A 76 year old man with known ischaemic cardiomyopathy was admitted with refractory heart failure. Cardiac magnetic resonance imaging confirmed severe left ventricular dysfunction with an ejection fraction of 9% (online video) with fully viable myocardium. Coronary angioplasty was performed on a critical lesion in the proximal LAD. Arterial pressure and ECG monitoring prior to angioplasty showed a normal aortic pressure tracing and no ischaemic changes (Figure 1A). Following balloon inflation in the LAD the patient developed marked pulsus alternans with alternating strong and weak beats (arrowheads, Panel B). Alternans of the ST-segment was also evident with mild ST-elevation in alternate beats (arrows, Figure 1B). Pulsus alternans is known to be a manifestation of severe heart failure. Although the mechanism is not fully understood, it is associated with a poor prognosis. Similarly ST-segment alternans may be a marker of severe and extensive myocardial ischaemia, and has been associated with malignant ventricular arrhythmias. The simultaneous development of both phenomena was worrying. These changes persisted even in the absence of symptoms, and accordingly an intra-aortic balloon pump was inserted with normalisation of the ECG and pressure tracing by 24 hours. The patient was successfully discharged one week later.
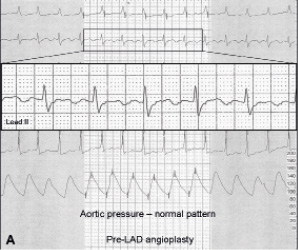
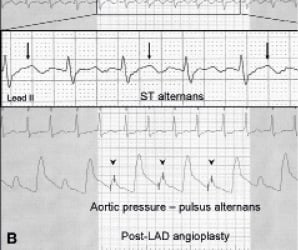
Figure 1. Arterial pressure and ECG monitoring prior (A) and post (B) angioplasty.

