/kg/min (p=0.11) and workload remained substantially stable (45±20 W vs 46±22 W, p=0.93). All other parameters remained essentially unchanged. An additional sensitivity analysis was performed on responder patients and is presented in Supplementary Appendix 1 and Supplementary Table 1.
Discussion
This is the first report on a significant improvement of CPET parameters supporting an objective reduction in myocardial ischaemia after CSR implantation. Indeed, the increased effort tolerance (exercise workload +34.8% compared with baseline) and the higher VO2 max (+11.3%), together with a borderline non-significantly higher VO2 at AT, support overall improved oxygenation kinetics during maximal effort after CSR implantation. In addition, these benefits are accompanied by consistent improvement in symptoms as expressed by CCS and SAQ assessments. Of note, these results were registered in conditions of stable medical treatment before and after CSR implantation (in particular, with a very high percentage of patients consuming beta-blockers and calcium channel blockers, which explains the submaximal HR observed) (Table 2, Table 3).
Data on the beneficial effects from the “transvenous” treatment of myocardial ischaemia by means of Reducer implantation have been investigated in previous studies. Indeed, increases in SAQ parameters and improvements of CCS class reported in our study are consistent with those of previously published experiences6,7,10. However, the mechanisms of its anti-ischaemia effect remain at least in part unknown. In a physiological study by Ido et al, the authors described a significant increase in regional myocardial blood flow towards more ischaemic subendocardial areas following intermittent occlusion of the CS21. Additional insights supporting reduction in ischaemia after CSR have been provided in the unique investigation by Giannini et al. According to their results, CSR implantation resulted in improved myocardial perfusion in all left ventricle (LV) layers as investigated with cardiac MRI8. Consistent with those findings, we hypothesise that the observed redistribution in flow to the ischaemic myocardium is linked not only to a better perfusion of ischaemic subendocardial area, but also to an overall improved myocardial performance during exercise22,23. This is confirmed by the improvements in VO2 max and VO2 at AT observed during CPET after CSR implantation. VO2 at AT, in particular, is less influenced by patients’ motivation and performance, and may suggest an overall improved condition independently from the maximal exercise reached during a single effort. Ongoing investigations with cardiac MRI after CSR implantation from our group will be able to explore the nature and mechanisms of these reported benefits further.
Furthermore, the improvements we describe here are in line with those historically shown in patients with stable angina undergoing percutaneous revascularisation. In their original investigation, Adachi and colleagues observed a variation in performance at CPET in a population of relatively young patients (average age 55 years) undergoing, mostly, simple single-vessel PCI24. They reported an increase in VO2 max of nearly 14% (from 23.1±3.5 to 26.5±3.2 mL/min/kg), which is similar to the 11.3% observed with the CSR. Of note, the population enrolled in the present study comprises complex patients suffering from refractory angina, of older age (68±9 years old), with a common history of previous multiple myocardial revascularisation procedures (including CABG in almost 75% of cases) and presence of symptoms despite maximised anti-ischaemic medical therapy in the absence of other therapeutic options. For this reason, the increments reported here represent a valuable improvement and have to be considered in the context of a relatively complex pool of patients with advanced coronary artery disease.
Our findings may suggest potentially relevant prognostic implications. In fact, a significant body of evidence has linked the performance at CPET with clinical outcome in patients with chronic heart failure25,26,27,28,29. In a recent article, specific cut-offs of VO2 max have been identified to predict worse clinical outcome (including cardiac death), which varied during the last decades, but constantly showed that a reduction in absolute VO2 max is associated with lower survival30. The effects of physical training on CPET performance were investigated in a study from Hambrecht et al30, where 22 patients with HF and impaired LV function (mean EF 26±9%) were randomised to six months of training programme versus physical inactivity. At six months, patients undergoing physical training showed significant improvements in peak VO2 (+31%, p<0.01 vs control group) and VO2 at AT (+23%, p<0.01 vs control group). Moreover, in the HF-ACTION trial, a dedicated rehabilitation programme was applied to heart failure patients, showing consistent improvement in VO2. Of interest, the exercise training-induced increases in peak VO2 were closely correlated with a better prognosis. For every 6% increase in peak VO2 (+0.9 ml/kg/min), there was an associated 5% lower risk of the primary endpoint (time to all-cause mortality or all-cause hospitalisation, p<0.001) and an associated 8% lower risk of combined cardiovascular mortality and chronic heart failure (CHF) hospitalisations (p<0.001)31. Thus, even a small increase in VO2 max as observed with CPET may translate to clinically significant improvement.
Finally, recent evidence supports possible benefits in diastolic function after CSR implantation14. Diastolic dysfunction has been linked to reduced VO2 max, which appeared to be negatively impacted by increased LV end-diastolic filling pressures32.
Our observations (in particular the average absolute +34.8% increased workload capacity and +0.97 ml/kg/min [+11.3%] in VO2 max) suggest that a significant proportion of patients undergoing CSR implantation also experience a relevant improvement in their general clinical condition, with higher effort tolerance and more physiological oxygen kinetics. A possible reduction in the incidence of adverse cardiac events may therefore be expected, even though this remains, at least at present, only speculative. Dedicated trials – with larger sample sizing and a control group – are needed to confirm these hypotheses.
Limitations
The present study has some limitations that need to be acknowledged. First, this was not a randomised trial, and no control group was available to support the described outcomes and avoid any possible bias in the analysis. No independent and centralised laboratory was commissioned to analyse the CPET data. Another limitation is the relatively small number of patients included in the analysis. A larger cohort of subjects would probably offer additional analysis and, in our view, potentially confirm those increments with borderline statistical significance (such as the improvements in VO2 at AT). In addition, insights on the interaction between anti-ischaemic agents (such as beta-blockers) and CPET outcomes would merit deeper investigation, provided there was a sufficient sample size. In addition, relative new parameters of oxygen kinetics were not available in our analysis33,34. Finally, despite the fact that no specific instruction for any physical rehabilitation programme was given after CSR implantation, a potential impact of any autonomous physical activity performed by the enrolled subjects on the CPET outcome cannot be excluded.
Conclusions
The application of the coronary sinus Reducer in patients with refractory angina is associated with significant clinical benefits and with objective improvements in VO2 kinetics and effort tolerance, as assessed by cardiopulmonary exercise testing. Further dedicated studies are needed to confirm our findings and to assess their impact on long-term clinical outcome.
|
Impact on daily practice Coronary sinus Reducer (CSR) implantation represents an emerging treatment option to reduce symptoms in patients with refractory angina. This is the first description of improved effort tolerance and oxygen kinetics after CSR implantation as assessed with a cardiopulmonary exercise test. CSR implantation should be considered in clinical practice not only to improve the quality of life of patients with refractory symptoms, but also potentially to reduce ischaemic burden and improve clinical conditions. |
Conflict of interest statement
P. Agostoni reports personal fees from Neovasc Inc. S. Verheye is a consultant to and proctor for Neovasc Inc. S. Banai reports personal fees from Neovasc Inc, and being a medical director of Neovasc Inc. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.